
When a brand-name drug loses its patent, the first generic version usually hits the market at about 87% of the original price. It sounds like a big discount, but here’s the real story: the biggest price drops don’t come from the first generic. They come from the second and third.
Why the second generic is the game-changer
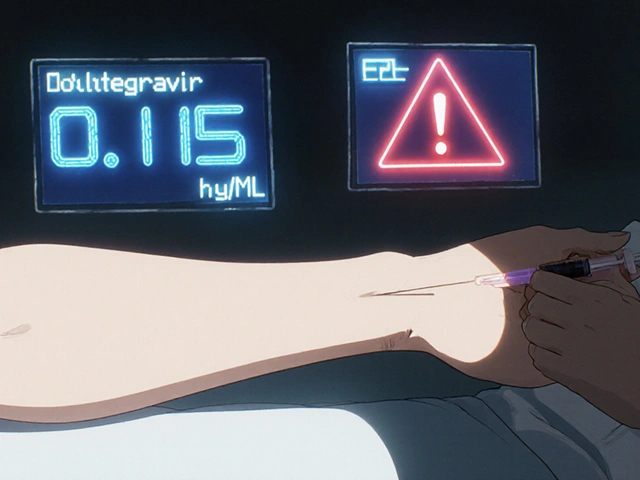
The moment a second company starts selling the same drug, prices don’t just dip-they plunge. Data from the FDA shows that after the first generic enters, the average price is still at 87% of the brand’s original cost. But as soon as a second manufacturer joins, that number drops to 58%. That’s not a 10% reduction. It’s a 31% drop in just one step. This isn’t luck. It’s basic economics. When there’s only one generic seller, they have little pressure to lower prices further. They’re the only option. But bring in a second company, and suddenly there’s a race to the bottom. Each one tries to undercut the other to win contracts with pharmacies, hospitals, and pharmacy benefit managers. The result? You pay less. Insurance plans pay less. The whole system saves money.The third generic makes it even worse-for drug companies
If the second generic cuts prices nearly in half, the third one slams the door shut. Prices fall again-to just 42% of the original brand price. That’s more than a 50% drop from the second generic’s price alone. In some cases, drugs that once cost $100 a month drop to under $40 after three manufacturers are selling them. The FDA tracked this across thousands of drugs approved between 2018 and 2020. The result? $265 billion in savings for patients and the healthcare system. Almost all of that came from competition beyond the first generic. The first generic opened the door. The second and third kicked it down.What happens when competition stalls
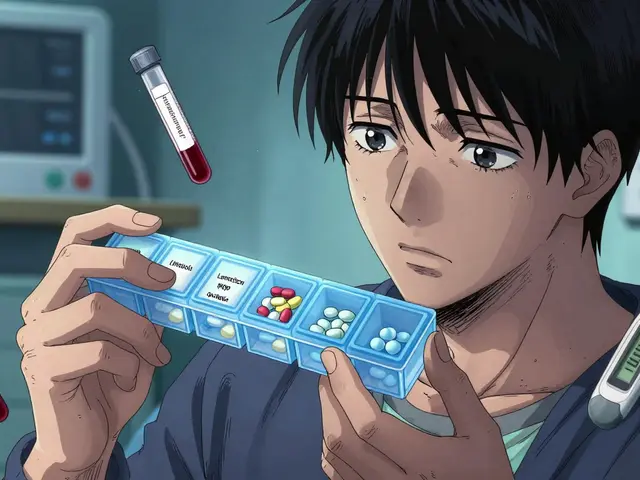
Not every drug gets a second or third generic. In nearly half of all generic markets, only two companies ever enter. That’s called a duopoly. And in those cases, prices don’t keep falling. They stabilize-or even rise. A 2017 study from the University of Florida found that when a market drops from three competitors to two, prices can spike by 100% to 300%. Why? Because with only two players, they can quietly coordinate pricing without fear of being undercut. It’s not collusion-it’s just the natural outcome of too little competition. This isn’t hypothetical. Drugs like levothyroxine, metformin, and amlodipine have all seen wild price swings when manufacturers exit or merge. When one of the three makers of a common blood pressure drug shuts down production, the remaining two raise prices. Patients pay more. Pharmacies pay more. And the system pays more.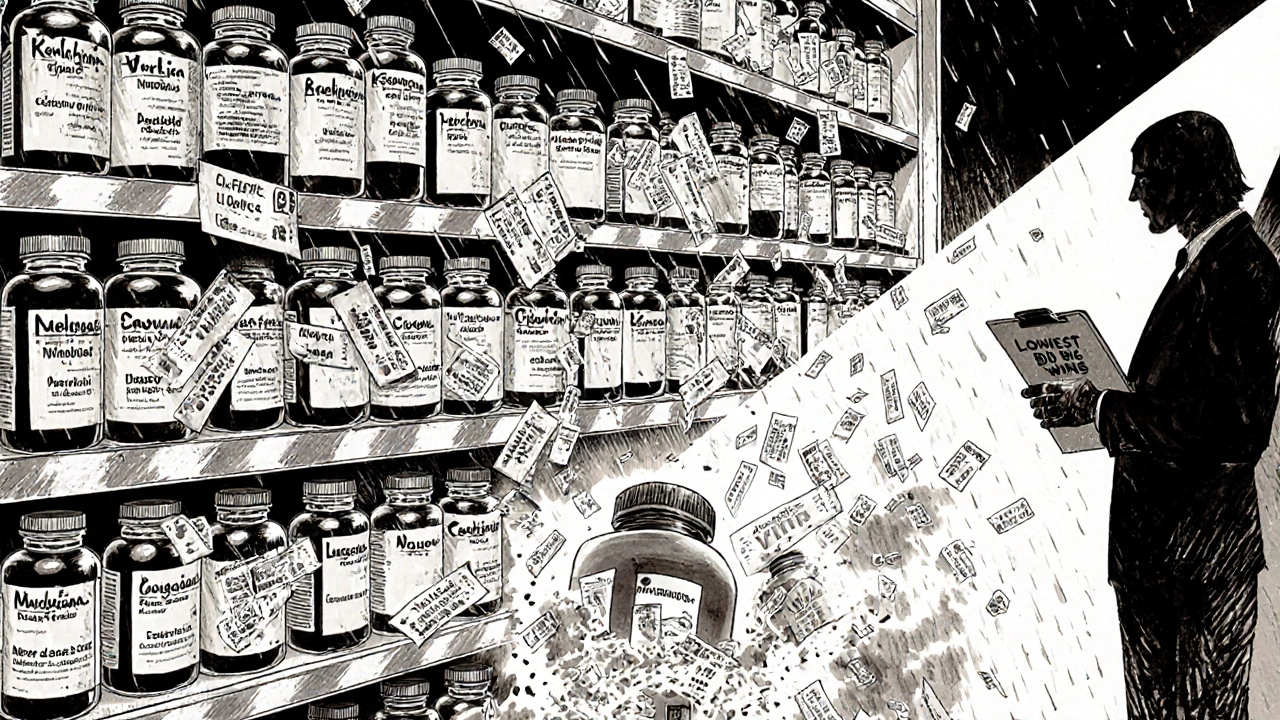
