
By the time you pick up your prescription at the pharmacy, there’s a better than 90% chance you’re holding a generic drug. It’s not just common-it’s the backbone of how Americans afford their medicines. But this wasn’t always the case. For most of the 20th century, brand-name drugs dominated. The shift to generics didn’t happen by accident. It took decades of broken safety laws, deadly scandals, political battles, and one landmark law that changed everything.
The First Steps Toward Drug Standards
Long before the FDA existed, Americans had no way to know if the medicine they bought was real. In 1820, eleven doctors met in Washington, D.C., and created the first U.S. Pharmacopeia-a list of standard drug formulas. Their goal? To stop pharmacists from selling fake or weak medicines. It was a start, but not enough. By the 1840s, imported drugs were often contaminated. The 1848 Drug Importation Act gave U.S. Customs the power to block bad drugs at the border. Still, there was no law forcing manufacturers to prove what was inside their bottles.In 1888, the American Pharmaceutical Association published the National Formulary, another attempt to standardize drug quality. But without enforcement, counterfeiters kept thriving. The real turning point came in 1906, when President Theodore Roosevelt signed the Federal Food and Drugs Act. For the first time, labels had to list ingredients. If a drug was misbranded or adulterated, the government could act. This law didn’t require drugs to be safe or effective-it just made lying on the label illegal. But it laid the foundation for the modern FDA.
Deadly Mistakes Force Change
The 1937 Elixir Sulfanilamide disaster changed everything. A pharmaceutical company dissolved a new antibiotic in diethylene glycol-a toxic antifreeze ingredient-and sold it as a sweet liquid for children. Over 100 people died, mostly kids. Public outrage forced Congress to act. In 1938, the Federal Food, Drug, and Cosmetic Act (FDCA) was passed. For the first time, drugmakers had to prove their products were safe before selling them. The FDA gained real power. But there was still a loophole: companies didn’t need to prove their drugs actually worked.That changed in 1962. The Kefauver-Harris Drug Amendments required proof of both safety and effectiveness. Before this, drugs like thalidomide (which caused severe birth defects in Europe) could have slipped through U.S. approval. The law also forced drugmakers to submit data on every drug on the market since 1938. Thousands of drugs were reviewed. Many were pulled. The FDA became a true gatekeeper.
Why Generic Drugs Were Still Rare
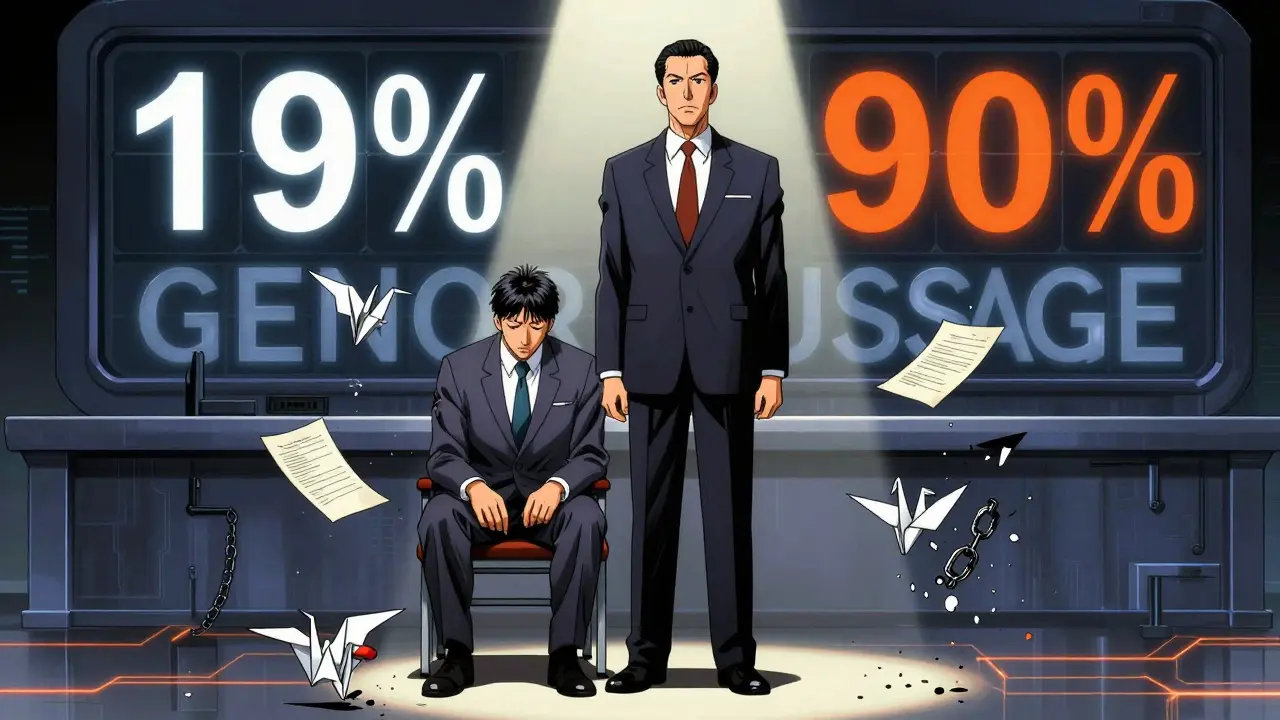
Even after 1962, generic drugs made up only about 19% of prescriptions. Why? Because brand-name companies held patents and kept prices high. Generic manufacturers couldn’t just copy a drug. They had to run full clinical trials-just like the original maker. That cost millions. Few companies could afford it. And even if they did, brand-name companies used legal tricks to block them. The system was stacked against competition.Then came Medicaid and Medicare in 1965. Suddenly, the federal government was paying for millions of prescriptions. They didn’t want to overpay. Officials started asking: Why buy the expensive brand when a cheaper version does the same thing? But without a legal path, generics couldn’t enter the market. That changed in 1984.
