Cephalosporin Safety Calculator
How Safe Is This Cephalosporin For You?
Based on current medical evidence, the risk of cross-reactivity between penicillin allergies and cephalosporins depends on both the type of penicillin reaction and the specific cephalosporin selected.
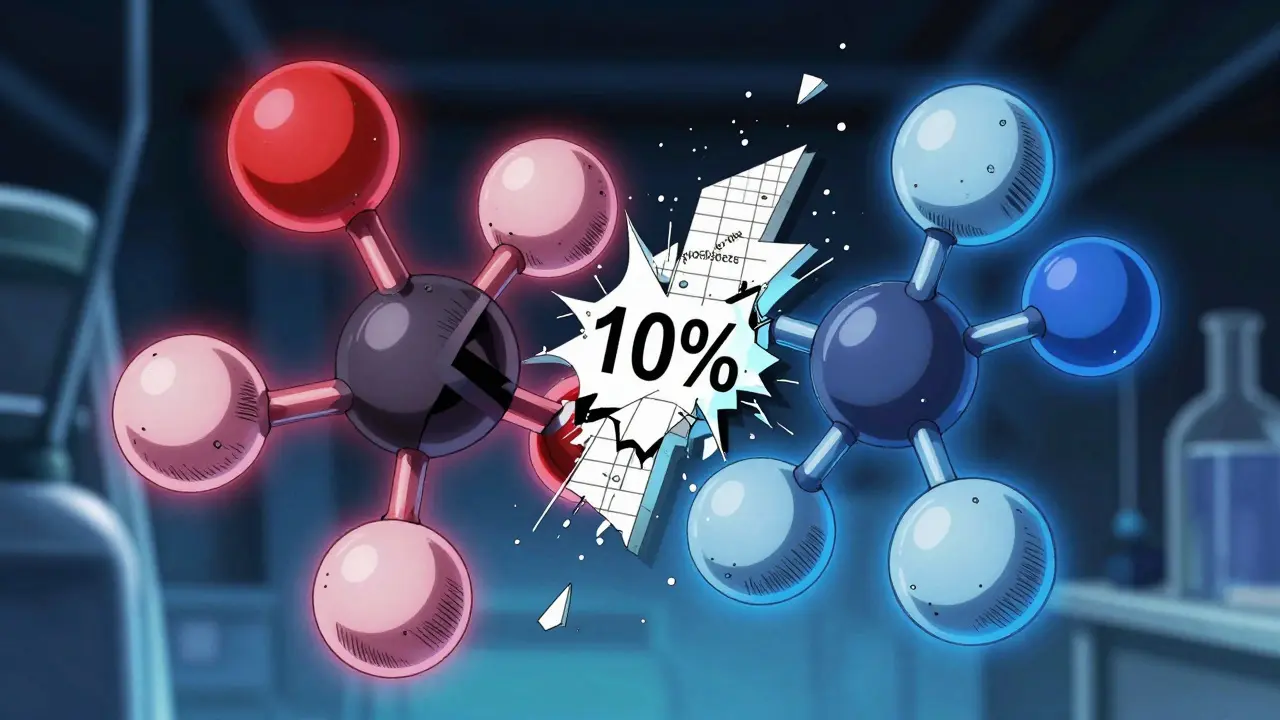
For decades, doctors were told to avoid cephalosporins in patients with penicillin allergies-based on a 10% cross-reactivity rate. But that number is outdated, misleading, and putting patients at greater risk. Today, we know better. The real cross-reactivity between penicillins and cephalosporins is far lower, and the reason has everything to do with side chains-not the beta-lactam ring you’ve heard so much about.
