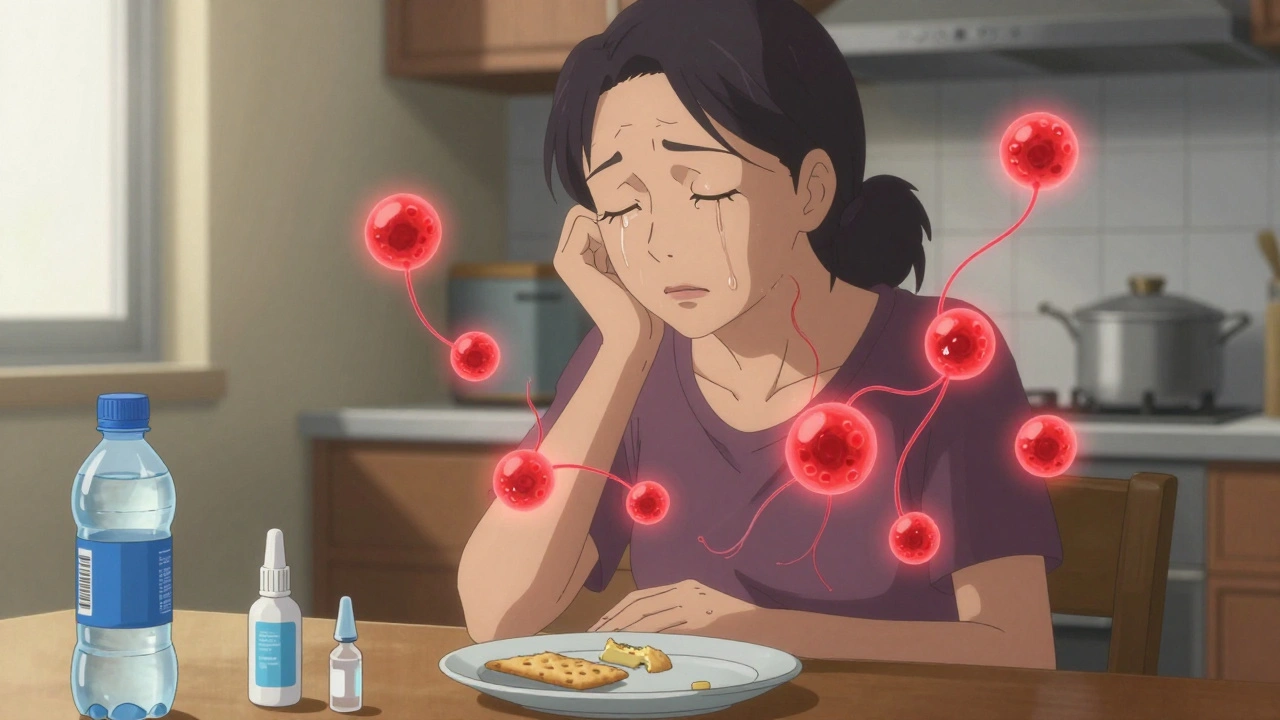
Sjögren’s Syndrome isn’t just about being thirsty or having watery eyes. It’s when your immune system turns on the very glands that keep you moist - the ones that make tears, saliva, and other lubricating fluids. Imagine your body’s natural wetness switches being flipped off, one by one. For millions of people, especially women over 45, this isn’t imagination - it’s daily reality.
What Exactly Happens in Your Body?
Sjögren’s Syndrome is an autoimmune disorder. That means your immune system, which should protect you from viruses and bacteria, starts attacking your own tissues. In this case, it targets the exocrine glands - the tear glands in your eyes, the salivary glands under your jaw, and even glands in your skin, lungs, and reproductive organs.
The result? Dryness. But not just any dryness. This is chronic, unrelenting dryness that doesn’t go away with a glass of water or eye drops. Your eyes feel gritty, like sand is rubbing against them. Your mouth becomes so dry that swallowing a cracker feels impossible without a full glass of water. You might find yourself sipping constantly, even at night.
It’s not just about comfort. Dry mouth increases your risk of cavities by 5 to 10 times. Without enough saliva to neutralize acids and wash away food particles, your teeth decay faster. Dental visits go from every six months to every three or four. And dry eyes? They can lead to corneal damage if left untreated.