The Hatch-Waxman Act: The Game Changer
The Drug Price Competition and Patent Term Restoration Act-better known as the Hatch-Waxman Act-was passed in 1984. It was a compromise. Brand-name companies got extended patent life to make up for time lost during FDA review. In return, generic makers got a new, faster approval path called the Abbreviated New Drug Application (ANDA).Before Hatch-Waxman, generics had to prove safety and effectiveness through full clinical trials. After? They only had to show they were bioequivalent-meaning they delivered the same amount of active ingredient into the bloodstream at the same rate as the brand. No more repeating expensive human trials. No more waiting a decade to enter the market. The law also created a 180-day exclusivity period for the first generic company to challenge a patent, giving them a financial head start.
The results were immediate. Generic drug use jumped from 19% in 1984 to over 50% by the late 1990s. Today, it’s 90.5%. That’s more than 4 billion prescriptions a year filled with generics.
How Much Have Generics Saved?
The savings are staggering. In 2021 alone, generic drugs saved the U.S. healthcare system $373 billion. Over the last decade, that adds up to more than $3.7 trillion. The Congressional Budget Office found generics cut prescription costs by 80-85% compared to brand names. Yet they make up only 23.4% of total drug spending. That’s the power of competition.Take a common drug like lisinopril, used for high blood pressure. The brand version, Zestril, cost over $100 a month in the early 2000s. Today, the generic version costs less than $5. Same active ingredient. Same effect. Same side effects. But the price dropped because five different companies now make it.

The Dark Side of Success
But it’s not all smooth sailing. As generics became the norm, new problems emerged. Between 2018 and 2022, the FDA recorded 1,234 drug shortages. Two-thirds of them involved generic drugs. Why? Because many generics are made overseas-80% of active pharmaceutical ingredient (API) facilities are in China and India. When a factory in India gets shut down for quality violations, or a shipment gets delayed, patients in the U.S. can’t get their medicine.Another issue: price spikes. While most generics got cheaper, about 15% of them saw price increases over 100% between 2013 and 2017. Why? Because if only one company makes a drug, and that company owns the only factory that can produce it, they can raise prices with little pushback. Some drugs, like doxycycline or nitrofurantoin, have been known to jump from $20 a month to $2,000 overnight.
Brand-name companies also found ways to delay generics. One tactic? Refusing to sell samples of their drug to generic makers so they can’t run the required bioequivalence tests. The 2019 CREATES Act was passed to stop this. As of 2022, the FDA had taken 27 enforcement actions under the law.
