Every year, over 90% of prescriptions filled in the U.S. are for generic drugs. Yet, many patients still ask: "Is this really the same?" And some doctors, despite knowing the science, still reach for the brand-name box.
It’s not about cost alone. It’s not even mostly about cost. It’s about trust - the kind built over years of seeing a familiar name on a pill bottle, the kind that makes patients feel safer. But here’s the truth: generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t need to pay for ads, fancy packaging, or decades of marketing.
What Exactly Makes a Drug "Generic"?
A generic drug contains the exact same active ingredient, in the same strength, and delivered the same way as its brand-name version. That means if you take 10 mg of lisinopril from Walmart or 10 mg of Zestril from the brand, your body absorbs it the same way. The FDA requires this. Not just says it - proves it.
To get approved, a generic must show bioequivalence: the amount of drug in your bloodstream over time must fall within 80% to 125% of the brand’s levels. That’s not a guess. It’s tested in real people using blood samples. The FDA inspects every manufacturing plant - whether it’s in Ohio or India - the same way they inspect Pfizer or Merck. There’s no special lane for generics. No shortcuts.
And yet, people still worry. Why? Because the pills look different. The color is off. The shape is weird. The imprint says "LIS" instead of "ZES." That’s not a mistake. That’s the law. Generic manufacturers can’t copy the exact look of the brand. So they change it. And patients notice. And they panic.
Doctors Know Generics Work. So Why Don’t They Prescribe Them More?
Here’s the contradiction: 96% of Saudi physicians said they understood generics were just as effective. But only 16% said they’d use them in "all" cases. In Greece, half of doctors thought generics were high quality - yet only 25% prescribed them regularly.
It’s not ignorance. It’s habit. It’s fear. Fear that a patient will come back saying, "This isn’t working." Fear that the insurance company pushed it, not the doctor. Fear that if something goes wrong - even if it’s unrelated - they’ll be blamed for switching.
Primary care doctors prescribe generics more than specialists. Why? Because they see the big picture. They know that if a 72-year-old with high blood pressure can’t afford their $350 brand-name pill, they’ll skip doses. Or stop entirely. And then they end up in the ER. That’s not speculation. That’s data. One Canadian study showed ER visits went up 8-14% after switching from brand to generic for blood pressure meds - but the researchers admitted: it wasn’t the drug. It was the disruption. Patients got confused. They thought the change meant something was wrong.
Doctors aren’t resisting generics because they think they’re unsafe. They’re resisting because they’ve seen patients lose trust when the pill changes. And once trust is broken, it’s hard to rebuild.
The Real Cost of Not Using Generics
Brand-name drugs can cost 80-85% more than generics. That’s not a marketing number. That’s the Congressional Budget Office’s estimate. For Medicare Part D alone, if doctors prescribed generics at the same rate they’re filled, the program could save $17.3 billion a year.
But money isn’t the only thing at stake. Adherence is.
Studies show patients taking generics are 6% more likely to stick with their meds than those on brand-name drugs. Why? Because they can afford them. A $4 pill at Walmart beats a $350 one every time. That 6% difference? It translates to a 2.2% drop in hospitalizations for chronic conditions like diabetes, heart disease, and asthma.
One patient told me: "I used to skip my pills every other week because the brand cost too much. Now I take them every day. I feel better. My blood pressure is normal. And I’m not broke." That’s not a clinical trial. That’s real life.
When Generics Might Not Be the Best Fit
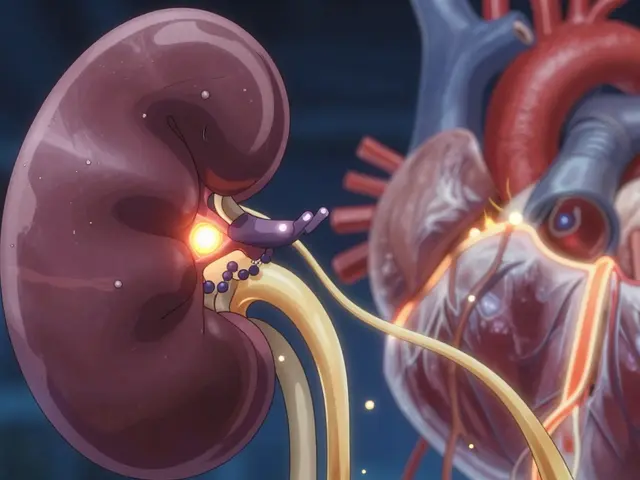
There are exceptions. The FDA keeps a list of 15 drugs with a "narrow therapeutic index" - meaning tiny differences in blood levels can cause big problems. Think warfarin, lithium, or certain seizure meds. For these, switching from brand to generic might need extra monitoring.
And then there are complex drugs - inhalers, topical creams, injectables. A 2015 FDA study found patients with asthma or COPD were unsure if their generic inhaler worked the same. Why? Because the device felt different. The puff didn’t feel right. The dose counter looked odd. It wasn’t the medicine. It was the delivery.
That’s why the FDA launched its "Look Alike Sound Alike" program. It reduces confusion between similar-looking drugs. Since 2018, patient mix-ups have dropped 37%. But education still lags. Many doctors don’t know how to explain these differences to patients.
