
Choosing the right insulin regimen isn’t just about lowering blood sugar-it’s about fitting treatment into your life without making it unbearable. Two main options dominate insulin therapy: basal-bolus and premixed insulin. Both work, but they’re built for very different people. One gives you freedom at the cost of complexity. The other simplifies your routine but locks you into a schedule. The side effects? They’re not the same. And your lifestyle? It’s the deciding factor.
How Basal-Bolus Insulin Works
Basal-bolus therapy uses two types of insulin: a long-acting background dose (basal) and fast-acting doses before meals (bolus). You take the basal shot once or twice a day to keep your blood sugar steady between meals and overnight. Then, before every meal, you inject a bolus based on how many carbs you’re eating and what your blood sugar is right now. This isn’t a one-size-fits-all dose-it’s customized.
Most people on this regimen need 4 to 5 injections daily. It sounds like a lot, but it’s designed for flexibility. Got a late lunch? Adjust your bolus. A big dinner? Add a little more insulin. A surprise snack? You can cover it. This system works because it mimics how a healthy pancreas releases insulin-steady background, bursts when needed.
Studies show this approach gets people closer to their HbA1c targets. In one 2014 meta-analysis, 63.5% of people on basal-bolus hit their goal of under 7% HbA1c, compared to just 50.8% on premixed insulin. It also reduces blood sugar swings, which lowers the risk of long-term damage to nerves, kidneys, and eyes. Continuous glucose monitors (CGMs) make this even better, letting you see trends and tweak doses in real time.
How Premixed Insulin Works
Premixed insulin is a fixed combo of two types-usually 70% intermediate-acting (like NPH) and 30% short- or rapid-acting insulin. It’s sold as a single vial or pen, so you get both types in one shot. You typically take it twice a day, before breakfast and dinner. Some people take it three times if they snack heavily, but it’s still fewer injections than basal-bolus.
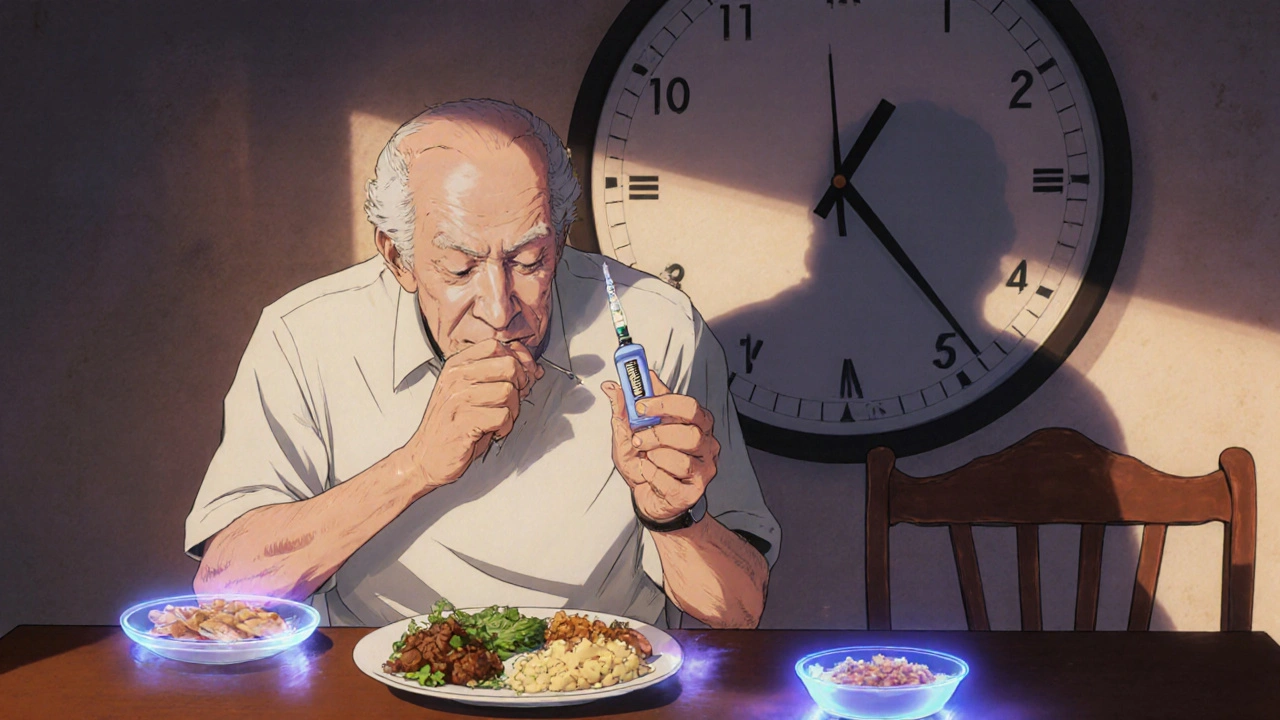
The big trade-off? Rigidity. Premixed insulin expects you to eat the same amount of carbs at the same time every day. Miss a meal? Your blood sugar can crash. Eat more carbs than usual? You might spike. There’s no room for adjustment. The insulin dose is locked in. That’s fine if you have a predictable routine-like a retiree eating meals at 8 a.m. and 6 p.m. every day. It’s not fine if you work night shifts, travel often, or skip meals because you’re busy.