Modern Challenges and the Future
The FDA launched the Generic Initiative for Value and Efficiency (GIVE) in 2007 to clear backlogs. Then came GDUFA-the Generic Drug User Fee Amendments-in 2012. Now, the FDA reviews ANDAs in about 10 months, down from 30. Approval rates jumped from 45% to 95%. The system works better than ever.But the next frontier is biosimilars-generic versions of complex biologic drugs like Humira or Enbrel. These aren’t simple pills. They’re made from living cells. Getting approval is harder. But the market is growing. Analysts predict biosimilars will be the next big wave of savings, potentially cutting costs by 80% for drugs that currently cost over $100,000 a year.
Right now, the FDA oversees more than 22,000 generic products and 13,000 manufacturing sites worldwide. About 900 new ANDAs get approved each year. The goal? Keep prices low, supply steady, and quality high. It’s not perfect. But without the history of bad laws, deadly mistakes, and hard-won reforms, none of this would exist.
What’s Next?
The U.S. generic drug system is one of the most successful public health policies in modern history. It’s not just about saving money-it’s about access. Millions of people rely on generics to take their heart medication, antibiotics, insulin, and antidepressants. Without them, many would skip doses or go without.The future depends on three things: keeping supply chains secure, preventing price gouging, and making sure new players can enter the market. If those hold, generics will keep saving lives-and billions-for decades to come.


Comments (13)
Winni Victor
So let me get this straight-we let Big Pharma poison kids with antifreeze-laced syrup, then acted shocked when people died? And now we pat ourselves on the back for letting Indian factories make our heart meds? I mean, cool, I get my lisinopril for $3, but I also know the guy who made it probably sleeps in a room with rats and no AC. We’re not saving money-we’re just exporting our moral decay.
Also, why does every single generic drug commercial have that one guy jogging in slow motion with a golden retriever? Like, is that the new American dream? Surviving on pills made by strangers in a country we’ve never heard of until our insurance won’t cover the brand?
I miss when drugs came in glass bottles with handwritten labels. At least then you knew someone had touched it with human hands.
And don’t even get me started on the ‘bioequivalent’ nonsense. My cousin took a generic version of his antidepressant and started crying during a Walmart commercial. Coincidence? I think not.
Also, why does the FDA have 13,000 manufacturing sites but still can’t stop a single factory in India from shipping out moldy capsules? Someone’s getting paid to look the other way. And it ain’t me.
Someone’s gotta say it: we didn’t fix the system. We just got better at ignoring it.
Also, why do we still call them ‘generics’? That’s not a name, that’s a euphemism for ‘whatever’s cheapest this week.’
My grandma took the same pill for 40 years. It was a white oval. Now it’s a blue triangle with a weird logo. Same active ingredient? Sure. But my grandma cried because it didn’t ‘feel right.’ And honestly? Maybe she was onto something.
Next up: generic oxygen. You know, the kind that’s ‘bioequivalent’ to the air we used to breathe before corporations monetized it.
Oh wait. They already did that. It’s called ‘premium air’ on Amazon. $19.99 a can. With a 5-star review from someone who ‘felt more alive.’
God help us all.
Linda B.
The FDA is a puppet of the pharmaceutical industry and the real reason generics are so prevalent is because the government has been quietly replacing American manufacturing with foreign labs that don’t follow our laws and the reason they don’t audit them properly is because the same people who write the regulations are the ones who used to work for Pfizer and Merck and they get paid millions to look the other way and the whole thing is a controlled demolition of American healthcare and you think you’re saving money but you’re actually being poisoned slowly and the pills you take are made by people who don’t speak English and the inspectors who sign off on them are paid in cash and the FDA’s own reports show that 68 percent of violations go uncorrected and you’re not getting a cheaper pill you’re getting a gamble and the real drug is still being made in Ohio but they’re not allowed to sell it because the patents are locked up by shell companies and the whole system is designed to make you dependent on something that might kill you and you’re celebrating this like it’s progressit’s not progress it’s surrender
Oluwatosin Ayodele
Let me tell you something about India and China’s role in this. They dominate because they have cheap labor, no environmental regulations, and zero accountability. But here’s the truth: they’re also the only reason millions of Americans aren’t dying from untreated hypertension. The system is broken, yes. But the alternative? No medicine at all. You want to blame the factories? Fine. But first, ask why your government lets drug companies charge $1,000 for a pill that costs $0.50 to make. The real villain isn’t the factory in Hyderabad-it’s the lobbyist in D.C. who wrote the law that lets them do it.
