
How FDA Facility Inspections Keep Your Medicines and Devices Safe
If you’ve ever taken a prescription pill, used an insulin pump, or had a pacemaker implanted, you’re relying on a system that checks every step of how those products are made. The U.S. Food and Drug Administration doesn’t just approve drugs and devices - it watches over the factories where they’re produced. Every year, FDA inspectors show up at about 13,000 facilities across the U.S. and around the world. These aren’t surprise visits for fun. They’re legal, detailed, and often life-or-death evaluations of whether a company follows the rules to make safe, effective products.
It’s not enough to say a company follows the rules. The FDA needs proof. That’s why inspections exist - as a real-world check on paper claims. A company might say its staff are trained, its machines are calibrated, and its records are perfect. But inspectors don’t take words for it. They walk the floors, ask questions, pull files, and look for the tiny gaps that can lead to big problems: contaminated medicine, faulty devices, or data that doesn’t add up.
The Four Types of FDA Inspections and When They Happen
Not all FDA inspections are the same. The agency uses four distinct types, each serving a different purpose in the quality chain.
- Pre-approval inspections happen before a new drug or device gets final approval. If a company submits a new product application, the FDA will send inspectors to the manufacturing site within 30 days of saying the facility is ready. This isn’t a formality - it’s a gate. If the inspection finds major issues, the product won’t be approved, no matter how good the science looks on paper.
- Routine surveillance inspections are scheduled every 2 to 5 years, depending on risk. A factory making low-risk dietary supplements might go 5 years between visits. A plant making injectable cancer drugs? That one gets checked every 6 to 12 months. The decision isn’t random. It’s based on a risk model using 12 specific factors like past violations, product complexity, and patient safety impact.
- Compliance follow-up inspections come after a company gets an FDA Form 483 - the official list of problems found during a previous visit. The company has 15 working days to respond with a plan to fix each issue. If the FDA doesn’t believe the plan is strong enough, or if the fixes aren’t done, inspectors come back. Sometimes within months.
- For-cause inspections are triggered by red flags: a spike in patient complaints, a whistleblower tip, a product recall, or a pattern of adverse events. These can happen with no notice at all. A company might be going about its day when an FDA team walks in, credentials in hand, ready to investigate.
Each type of inspection follows the same basic structure: notice (unless it’s for-cause), on-site visit, documentation review, interviews, and a final report. But the stakes change with the type. A pre-approval inspection can kill a product launch. A for-cause inspection can shut down a factory.
What Happens During an FDA Inspection
When the inspectors arrive, they don’t just start asking questions. First, they hand over FDA Form 482 - the official Notice of Inspection. This isn’t optional. It’s required by law. The facility must have someone assigned to accompany them the whole time.
The inspection usually lasts 3 to 10 days. It’s not a tour. It’s an audit with boots on the ground. Inspectors do four things:
- Walk the facility. They look at cleanliness, equipment condition, storage conditions, and whether there’s a clear separation between clean and dirty areas. One common issue? Dust buildup on machinery or unmarked containers. Sounds small? It’s not. Contamination risks start here.
- Review documents. This is where most problems are found. They ask for records like: deviation reports, batch records, equipment calibration logs, validation studies, training files, and change control logs. The FDA doesn’t want summaries - they want the original, signed, dated paperwork.
- Interview staff. They pick people at random - from the machine operator to the quality manager - and ask simple questions: “What do you do if a batch fails?” or “How do you know this machine is calibrated?” Inconsistent answers are a red flag. It suggests training is patchy or people aren’t following procedures.
- Collect samples. If something looks off - a strange odor, discolored product, or mismatched labels - inspectors can take samples for lab testing. That can lead to a recall or worse.
The most common findings? Documentation gaps. A 2024 analysis of over 2,400 inspection reports showed that 78% of observations came from just four areas: incomplete investigations of deviations (32%), missing training records (24%), poor validation documentation (15%), and weak change control systems (7%).