It’s More Than Just Dry Eyes and Mouth
Most people think Sjögren’s is only about dryness. But it’s a systemic disease - meaning it can affect your whole body.
- Joint pain: About 30-50% of patients report achy, swollen joints - often mistaken for rheumatoid arthritis. But unlike RA, Sjögren’s rarely destroys joint structure.
- Extreme fatigue: Seven in ten patients say their tiredness is constant, crushing, and doesn’t improve with sleep. It’s not just being tired - it’s brain fog, memory lapses, and difficulty concentrating.
- Skin and vaginal dryness: Up to 20% develop dry, itchy skin or rashes. For women, vaginal dryness affects about half, leading to pain during sex and emotional strain.
- Nerve damage: Numbness, tingling, or burning in hands and feet happens in 10-15% of cases. This is called peripheral neuropathy.
- Lung issues: About 25% develop a persistent dry cough or shortness of breath due to inflammation in the airways.
One patient on Reddit wrote: “I’ve had colleagues think I was lazy or incompetent during meetings. I wasn’t zoning out - I was trying to find the right word because my brain was fogged from fatigue.”
Why Is It So Hard to Diagnose?
It takes an average of 2.8 years to get diagnosed. Why? Because the symptoms look like so many other things.
A primary care doctor might think it’s allergies. An ENT might blame acid reflux. A dentist might say you’re not drinking enough water. One patient visited four doctors over three years before getting a diagnosis.
Doctors don’t always know what to look for. Sjögren’s doesn’t show up on a standard blood test. Diagnosis requires a combination of:
- Symptoms: At least three months of persistent dry eyes and/or dry mouth.
- Tests: Schirmer’s test (measures tear production - less than 5mm in 5 minutes is abnormal) or a salivary flow test (less than 1.5mL in 15 minutes).
- Blood tests: Presence of anti-SSA/Ro and anti-SSB/La antibodies - found in 60-70% of cases.
- Biopsy: A small sample from the inner lip shows lymphocytes clustering around salivary glands - a hallmark of the disease.
Even then, it’s easy to miss. The American College of Rheumatology says many patients are told their symptoms are “just aging” or “stress-related.” But Sjögren’s isn’t normal aging. It’s an autoimmune attack.
Primary vs. Secondary Sjögren’s
There are two types:
- Primary Sjögren’s: Happens alone, without another autoimmune disease. About half of all cases.
- Secondary Sjögren’s: Occurs alongside other conditions like rheumatoid arthritis, lupus, or scleroderma. This makes up 30-50% of cases.
Secondary Sjögren’s is harder to spot because its symptoms get buried under the other disease. A rheumatologist treating lupus might not think to test for dryness - but they should. The presence of Sjögren’s changes how you manage the whole condition.
Who Gets It - And Why?
Nine out of ten people with Sjögren’s are women. The average age at diagnosis is 48. It’s rare in children, though cases have been seen as young as 8.
Genetics play a role. If you have a close relative with an autoimmune disease, your risk goes up. But genes alone don’t cause it. Something triggers it - likely a virus or bacterial infection in someone genetically prone to it. Researchers are still trying to figure out exactly what that trigger is.
It’s more common in Caucasians, but underdiagnosis in Black, Hispanic, and Asian populations is likely. Many people in these groups never get tested because their symptoms are dismissed or misattributed.
How Is It Treated? (No Cure - But There Are Options)
There’s no cure yet. But there are ways to manage symptoms and slow damage.
For dry eyes:
- Preservative-free artificial tears - use 8-10 times a day.
- Prescription eye drops like cyclosporine (Restasis) or lifitegrast (Xiidra) to reduce inflammation.
- Punctal plugs - tiny devices inserted into tear ducts to keep tears on the eye longer.
For dry mouth:
- Saliva substitutes (gels, sprays) - use 5-7 times daily.
- Medications that stimulate saliva: pilocarpine (5mg three times a day) or cevimeline (30mg three times a day). About 60-70% of patients report noticeable improvement.
- Chewing sugar-free gum or sucking on sugar-free hard candies to trigger natural saliva flow.