How to Build Trust - Even When the Pill Looks Different
Patients don’t distrust generics because they’re dumb. They distrust them because no one took the time to explain.
Dr. Sarah Ibrahim from the FDA says: "Patients are more likely to stop taking their generic medications when they experience a change." That’s not about the drug. It’s about the conversation.
Here’s what works:
- Don’t just write "generic" on the script. Say it out loud: "This is the same medicine as your old pill, just cheaper. The active ingredient is identical. The only difference is the color and the name on it."
- Hand them the box. Point to the active ingredient. Show them it matches what they were taking before.
- Don’t assume they know what "bioequivalent" means. Say: "Your body gets the same amount of medicine the same way."
- If they’ve had a bad experience with a generic before, ask why. Was it the side effect? The pill size? The taste? Sometimes it’s the filler, not the active drug.
One internist in Texas said: "I had a patient refuse generic lisinopril because she thought the white pill was fake. I pulled up the FDA’s website on my tablet. Showed her the approval data. She cried. Said she’d been scared for months. She’s been on it for a year now. No issues."
The Future Is Generic - But Only If We Talk About It
By 2030, generics will still make up over 85% of all prescriptions. The market is growing. New biosimilars - generics for biologic drugs like Humira - are coming. They’ll be more complex. More expensive. And even harder to explain.
But here’s the good news: residency programs are catching up. In 2015, only 29% of internal medicine programs taught generic prescribing. Now, it’s 68%. That’s progress.
And patients? When they understand, they choose generics. Medicare beneficiaries using generics report 12.7% higher adherence than those on brand-name drugs. That’s not luck. That’s clarity.
Doctors don’t need to be salespeople. But they do need to be educators. Because when patients believe the pill in their hand is just as good - even if it looks different - they take it. And when they take it, they stay healthy. And that’s the whole point.


Comments (9)
Erika Sta. Maria
So let me get this straight-generic drugs are *exactly* the same, but the pills look different so people think they’re fake? 🤦♀️ Like, if I swapped my iPhone charger for a $2 one that says ‘Made in China’ and it still charges my phone, I’d be thrilled. But pills? Nooo, now we’re in the realm of witchcraft. The real problem isn’t science-it’s that we’ve been conditioned to equate price with purity. And honestly? That’s capitalism’s greatest trick.
Steve Harris
I’ve worked in primary care for 18 years. I’ve seen patients cry because they thought their generic blood pressure med was ‘weak.’ I’ve also seen them sob a year later when they realized they hadn’t had a headache in 11 months because they could finally afford to take it daily. The science is rock solid. The fear? That’s the real epidemic. We need to stop treating patients like they’re dumb and start treating them like people who’ve been lied to by marketing for decades.
Logan Romine
So the FDA says it’s the same… but the pill is a different color??? 😭 I mean, if my antidepressant suddenly turned from blue to neon green, I’d swear I was hallucinating. And that’s the point-our brains are wired to associate *appearance* with *identity*. A generic isn’t just a drug. It’s a psychological identity crisis in a bottle. 🧠💊 #BioequivalenceIsASocialConstruct
Chris Vere
In Nigeria we do not have the luxury of brand name versus generic. Everything is generic. We do not have choice. If it works it is good. If it does not work we go to next. No one has time to cry over pill color. We care about result. If blood pressure goes down then medicine is good. Simple. No drama. No marketing. Just life.
Pravin Manani
The bioequivalence threshold of 80–125% is statistically robust, but it’s worth noting that the pharmacokinetic variability within the same brand over time can exceed that range due to formulation changes, manufacturing shifts, or even batch-to-batch differences. The assumption that brand = consistency is a myth. The real issue is not generics-it’s the lack of transparency in supply chain traceability and the absence of patient-facing pharmacovigilance infrastructure. We’re treating symptoms, not root causes.
Mark Kahn
I had a patient tell me she stopped her generic statin because it ‘didn’t feel right.’ So I gave her a little card with the active ingredient printed on it and a photo of the brand-name pill side by side. She brought it back a month later saying, ‘I didn’t know they were the same thing.’ I cried. Not because she was wrong. Because I wish I’d done this sooner.
Leo Tamisch
Ah yes, the great generic delusion. Let’s ignore the fact that the inactive ingredients can cause reactions in sensitive patients. Let’s ignore that some generics have different dissolution profiles that *do* matter in chronic conditions. And let’s pretend the FDA inspections in India are as rigorous as those in New Jersey. 🤡 Meanwhile, my insurance company is laughing all the way to the bank. ‘It’s the same!’ they say. Yeah. So is a paper airplane and a Boeing 747. Both fly. One just doesn’t crash mid-flight.
Daisy L
I don’t care what the FDA says-my husband’s generic seizure med made him lose his mind for three weeks! He was crying in the shower, yelling at the toaster, thinking the cat was plotting against him. We went back to the brand. He’s fine now. Don’t you DARE tell me ‘it’s the same.’ It’s NOT the same when your husband turns into a zombie because some Indian factory used a different dye. I’m not a scientist-I’m a wife. And I know what I saw.
Anne Nylander
I used to skip my pills too... until i got the generic for $4. now i take them every day. i feel better. my bp is good. i dont cry about the color. i just take it. thank you for writing this. it made me feel less alone.