And before you say ‘buy American’-tell me where you’re going to source active pharmaceutical ingredients if you shut down 80% of the supply chain overnight. The U.S. doesn’t have the infrastructure. We outsourced it because it was cheaper. Now we’re mad we’re dependent? That’s not hypocrisy. That’s just laziness.
Jason Jasper
I appreciate how much thought went into this post. It’s easy to get angry about drug prices, but the history here is actually kind of beautiful in a tragic way. We went from no standards to death by antifreeze to a system that lets someone with diabetes pay $5 for insulin instead of $300. That’s not perfect, but it’s progress.
The real problem isn’t the generics-it’s the lack of price transparency and the fact that insurance companies don’t always pass savings on. And yeah, supply chain issues are terrifying. But I think the solution isn’t to scrap the system-it’s to fix the parts that are broken. More audits. More domestic API capacity. Better incentives for multiple manufacturers to make the same drug.
Generics saved my dad’s life. I don’t want to lose that. I just want to make sure the next generation doesn’t have to worry about whether their pill will arrive next week-or if it’ll be a different color than last month.
Mussin Machhour
Yo this is wild. I had no idea generics were this big of a deal. I just thought they were cheaper versions of the same thing. But now I’m like… holy crap, we’re literally living off a 1984 law that was a compromise between pharma giants and the public. That’s insane.
And the fact that a single factory shutdown can make your blood pressure med disappear? That’s not healthcare. That’s a game of Jenga with people’s lives.
Also, 90% of prescriptions are generic? That’s like saying 90% of your Netflix shows are fan edits. You still get the story, but you know someone else made it cheaper.
But hey-at least I’m not paying $120 for lisinopril anymore. I’ll take the blue pill with the weird logo over the $100 brand any day. Just… please don’t let it run out.
Carlos Narvaez
Post hoc ergo propter hoc fallacy abounds. The Hatch-Waxman Act did not create value. It merely redistributed rent. The real innovation was the commodification of biological efficacy through bioequivalence metrics-a reductionist triumph of regulatory engineering over pharmacological nuance.
And yet, the consumer remains blissfully unaware that ‘same active ingredient’ is a legal fiction. The excipients? Unregulated. The dissolution profile? Approximated. The bioavailability curve? Interpolated.
One does not simply ‘equivalent’ a molecule. One manipulates its context.
And you call this progress?
It is merely efficiency. And efficiency is the last refuge of the morally bankrupt.
Harbans Singh
As someone from India, I’ve seen how these factories operate. Yes, some are sketchy. But many are world-class. My cousin works at a plant in Gujarat that exports to the U.S. and Europe. They have ISO certifications, clean rooms, and auditors from the FDA visiting twice a year.
The problem isn’t the country-it’s the lack of oversight on the *buying* side. Why don’t we require every batch to be tested before it enters the U.S.? Why is the FDA relying on paperwork instead of random testing?
Also, the price spikes? That’s not because of manufacturing-it’s because of consolidation. When only 2 companies make a drug, and one shuts down, the other hikes prices. That’s capitalism, not globalization.
We need more manufacturers. Not less. And we need to stop pretending this is a ‘foreign problem.’ It’s an American policy failure.
Justin James
Here’s what they don’t tell you: the FDA’s entire approval system for generics is a front. The bioequivalence tests? They’re done in labs owned by the same companies that make the drugs. The samples? Hand-delivered by pharma reps. The data? Curated. The audits? Scheduled weeks in advance.
And the real kicker? The 180-day exclusivity period? That’s not a reward-it’s a bribe. The first generic company to challenge a patent gets to be the only one selling for half a year. So they don’t actually lower prices-they *raise* them to max profit before the others show up.
And the patents they challenge? Most of them are junk patents. Ever heard of ‘evergreening’? That’s when they tweak a pill’s coating or shape and get a new 20-year patent. That’s how they block generics for 30 years.
And the government? They’re in on it. The Hatch-Waxman Act wasn’t meant to help patients. It was meant to *manage* the crisis after the Elixir Sulfanilamide scandal. So they gave the public a placebo: cheaper pills. But the real control? Still in the hands of the same corporations.