For systemic symptoms:
- Hydroxychloroquine (Plaquenil): Used in 40-50% of patients for joint pain and fatigue. Only 30-40% get real relief.
- Immunosuppressants: For severe cases involving lungs, kidneys, or nerves - drugs like methotrexate or azathioprine.
- New treatment: In June 2023, the FDA approved Efgartigimod (Vyvgart Hytrulo), the first new drug for Sjögren’s in 20 years. In trials, it improved dry mouth symptoms by 35% compared to placebo.
Dental care is critical: Brush twice a day with fluoride toothpaste, floss daily, and visit your dentist every 3-4 months. Your risk of cavities is 5-10 times higher.
What About Complementary Therapies?
Many patients turn to lifestyle and natural approaches:
- Omega-3 supplements: Used by 52% of patients in one survey - may help reduce inflammation.
- Humidifiers: Keep indoor humidity between 40-60% to ease dry skin, eyes, and airways.
- Diet changes: Avoid salty, dry, spicy, or acidic foods that irritate a dry mouth. Drink water constantly.
- Acupuncture: 23% of patients report improved dryness and pain after sessions.
- Specialized oral care: 89% use alcohol-free mouthwashes, moisturizing gels, or fluoride rinses.
One patient said: “Pilocarpine changed my life. I could finally eat a sandwich without needing a whole pitcher of water. I wish I’d tried it sooner.”

The Hidden Costs - Mental Health and Quality of Life
Sjögren’s doesn’t just hurt your body - it hurts your life.
A 2022 survey of 1,200 patients found:
- 87% struggled with daily activities because of dry mouth.
- 79% said eye pain affected their work performance.
- 63% reported social isolation - avoiding meals, gatherings, or even talking because of dryness.
- 42% experienced symptoms of depression - more than five times the general population rate.
Many feel dismissed by doctors. One patient said: “I’ve been told I’m exaggerating. That I just need to drink more water.”
But this isn’t in your head. The fatigue, brain fog, and pain are real. And they’re part of the disease.
What’s New in Research?
There’s real hope on the horizon.
- Targeted therapies: 12 new drugs are in clinical trials, including biologics that block B-cells - the immune cells driving the attack.
- Biomarkers: Researchers found a specific T-cell signature present in 78% of patients. This could lead to a simple blood test for early diagnosis.
- Genetic studies: The new TARGET initiative is mapping genes that predict who will develop severe disease.
- Ultrasound: Salivary gland ultrasound is now part of European diagnostic guidelines. It’s non-invasive, fast, and 85% accurate.
- Precision medicine: The NIH launched the Sjögren’s Precision Medicine Network in 2023 - aiming to match each patient with the best treatment based on their biology.
Still, funding is a problem. In 2022, the NIH spent $28.7 million on Sjögren’s research. For lupus? $167 million. For rheumatoid arthritis? $114 million. Sjögren’s affects 4 million Americans - yet gets less than 20% of the funding of diseases with fewer patients.
What’s the Long-Term Outlook?
Good news: 90% of people with Sjögren’s have a normal life expectancy.
Bad news: Quality of life drops by 30-40% compared to healthy peers. The biggest threat isn’t death - it’s lymphoma. People with Sjögren’s have a 4-5% lifetime risk of developing non-Hodgkin lymphoma. That’s 10 times higher than the general population.
That’s why regular check-ups matter. If you develop new lumps, unexplained weight loss, night sweats, or persistent fever, tell your doctor immediately.
With proper care - eye drops, saliva stimulants, dental visits, and monitoring - most people live full lives. But it takes work. And it takes being your own advocate.
What Should You Do If You Think You Have It?
If you’ve had dry eyes and dry mouth for more than three months - and nothing helps - it’s time to push for answers.
- Write down your symptoms: When did they start? How bad are they? What makes them better or worse?
- Track your medications. Some drugs - like antihistamines, antidepressants, or blood pressure pills - cause dryness. But if you’re on them and still dry, it’s not the cause.
- Ask your doctor for a referral to a rheumatologist. Not a dentist, not an ENT - a rheumatologist.
- Request the Sjögmer’s tests: Schirmer’s test, anti-SSA/SSB blood work, and possibly a lip biopsy.