Even though it’s simpler to use, studies show premixed insulin often requires higher total daily doses. One study found people on premixed took 0.72 units per kg of body weight, while basal-bolus users averaged 0.55. That’s because the intermediate-acting component (NPH) is less predictable and often needs higher doses to cover the same ground as modern long-acting insulins like glargine or degludec.
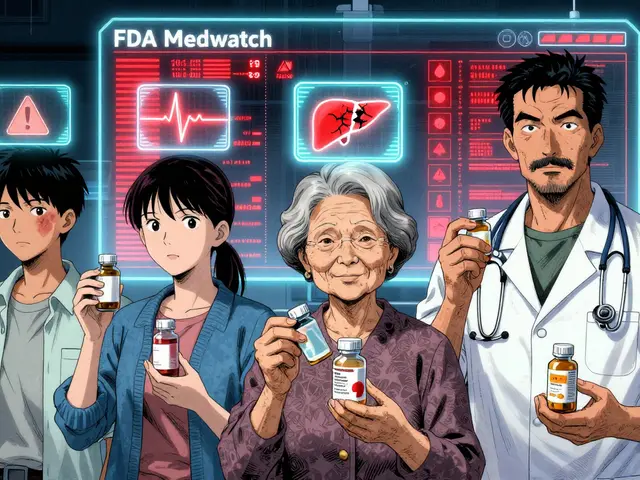
Side Effects: Hypoglycemia Risk Is the Real Difference
The biggest concern with any insulin is low blood sugar. But here’s where basal-bolus and premixed diverge sharply.
Premixed insulin carries a higher risk of hypoglycemia-especially between meals and overnight. Why? Because the intermediate-acting insulin peaks 4 to 8 hours after injection. If you don’t eat on schedule, or if you’re more active than usual, that insulin keeps working and your blood sugar drops. A 2015 trial was stopped early because over 50% of patients on premixed human insulin had dangerous lows. That’s not a small number-it’s a red flag.
Basal-bolus has lower hypoglycemia rates because the basal insulin is smoother and doesn’t peak. Modern analogs like glargine or detemir release insulin steadily over 24 hours. The bolus insulin acts fast and fades quickly. You’re less likely to have a low unless you miscalculate your meal dose. Even then, you can often catch it with a CGM before it becomes serious.
Weight gain is another side effect. Both regimens can cause it, but basal-bolus tends to lead to slightly more-around 1.9 kg on average versus 1.0 kg with premixed. Why? Because basal-bolus users are more likely to correct highs aggressively, which can lead to overtreating and then overeating to prevent lows. It’s a cycle.
Lifestyle Fit: Freedom vs. Structure
Here’s the truth: your daily life matters more than your HbA1c number if you can’t stick with the plan.
Basal-bolus demands skill. You need to count carbs. You need to check your blood sugar before every meal. You need to understand how stress, exercise, or illness affects your insulin needs. It takes 8 to 12 weeks to get comfortable. Many people give up early because it feels overwhelming. But for those who stick with it, satisfaction soars. A 2013 study found patients on basal-bolus were 50% more likely to reach their HbA1c goal-and reported better quality of life, less anxiety, and more confidence.
Premixed insulin is easier to start. You don’t need to count carbs. You don’t need to adjust doses daily. You just take your two shots and hope your meals stay consistent. That’s why it’s still popular among older adults, people with limited dexterity (like those with arthritis), or those who struggle with numbers. One patient on an ADA forum said, “Two shots a day instead of four has made managing my diabetes possible.” For them, simplicity beats perfection.
But the cost of simplicity? Rigidity. Reddit users often share stories like: “I switched from premixed to basal-bolus because I couldn’t handle the rigid meal schedule-missing a meal meant risking hypoglycemia even if my blood sugar was normal.” That’s not a minor inconvenience. It’s a barrier to living normally.
Who Should Choose What?
There’s no universal answer. But guidelines give clear direction based on who you are.