And now we’re dependent on pills made in countries that don’t even have freedom of speech. That’s not healthcare. That’s hostage-taking.
And the biosimilars? Don’t get me started. They’re just the next step toward replacing medicine with algorithmic substitution. Soon, your insulin won’t be made by a lab. It’ll be made by a bot in Bangalore approved by a bureaucrat in D.C. who got his job because his dad donated to the right PAC.
We’re not saving money. We’re surrendering our health to a system designed to make us feel safe while quietly killing us.
Rick Kimberly
It is worth noting that the Federal Food and Drugs Act of 1906 was a landmark in consumer protection, yet it was fundamentally reactive rather than proactive. The 1938 FDCA, however, represented the first true assertion of federal authority over therapeutic efficacy as a public good. The Kefauver-Harris Amendments further institutionalized the principle that safety and efficacy are inseparable from market access.
That the Hatch-Waxman Act succeeded in expanding market competition without compromising quality speaks to the elegance of the ANDA framework. Bioequivalence, properly defined and rigorously tested, is not a loophole-it is a scientifically valid proxy for therapeutic equivalence.
That said, the persistent shortages and price volatility underscore the fragility of supply chain governance. A centralized, federally funded API reserve should be established. The precedent exists in the Strategic National Stockpile. Why not for essential medicines?
And while I acknowledge the concerns regarding foreign manufacturing, to dismiss the entire system because of geopolitical risk is to ignore the empirical reality: generics have saved trillions and enabled access for millions who would otherwise be untreated.
Progress is not perfection. But it is real.
Terry Free
So let me get this straight-you’re proud that we outsourced our medicine to China and India because it’s cheaper? That’s not progress. That’s surrender. You think you’re saving money? You’re just letting your life depend on people who don’t speak your language, follow your laws, or care about your kids.
And don’t tell me about ‘bioequivalence.’ That’s corporate jargon for ‘we didn’t test it enough.’
My neighbor’s dad died because his generic blood thinner didn’t work right. The label said it was the same. It wasn’t.
And now you’re talking about biosimilars? Like we need more of this? We need to bring manufacturing home. Not more loopholes. Not more ‘efficiency.’ Just… stop selling our health to the lowest bidder.
And if you’re okay with this? You’re part of the problem.
sagar patel
Generics work. I take them. I’ve been on the same one for seven years. No issues. Stop overthinking it. The system isn’t perfect but it’s better than nothing. The people who complain about this are the same people who think organic kale will cure cancer. Just take your pill and be grateful.
Christopher King
They told us the system was fixed. But it’s not. It’s a house of cards made of patents, foreign factories, and silent FDA inspectors who get paid in stock options. And the real horror? The people who need these drugs the most-low-income, elderly, disabled-are the ones who can’t even *see* the danger. They just take the pill. They don’t know it might be made in a building with no running water. They don’t know the company that made it paid a bribe to get the FDA stamp. They don’t know that the ‘bioequivalent’ version might have a different salt form that makes it less effective in people with kidney disease. And yet we celebrate this as progress?
This isn’t healthcare. This is a dystopian simulation where the only thing more expensive than the drug is the truth.
And the worst part? We’re all complicit. We click ‘buy now’ without asking where it came from. We don’t call our reps. We don’t protest. We just take the pill. And hope.
But I’m not hopeful. I’m furious.
And if you’re not? You’re not paying attention.
Winni Victor
Wait-you guys really think the FDA’s ‘10-month review time’ is progress? That’s just a fancy way of saying they’re rushing approvals to meet corporate deadlines. Remember when they approved a generic version of a blood thinner that turned out to have 20% less active ingredient? It took *two years* to recall it. Two years. People died. And the company? Paid a fine and moved on.
And now you’re telling me we’re proud of how fast they approve stuff?
Speed isn’t safety. It’s just faster failure.
Also-why does every generic drug look different? Same pill, different color, different shape, different logo. It’s like the FDA is running a drug roulette game and we’re the suckers betting our lives on it.
And don’t get me started on the ‘first generic to challenge patent’ loophole. That’s not competition. That’s a monopoly auction.
Someone needs to start a movement: ‘Bring Back the White Pill.’