Why the 10% Rule Is Wrong
The 10% cross-reactivity figure comes from studies done in the 1960s and 70s. Back then, cephalosporin production wasn’t clean. The mold used to make these drugs, Cephalosporium, often had traces of penicillin left behind. So when patients reacted to cephalosporins, it wasn’t because the drugs were structurally similar-it was because they were contaminated. Modern manufacturing has eliminated this issue. Today’s cephalosporins are pure. And when you remove the contamination factor, the real cross-reactivity rate drops to 2-5% for first- and second-generation cephalosporins, and under 1% for third- and fourth-generation ones.The Side-Chain Hypothesis: What Actually Matters
The beta-lactam ring is what makes penicillins and cephalosporins part of the same antibiotic family. But it’s not what triggers allergies. The real culprit? The side chains-the chemical groups hanging off the main structure. Think of it like this: two cars might have the same engine, but if one has a red spoiler and the other has a blue one, they’re not the same to a cop who’s looking for the red one. In penicillin allergies, 42% to 92% of immune reactions are tied to the side chain, not the ring. Cephalosporins have two side chains: R1 and R2. The R1 side chain is the big player in triggering immune responses. The R2 chain? It falls off when the drug breaks down in the body, so it doesn’t matter much. That’s why ceftriaxone and cefotaxime (third-generation) are so safe in penicillin-allergic patients-they have completely different R1 side chains than penicillin G or amoxicillin.Generations Matter: Which Cephalosporins Are Riskier?
Not all cephalosporins are created equal. Here’s how they stack up:| Generation | Examples | Approx. Cross-Reactivity with Penicillin | Side-Chain Similarity to Penicillin |
|---|---|---|---|
| First | Cefazolin, Cephalexin | 1%-8% | High |
| Second | Cefuroxime, Cefaclor | 1%-5% | Moderate |
| Third | Ceftriaxone, Cefotaxime, Cefixime | <1% | Low |
| Fourth | Cefepime | <1% | Very Low |
| Newer Agents | Ceftolozane/tazobactam | Unknown (likely low) | Distinct |
First-generation cephalosporins like cefazolin have side chains that look a lot like those in penicillin V or ampicillin. That’s why they carry the highest risk. But ceftriaxone? Its side chain is completely different. Studies show zero anaphylaxis cases in over 3,300 penicillin-allergic patients given ceftriaxone-even though many of them had reported allergies. The same goes for cefepime. These aren’t just safer-they’re often the best choice for treating serious infections like meningitis or complicated UTIs.

What About Anaphylaxis? Is It Really That Rare?
Yes. Anaphylaxis from cephalosporins in penicillin-allergic patients is extremely rare. The CDC estimates it happens in about one out of every 52,000 cases. In a major study from Kaiser Permanente, researchers gave cephalosporins to over 3,300 patients who claimed they were allergic to them. Most got first-generation drugs. Zero cases of anaphylaxis. Not one. This suggests that many people who say they’re allergic to penicillin aren’t truly allergic at all. They might’ve had a rash as a kid, or nausea after taking the drug, or just heard someone say they were allergic. True IgE-mediated allergies-hives, swelling, trouble breathing-only happen in a small fraction of people who report penicillin allergy. And even among those, the risk of reacting to a third-gen cephalosporin is negligible.When Is It Safe to Use Cephalosporins?
The CDC and Infectious Diseases Society of America agree: if a patient has no history of IgE-mediated reactions (anaphylaxis, hives, swelling, wheezing) to penicillin in the last 10 years, it’s safe to use third- or fourth-generation cephalosporins. No skin test needed. No waiting. No unnecessary delays. But here’s the catch: if someone had a true anaphylactic reaction to penicillin, you still need to be careful. For those patients, avoid first-generation cephalosporins. If you must use a cephalosporin, pick one with a very different side chain-ceftriaxone or cefepime. And if you’re unsure, do a skin test with the specific cephalosporin you plan to use. Skin testing for cephalosporins isn’t routine everywhere, but it’s growing. And when done right, it’s accurate.Why This Matters More Than You Think
Over 10% of people in the U.S. say they’re allergic to penicillin. That’s over 30 million people. But 90-95% of them aren’t truly allergic. And because doctors still believe the old 10% myth, they avoid all beta-lactams-penicillins AND cephalosporins. That means patients get clindamycin, vancomycin, or fluoroquinolones instead. Those alternatives are worse. They’re broader-spectrum. They wipe out good bacteria. They increase the risk of Clostridioides difficile infections-deadly, hard-to-treat diarrhea that can land you in the hospital for weeks. They also drive antibiotic resistance. One study showed that hospitals with penicillin allergy delabeling programs cut broad-spectrum antibiotic use by 10-25% and shortened hospital stays by 1-2 days. This isn’t just about avoiding a rash. It’s about saving lives, reducing costs, and fighting superbugs.