- Bring a symptom tracker. Use a free app or a notebook. Show them your struggle - not just your words.
Don’t let anyone tell you it’s “just aging” or “all in your head.” Sjögren’s is real. It’s common. And you deserve to be heard.
Is Sjögren’s Syndrome the same as dry eye syndrome?
No. Dry eye syndrome can happen from screen use, aging, or contact lenses - and it usually doesn’t come with dry mouth, fatigue, or joint pain. Sjögren’s is an autoimmune disease that causes dryness in multiple glands and often affects other organs. If you have dry eyes plus dry mouth, fatigue, or joint pain, you need to be tested for Sjögren’s.
Can Sjögren’s Syndrome be cured?
There is no cure yet. But treatments can control symptoms and prevent complications. New drugs like Efgartigimod and ongoing research into biomarkers and targeted therapies offer real hope for better management - and possibly even remission - in the future.
Why does Sjögren’s affect women more than men?
The exact reason isn’t known, but hormones likely play a role. Estrogen may influence immune system behavior, making women more prone to autoimmune diseases. Also, genetic factors linked to X-chromosome activity may increase susceptibility. About 90% of cases occur in women.
Can you get Sjögren’s Syndrome if you’re under 40?
Yes. While most people are diagnosed between 45 and 55, it can occur at any age. Cases have been confirmed in children as young as 8, though these are rare - making up only 3-5% of total cases. Younger patients often have more systemic symptoms and may be misdiagnosed for longer.
Does diet affect Sjögren’s symptoms?
Diet doesn’t cause Sjögren’s, but it can make symptoms worse. Spicy, salty, acidic, or dry foods irritate a dry mouth. Alcohol and caffeine dehydrate you. Eating soft, moist foods and drinking water throughout the day helps. Omega-3 fatty acids (found in fish, flaxseed, walnuts) may reduce inflammation, and many patients report feeling better with these in their diet.
What’s the biggest mistake people make with Sjögren’s?
Waiting too long to get diagnosed. Many people live for years thinking their dryness is normal or stress-related. By then, damage to teeth, eyes, or nerves may have already started. The earlier you’re diagnosed, the better you can protect your body - and your quality of life.




Comments (15)
Francine Phillips
Been dry as a bone for years and no one believed me until I got diagnosed. Now I know it wasn't just me being dramatic.
Katherine Gianelli
Y'all need to hear this: Sjögren’s isn’t a lifestyle inconvenience-it’s a full-body rebellion. I’ve cried over my own tears because they don’t come anymore. I’ve chugged water like it’s oxygen. And yeah, I’ve eaten yogurt with a spoon because my mouth forgot how to chew. You’re not alone. We’re out here. And we’re not giving up.
Joykrishna Banerjee
Typical Western medical reductionism. You blame the immune system without acknowledging the environmental toxins, glyphosate-laden food supply, and EMF-induced immune dysregulation. This is a symptom of systemic collapse, not a standalone autoimmune disorder. Efgartigimod? A Band-Aid on a severed artery. The real cure is detox, fasting, and ditching the modern diet. But of course, Big Pharma won’t fund that.
Myson Jones
Thank you for this comprehensive overview. I appreciate the clinical precision and the emphasis on diagnostic criteria. As someone who has spent years navigating the healthcare system, I can attest that rheumatologists are the only specialists who consistently take these symptoms seriously. I would recommend all patients keep a detailed symptom journal and bring printed lab references to appointments. Knowledge is power.
parth pandya
u forgot to mention that pilocarpine can cause sweating like crazy. i was drenched in my office meeting. but yeah it saved my life. also use Biotene mouthwash, not any other. the alcohol ones burn like hell. also try coconut oil pulling, it helped me with dry mouth. ps: dont trust drs who say its just aging. its not.
Albert Essel
I’ve lived with this for 12 years. The fatigue? Real. The brain fog? Real. The way people look at you when you ask for water at dinner? That’s the real disease. I used to apologize for needing to drink constantly. Now I say, ‘I have Sjögren’s. This is just how I function.’ No shame. No explanation needed. You’re not broken-you’re just fighting a silent war.