Who’s really setting the price?
You might think drug manufacturers control prices. But in reality, they’re caught in the middle. The real power lies with the “Big Three” wholesalers-McKesson, AmerisourceBergen, and Cardinal Health-and the big pharmacy benefit managers (PBMs) like Express Scripts and CVS Health. These companies buy in bulk and demand the lowest possible price. The more generic options they have, the more leverage they have. A PBM can tell a manufacturer: “We’ll buy from you if you match the lowest price on the market-or we’ll go to someone else.” That’s why prices keep falling with each new entrant. It’s not charity. It’s negotiation. But here’s the catch: when only one or two generics are available, PBMs have no real alternatives. That’s when prices creep up. And that’s exactly what happened with some antibiotics and heart medications after consolidation reduced the number of manufacturers.Why some drugs never get a second generic
Not all drugs are created equal. Simple pills like generic ibuprofen have dozens of manufacturers. But complex drugs-injectables, inhalers, or those requiring special manufacturing-take longer and cost more to copy. That’s why many of these drugs stay with only one or two makers. Brand-name companies also fight back. They use tactics like “pay for delay,” where they pay a generic maker to hold off on entering the market. One study estimated this costs patients $3 billion a year in higher out-of-pocket costs. Another tactic? Filing dozens of overlapping patents to stretch monopoly protection for years. One drug had 75 patents, keeping generics out for nearly two decades after the original patent expired. The FDA and Congress have started pushing back. The CREATES Act blocks brand companies from refusing to supply samples needed for generic testing. New laws aim to ban pay-for-delay deals. The FDA’s GDUFA III program is speeding up approvals for complex generics. But progress is slow.
What this means for you
If you take a generic drug, check how many makers produce it. If it’s just one or two, ask your pharmacist if there’s a version from another company. Sometimes, switching brands (not the drug, just the manufacturer) can save you 30% or more. If you’re on a high-deductible plan or pay cash, this matters even more. A $100 pill at 42% of brand price is $42. At 87%, it’s $87. That’s $45 you didn’t have to spend. Multiply that across your prescriptions, and you’re talking hundreds of dollars a year. Your insurance company knows this. That’s why they push for multi-source generics. They want you on the cheapest version. But you have to be the one to ask.What’s next?