What’s Holding Back Change?
The FDA still lists a 10% cross-reactivity warning on cephalosporin labels. That’s based on 50-year-old data. Meanwhile, the CDC, Medsafe (New Zealand’s drug regulator), and major medical societies have updated their guidelines to reflect the science. But because the FDA’s label stays the same, many doctors still play it safe-out of fear of liability, not science. Add to that: 80-90% of clinicians still believe the 10% myth. Medical schools haven’t caught up. Electronic health records still flag all cephalosporins as high-risk for penicillin-allergic patients. It’s a systemic problem.What You Can Do
If you or someone you know has a penicillin allergy label:- Ask: Was this a true allergic reaction-or just a side effect? Rashes, nausea, or headaches aren’t allergies.
- Ask: Can I get tested? Penicillin skin testing is safe, quick, and available in most hospitals and allergy clinics.
- If you need an antibiotic and are told cephalosporins are off-limits, ask: Which one? Is it first-gen? Could we use ceftriaxone instead?
Even if you’ve never been tested, if your allergy was mild or happened over 10 years ago, the risk of reacting to a third-gen cephalosporin is lower than the risk of taking a worse antibiotic.
What’s Next?
Researchers are now mapping exact side-chain structures to predict which combinations are safe. New drugs like ceftolozane/tazobactam don’t fit into old categories, so we need better tools. Some hospitals are starting automated alerts in their EHRs that pop up when a penicillin-allergic patient is prescribed a broad-spectrum antibiotic-suggesting a safer cephalosporin instead. The future is precision: not avoiding all beta-lactams, but choosing the right one based on chemistry, not fear.Can I take ceftriaxone if I’m allergic to penicillin?
Yes, in most cases. Third-generation cephalosporins like ceftriaxone have a cross-reactivity rate of less than 1% with penicillin-allergic patients. This is especially true if your penicillin allergy was not IgE-mediated (no anaphylaxis, hives, or swelling). The CDC and major medical societies consider ceftriaxone safe for patients with a history of penicillin allergy who haven’t had a severe reaction in the past 10 years.
Are all cephalosporins unsafe if I’m allergic to penicillin?
No. First-generation cephalosporins like cefazolin and cephalexin have a higher risk-up to 8%-because their side chains resemble penicillin’s. But third- and fourth-generation cephalosporins like ceftriaxone and cefepime have very different side chains and carry almost no risk. The key is matching the drug to the side-chain structure, not avoiding the whole class.
I had a rash after penicillin. Does that mean I’m allergic?
Not necessarily. Many people mistake side effects for allergies. A mild rash that appears days after taking penicillin is often a non-allergic reaction. True penicillin allergies involve hives, swelling, trouble breathing, or anaphylaxis-usually within minutes to hours. If you’re unsure, ask about penicillin skin testing. It can confirm whether you’re truly allergic or not.
Why do some doctors still avoid cephalosporins for penicillin-allergic patients?
Because outdated information is still in drug labels and medical training. The FDA’s labeling hasn’t changed since the 1970s, even though modern evidence shows cross-reactivity is far lower. Many clinicians were taught the 10% rule and haven’t updated their knowledge. Hospitals are slowly changing, but progress is uneven.
What’s the safest alternative if I can’t take any cephalosporins?
If you have a confirmed IgE-mediated penicillin allergy and need an antibiotic, options include azithromycin, doxycycline, or vancomycin-depending on the infection. But before choosing these, consider getting tested. Many people who think they can’t take penicillins or cephalosporins actually can. Avoiding beta-lactams unnecessarily increases your risk of antibiotic-resistant infections and C. diff.