Why Data Integrity Is the Biggest Threat Today
In 2020, data integrity issues made up 28% of FDA inspection observations. By 2023, that number jumped to 45%. Why? Because more companies are using electronic systems - and many aren’t ready.
Data integrity means records are accurate, complete, and trustworthy from the moment they’re created. It’s not just about typing the right number into a computer. It’s about who can edit it, when, and why. The FDA now looks for:
- System access controls - are only authorized people allowed to enter data?
- Audit trails - can you see who changed a record and when?
- Backups - are records preserved in case of system failure?
- Validation - has the software been tested to prove it works as intended?
One common violation: a lab technician manually writes a result on a sticky note, then types it into the system later. That’s not data integrity. That’s a recipe for error. Another: deleting a failed test result and re-running the test until it passes - then only keeping the “good” one. That’s fraud. And the FDA’s new AI tools, launching in late 2024, are designed to spot these patterns automatically.
How Companies Actually Prepare - And What Works
Some companies panic when they hear “FDA inspection.” Others treat it like a routine audit. The difference? Preparation.
Facilities with formal inspection readiness programs see 63% fewer observations than those without. What do they do differently?
- Quarterly mock inspections. They simulate real inspections with internal teams acting as FDA investigators. This isn’t a drill - it’s a live test. They pull files, interview staff, and give feedback.
- A single inspection coordinator. Instead of five people fielding calls, one person manages all communication. This avoids mixed messages. A 2023 survey found 83% of companies with one point of contact had smoother inspections.
- A dedicated inspection room. Equipped with printers, computers, phones, and organized document folders. One company cut document retrieval time by 40% just by having this space ready.
- Updated facility diagrams. If a machine moves, the diagram changes - within 7 days. Inspectors notice if the floor plan on paper doesn’t match the floor in front of them. It erodes trust fast.
Training matters too. FDA guidance says staff who interact with inspectors need 8 hours of training per year. Principal investigators need 16. But only 63% of clinical sites meet that standard. That’s a gap - and it’s getting noticed.

What Happens After the Inspection
If inspectors find problems, they hand out FDA Form 483 - a list of “objectionable conditions.” This isn’t a fine. It’s a warning. The company has 15 working days to respond with a detailed plan to fix each item. That plan must include:
- What went wrong
- Why it happened
- How it will be fixed
- How they’ll prevent it from happening again
Weak responses get ignored. Strong ones lead to closure. Poor ones? The FDA can issue a warning letter - and those are public. In 2023, the agency issued 1,842 warning letters. Medical device makers got 42% of them. Pharmaceutical companies got 38%. Food facilities got 20%.
If the problems are severe - like widespread contamination or falsified data - the FDA can shut down the facility. Or ban the product. Or even refer the case to the Department of Justice for criminal charges.
What’s Changing in 2025 and Beyond
The FDA isn’t standing still. By late 2024, they’ll start testing AI tools to scan inspection documents for red flags - things like repeated deviations, missing signatures, or mismatched dates. By 2026, they plan to use remote inspections for up to 35% of their reviews. Virtual tours and digital document access are already being piloted with 147 facilities. So far, they’ve matched in-person results for 78% of documentation checks.
At the same time, the agency is shifting resources. High-risk products - like those for elderly patients or complex biologics - will see more inspections. Low-risk items, like some dietary supplements, will see fewer. It’s not about being tougher. It’s about being smarter.
One thing won’t change: the expectation that companies know their own processes inside out. The FDA doesn’t want perfect records. They want honest, accurate, and traceable ones. They want people who understand why they do what they do. Because in the end, inspections aren’t about catching companies out. They’re about making sure what you take - or what’s put into your body - actually works, safely, every time.



Comments (13)
Cooper Long
The FDA's risk-based inspection model is scientifically sound. Prioritizing high-risk facilities improves resource allocation without compromising safety. Data integrity remains the weakest link across global manufacturing.