Choose basal-bolus if:
- You have type 1 diabetes
- Your blood sugar spikes badly after meals
- You have an irregular schedule (shift work, travel, unpredictable meals)
- You’re comfortable with numbers and tech (CGMs, apps, carb counting)
- Your goal is tight control to prevent complications
Choose premixed insulin if:
- You have type 2 diabetes with stable routines
- You struggle with multiple daily injections or dexterity issues
- You have cognitive challenges or find complex regimens overwhelming
- You eat three meals a day at the same time, with consistent carbs
- You’re in a resource-limited setting where cost matters
Doctors often default to premixed because it’s easier to prescribe. But a 2019 survey found only 42% of primary care physicians felt confident starting basal-bolus therapy. That’s a gap. If you’re being pushed toward premixed because it’s “easier for the doctor,” ask if it’s really easier for you.
What’s Changing in 2025?
The landscape is shifting. New tools are making basal-bolus less intimidating.
Hybrid systems like “basal-plus” (e.g., Tresiba with optional Fiasp) let you start with one daily shot and add mealtime insulin only when needed. It’s a middle ground.
CGMs are now standard for most people on insulin. Studies show they cut hypoglycemia risk in premixed users by more than half. If you’re on premixed and not using a CGM, you’re missing a major safety net.
And then there’s AI. Systems like Diabeloop DBLG1 use algorithms to suggest insulin doses based on your glucose trends, activity, and meals. Early trials show it cuts decision-making steps by 27%. That’s huge. It’s not fully automated yet, but it’s turning basal-bolus from a chore into a guided process.
By 2030, experts predict basal-bolus will become the standard in high-income countries-not because it’s perfect, but because technology is finally catching up to its complexity.
Cost and Accessibility
Money matters. Premixed insulin is cheaper. Medicare data shows average monthly out-of-pocket costs of $45.75 for premixed versus $68.20 for basal-bolus. Why? Basal-bolus requires two or three separate insulin products. Premixed is one.
But cheaper isn’t always better. If premixed leads to more lows, more hospital visits, or more missed work, the real cost goes up. Basal-bolus might cost more upfront, but it often saves money long-term by preventing complications.
Global use varies. Premixed makes up 55% of insulin prescriptions in Asia, where meals are more consistent. In North America, it’s only 28%. That’s not random-it’s cultural. Basal-bolus fits a lifestyle of variable schedules and individualized eating.
Final Take: It’s Not About Which Is Better. It’s About Which Is Right for You.
Basal-bolus isn’t “better.” Premixed isn’t “worse.” They’re tools for different jobs.
If you want freedom, precision, and the best chance at long-term health-and you’re willing to learn the system-basal-bolus is your path. You’ll need support, tech, and time. But the payoff is real.
If you need simplicity, consistency, and fewer injections-and your life fits a fixed schedule-premixed insulin can work. But don’t ignore the hypoglycemia risk. Use a CGM. Stick to your meals. Talk to your doctor about safety nets.
The goal isn’t to pick the most advanced option. It’s to pick the one you can live with-for years, not just months.
Which insulin has more side effects: basal-bolus or premixed?
Premixed insulin carries a higher risk of hypoglycemia, especially between meals and overnight, because its intermediate-acting component peaks unpredictably. Basal-bolus has lower hypoglycemia rates due to smoother, more predictable long-acting insulin and faster-acting meal doses. Both can cause weight gain, but basal-bolus tends to lead to slightly more. The key difference is not the number of side effects, but the type and timing-premixed risks lows when you don’t eat on schedule, while basal-bolus risks lows only if you misjudge your meal dose.
Can I switch from premixed to basal-bolus insulin?
Yes, switching is common and often beneficial-especially if you’re struggling with low blood sugar, irregular meals, or poor HbA1c control. The transition requires education: learning carb counting, adjusting doses based on glucose readings, and possibly using a CGM. Most people need 6 to 12 weeks to adjust. Work with a diabetes educator or endocrinologist. Don’t try to switch on your own. Your doctor will calculate your new doses based on your current premixed total and gradually phase in basal and bolus insulin.
Is basal-bolus insulin only for type 1 diabetes?
No. While basal-bolus is standard for type 1 diabetes, it’s also recommended for type 2 patients who need tighter control-especially those with high post-meal spikes, busy lifestyles, or who haven’t reached HbA1c targets on other treatments. The American Diabetes Association supports individualized therapy, and many type 2 patients benefit from the flexibility and precision of basal-bolus, even if they’ve been on pills or premixed insulin for years.
Do I need a continuous glucose monitor (CGM) with basal-bolus?
You don’t absolutely need one, but it’s strongly recommended. CGMs reduce guesswork, show you how food, stress, and activity affect your glucose, and help prevent lows before they happen. For basal-bolus users, CGMs turn complex dosing into a data-driven process. Studies show CGM use improves HbA1c and cuts hypoglycemia by 30-50%. If you’re on basal-bolus without a CGM, you’re managing blindfolded.
Why do some doctors prefer prescribing premixed insulin?