Analysts predict generic prices will keep falling 3% to 5% a year through 2027-if competition stays strong. But if mergers continue to reduce the number of manufacturers, or if pay-for-delay deals go unchecked, those savings could vanish. The bottom line? The second and third generics aren’t just nice-to-have. They’re the main reason generic drugs work. Without them, we’d still be paying brand prices. With them, millions can afford their prescriptions.Don’t assume your generic is the cheapest just because it’s generic. Ask if there’s another maker. Ask if switching will save money. And remember: competition isn’t just good for the market. It’s the best tool we have to keep drugs affordable.
Why do generic drug prices keep dropping after the first one enters the market?
After the first generic enters, prices drop to about 87% of the brand’s price. But when a second manufacturer joins, competition forces prices down to 58%. A third lowers them further to 42%. Each new entrant pressures others to cut prices to win contracts with pharmacies and insurers. This isn’t about charity-it’s about market pressure.
What happens if only two companies make a generic drug?
When only two companies make a generic drug, it’s called a duopoly. Prices often stop falling and can even rise. Studies show that when a third competitor disappears, prices can jump 100% to 300%. With fewer options, companies have less incentive to undercut each other, and prices stabilize at higher levels.
Do pharmacy benefit managers (PBMs) help or hurt generic drug pricing?
PBMs help drive prices down when there are multiple generic makers. They use competition between manufacturers to negotiate the lowest possible price. But if only one or two generics exist, PBMs have little leverage. That’s why they push for more manufacturers-more options mean bigger discounts for patients and plans.
Why don’t more companies make complex generic drugs?
Complex generics-like inhalers, injectables, or extended-release pills-cost millions to develop and take years to get approved. Many smaller manufacturers can’t afford the risk. Big companies also delay entry by using patents or refusing to share samples. This keeps competition low and prices high for these drugs.
Can I ask my pharmacist for a different generic manufacturer?
Yes. Generic drugs have the same active ingredient, but different manufacturers. If your prescription is filled by one company, ask if another version is available. Switching to a different maker can save you 20% to 50%, especially if the drug has three or more manufacturers. Pharmacies often stock multiple brands and can switch without a new prescription.
What’s the biggest threat to generic drug price drops?
The biggest threat is reduced competition. When manufacturers merge-like Mylan and Upjohn forming Viatris-or when brand companies use legal tactics to block generics, fewer companies enter the market. That leads to higher prices. Pay-for-delay deals, patent thickets, and supply chain consolidation all limit the number of competitors, which hurts savings.

Comments (8)
Ezequiel adrian
Bro this is wild 😮 I had no idea the second generic was the real MVP. My insulin went from $80 to $35 overnight when another maker showed up. Pharma doesn't want you to know this.
Ali Miller
The fact that American consumers are this oblivious to basic market dynamics is embarrassing. We have the most advanced healthcare system in the world and yet we still don't understand supply and demand? Pathetic. 🇺🇸
JAY OKE
I work in pharmacy benefits and this is 100% accurate. The third generic is when the real savings kick in. PBMs don't care who makes it-they just want the lowest bid. It's not about ethics, it's about leverage.
Also, don't get me started on how some manufacturers delay entry just to avoid price wars. It's a mess.
Amanda Wong
You're oversimplifying. The FDA data you cite doesn't account for regional pricing disparities, formulary restrictions, or the fact that many patients are locked into specific generics due to insurance formularies. Also, the $265 billion figure is misleading-it includes savings from volume discounts, not just competition. This is dangerously reductive.
Stephen Adeyanju
So let me get this straight more generics = cheaper drugs yeah but why do they still cost so much like why cant we just make them for free bro
james thomas
The real story? Big Pharma and the Big Three PBMs are in bed together. They let one or two generics in so they can control the market. Then they raise prices just enough to look legit. Pay-for-delay? That's not a loophole-it's a cartel. And yeah I'm paranoid. Have you seen the FDA's approval logs lately?
Deborah Williams
It's fascinating how we treat medicine like a commodity when it's literally life or death. We celebrate competition in the abstract but never ask why we've allowed a system where someone's ability to breathe or think clearly depends on which manufacturer won a bidding war.
Maybe we should stop pretending this is capitalism and start calling it what it is: healthcare rationing by spreadsheet.
Asia Roveda
This is why we need to nationalize pharmaceutical production. Private companies will always game the system. Look at how many generics were pulled off the market during the pandemic because of supply chain issues. We can't trust profit-driven entities with essential medicine.