Simone Wood
I saw a plant in New Jersey get shut down last year because someone typed a batch number wrong. They didn't even have audit trails enabled. This isn't about compliance-it's about people treating life-saving meds like a spreadsheet game.
Swati Jain
Let’s be real-8 hours of training per year? That’s a joke. My cousin works in pharma QA and she’s been trained on 3 different ERP systems in 18 months. No one’s keeping up. They just pray the inspector doesn’t ask about change control logs.
Nikhil Purohit
I’ve been to a few of these inspections in Bangalore. The real issue isn’t the tech-it’s the culture. People hide mistakes because they’re scared of blame. If you want real compliance, you need psychological safety, not more forms.
Shawn Sakura
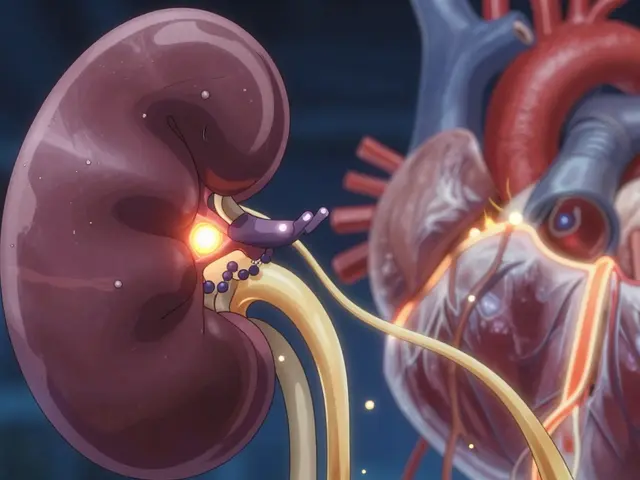
You guys are underestimating how much this matters. I had a family member on an insulin pump that failed. Turned out the manufacturer skipped validation on the sensor firmware. This isn’t bureaucracy-it’s life or death. Thank you, FDA, for doing the hard work.
Florian Moser
Mock inspections are the single most effective prep tool. We started doing them quarterly and our 483 observations dropped from 17 to 2 in one year. The key? Make it real. Bring in outside auditors. Don’t let your team know which files will be pulled.
Sammy Williams
I work in a med device shop. We have a dedicated inspection room now. Printer, 3 monitors, labeled binders, coffee. Inspectors actually smiled when they walked in. Weird, right? Turns out being organized makes people feel less like criminals.
jim cerqua
AI is coming for our paperwork. And honestly? Good. I’ve seen engineers delete failed tests and re-run them until they get a ‘pass.’ The FDA’s new tools will catch that in seconds. No more hiding behind sloppy data. The age of the paper trail is over.
Willie Doherty
The 78% statistic on documentation gaps is misleading. It conflates minor clerical errors with systemic failures. A missing signature isn’t the same as falsifying a validation protocol. The FDA needs to tier observations by severity, not just volume.
Julia Strothers
They’re using AI to spy on us? Of course they are. This is the deep state tightening its grip. They don’t care about safety-they care about control. Why not just install cameras in every lab? Next they’ll be scanning our thoughts. Wake up people.
Erika Sta. Maria
You all miss the point. The real problem isn’t data integrity-it’s the capitalist drive to cut corners. If you paid workers a living wage and gave them autonomy, they wouldn’t falsify records. This isn’t a technical issue. It’s a moral crisis disguised as compliance.
Sheldon Bazinga
FDA be trippin. We got 13k inspections a year? Bro we got 300k factories in this country. Half of these are in China anyway. Why are we even wasting money on this? Just let the market decide. If your pill gives you diarrhea, don’t buy it again.
Donald Frantz
The most dangerous thing I’ve seen? Companies that treat Form 483 as a checklist. They fix the listed items but ignore the root cause. That’s why repeat violations are so common. You can’t audit your way out of bad culture.