Doctors often choose premixed insulin because it’s simpler to prescribe and easier for patients to follow-especially if they’re older, have limited health literacy, or struggle with multiple daily injections. A 2019 survey found only 42% of primary care doctors felt confident starting basal-bolus therapy. Premixed requires less training, fewer calculations, and fewer follow-ups. But this convenience can come at the cost of safety and long-term control. If your doctor pushes premixed without discussing your lifestyle, ask if it’s really the best fit for you.




Comments (15)
Brian Bell
Man, I switched from premixed to basal-bolus last year and my A1c dropped from 8.2 to 6.4. No more 3 a.m. panic attacks from lows. Still hate counting carbs but my CGM does most of the thinking now. 🤖💯
Sean Evans
Let’s be real-premixed insulin is for people who can’t handle responsibility. If you’re too lazy to count carbs or check your glucose, don’t blame the insulin. Blame yourself. I’ve seen people on premixed crash so hard they end up in the ER. It’s not complicated-it’s just work. And if you’re too tired to do the work, maybe you shouldn’t be on insulin at all.
Scarlett Walker
Hey, I was on premixed for 5 years and I felt like a prisoner to my schedule. Then I switched-and yes, it was overwhelming at first. But now I can eat pizza at midnight without panic. It’s not perfect, but it’s mine. You got this. 💪❤️
Hrudananda Rath
One must observe with clinical detachment that the very notion of basal-bolus as a 'freedom' paradigm is a neoliberal illusion propagated by pharmaceutical marketing departments. The human pancreas does not operate on bolus schedules-it operates on circadian rhythm. To impose algorithmic insulin delivery upon biological systems is to commit epistemological violence upon the patient's autonomy.
Nathan Hsu
My grandfather, 78, on premixed insulin since 2010-eats breakfast at 7:30, lunch at 1:00, dinner at 7:00-no deviations. No CGM. No apps. Just two pens, two meals, two lives. He’s alive, he’s stable, he’s happy. Who are we to say his life is 'less than' because it doesn’t match Silicon Valley’s insulin fantasy?
Ashley Durance
People who say basal-bolus is 'better' are usually the ones who have the time, money, and mental bandwidth to obsess over every carb. Most of us don't. And the fact that you think your way is superior doesn't make it right-it just makes you tone-deaf.
Scott Saleska
Just wondering-have any of you tried basal-plus? I started with Tresiba and only added Fiasp when I ate out. It’s like a gateway drug to basal-bolus. No need to go full 5 shots a day right away. My doc called it 'insulin lite.' Kinda nice.
Ryan Anderson
For those considering switching: Don’t rush it. I spent 10 weeks with a diabetes educator learning carb ratios, correction factors, and how to read my CGM trends. I cried a lot. I failed a lot. But now I’m not just surviving-I’m living. You don’t need to be perfect. You just need to show up.
Eleanora Keene
My sister switched to basal-bolus and now she’s got her life back. She travels, eats sushi, goes out dancing. She still has lows sometimes, but she catches them. I’m so proud of her. If you’re scared, start small. One meal. One adjustment. One win. You’re not alone.
Joe Goodrow
Why do Americans think they need all this fancy tech just to manage diabetes? In my country, we just eat right and take our shots. Premixed works fine. You don’t need a smartphone to live. Maybe you need less tech and more discipline.
Anjan Patel
OH MY GOD I WAS ON PREMIXED FOR 8 YEARS AND I HAD A SEIZURE AT 3 AM BECAUSE MY NPH PEAKED AND I WASN’T EATING-MY MOM HAD TO CALL 911 AND NOW I’M ON BASAL-BOLUS AND I FEEL LIKE A NEW PERSON AND I JUST WANT TO SCREAM AT EVERY DOCTOR WHO PUSHED PREMIXED ON ME BECAUSE IT WAS EASIER FOR THEM
Kevin Wagner
Basal-bolus isn’t just insulin-it’s a lifestyle upgrade. You’re not just managing blood sugar-you’re reclaiming your autonomy. Yeah, it’s a grind at first. But once you crack the code? You’re not a patient. You’re a data wizard. A glucose ninja. A carb-calculating samurai. 🥷💉
gent wood
My brother-in-law, diabetic since 1997, still uses vials and syringes. No pens. No CGMs. Just paper logs and a calculator. He’s 72, active, sharp. His secret? Consistency. Routine. Respect for the condition. Technology helps-but it doesn’t replace wisdom.
Dilip Patel
premixed is for real people not tech bros with their fancy apps and cgms i work 12 hour shifts and i eat when i can and premixed keeps me alive so dont act like your way is better
Ryan Anderson
Reading this thread reminded me-when I first switched, I thought I’d fail. But I didn’t. I just needed time. And a good educator. And a lot of chocolate. 😅