Gavin Boyne
So let me get this straight-we’ve got a disease that affects 4 million people in the US, and it gets less funding than diseases that affect a fraction of that number? And we’re supposed to be grateful for a 35% improvement in dry mouth from a drug that costs $120,000 a year? This isn’t medicine. This is capitalism with a stethoscope. We’re not patients-we’re profit margins with eyelids.
Rashi Taliyan
I was diagnosed at 32. No one believed me. My mom said, ‘You’re just stressed.’ My boss thought I was ‘too dramatic’ for needing a water bottle at my desk. I cried in the bathroom every day for three months before I found a rheumatologist who listened. Now I carry lip balm, eye drops, and a printed copy of this article in my purse. I’m not asking for pity. I’m asking to be seen.
Gene Linetsky
They’re hiding the truth. Sjögren’s isn’t autoimmune-it’s a bioweapon side effect. The vaccines, the 5G towers, the fluoride in the water-they’re all triggering this in women because they’re genetically more susceptible. The NIH won’t admit it because they’re in bed with Big Pharma. Look at the timing: skyrocketing cases right after 2020. Coincidence? I think not. Someone’s watching. Someone’s testing.
Ignacio Pacheco
So Efgartigimod improves dry mouth by 35%? That’s… something. But what about the 65% of people who still feel like they’re chewing sandpaper? And why is the only ‘new’ treatment in 20 years just a band-aid? I mean, we’re talking about a disease that can cause lymphoma, and the best we’ve got is a drug that makes your mouth slightly less like the Sahara? This is tragic.
Jim Schultz
Let’s be real: this article is just a PR pamphlet for pharmaceutical companies. They’re selling you hope so you’ll keep buying their $200 eye drops and $100,000 drugs. Meanwhile, the real solution? Stop eating processed food. Stop drinking bottled water with fluoride. Stop staring at screens. But nope-let’s keep throwing money at drugs that barely work and call it progress. Classic.
Kidar Saleh
As someone who’s spent years in the UK NHS system, I can tell you this: Sjögren’s is a forgotten disease. I waited 18 months for a specialist referral. My GP said, ‘You’re too young for this.’ I was 41. I now use humidifiers, omega-3s, and carry saline spray everywhere. I’ve learned to live with it-but I shouldn’t have had to fight so hard to be believed. The system fails us daily.
Chloe Madison
You’re not broken. You’re not lazy. You’re not imagining it. I’ve been there-wiping my eyes with tissues at work, hiding my water bottle in my desk drawer like it’s contraband. But here’s the truth: you’re a warrior. Every time you swallow, every time you blink, every time you get up and do it anyway-you’re winning. Keep going. And if someone tells you it’s ‘just aging’? Smile, nod, and hand them this article. Then go get your damn pilocarpine.
Makenzie Keely
As someone who’s spent 15 years researching autoimmune conditions across cultures, I’ve seen how Sjögren’s is dismissed in communities where ‘toughing it out’ is valorized. In rural America, in parts of India, in conservative households-women are told to ‘drink more water’ or ‘stop being so sensitive.’ But this isn’t weakness. It’s biology. The fact that 90% of cases are in women? That’s not coincidence-it’s systemic neglect. We need global awareness campaigns, not just blog posts. We need policy changes. We need funding. And we need to stop treating chronic illness like a personal failure.
Also: the Schirmer’s test? It’s outdated. Salivary gland ultrasound should be first-line. It’s non-invasive, accurate, and accessible. Why are we still using paper strips in 2024? That’s not science-that’s inertia.
And to the person who said ‘just drink water’-you have no idea. Try swallowing a cracker with zero saliva. Try reading a screen when your corneas are raw. Try explaining to your child why you can’t kiss them goodnight because your lips are cracked and bleeding. This isn’t a lifestyle tweak. It’s a full-scale biological siege.
And yes-I’ve tried acupuncture. It helped my joint pain. Omega-3s? Yes. Humidifier? Always. But none of it replaces proper diagnosis, proper treatment, and proper validation. We don’t need platitudes. We need action.
Vincent Soldja
Diagnosis takes too long. Treatment options are limited. Funding is inadequate. The disease is under-recognized. End.