
Diarrhea Severity Calculator
Assess Your Diarrhea Severity
Enter your symptoms to determine the severity grade of your diarrhea according to medical guidelines
Enter your symptoms above to see your severity grade.
Diarrhea from medications isn’t just an inconvenience-it can stop your treatment, send you to the hospital, or even be life-threatening. Whether you’re on chemotherapy, antibiotics, or immunotherapy, sudden loose stools aren’t normal. They’re a signal that your body is reacting to the drugs, and medication-induced diarrhea needs quick, smart action. Ignoring it or waiting too long can turn a mild issue into a medical emergency.
What Causes Medication-Induced Diarrhea?
Not all diarrhea is the same. When a drug triggers it, the cause depends on the medicine. Chemotherapy drugs like irinotecan and 5-fluorouracil are major culprits. Up to 80% of patients on these treatments get diarrhea, and 10-25% end up with severe cases. Antibiotics are another big one-about 1 in 5 people on them develop diarrhea, often because the drugs wipe out good gut bacteria, letting harmful ones like Clostridioides difficile take over. Immunotherapy drugs, newer cancer treatments that boost your immune system, can also cause inflammation in the intestines, leading to watery stools.How Severe Is It? Grading the Symptoms
Doctors don’t just say “you have diarrhea.” They grade it to know how serious it is:- Grade 1: You have 1-3 more bowel movements than usual per day. Mild, but still needs attention.
- Grade 2: 4-6 stools a day. This is when most people start worrying. Treatment should begin now.
- Grade 3: 7 or more stools a day, or you’re incontinent, or you need to be hospitalized. This is urgent.
- Grade 4: Life-threatening. You’re dehydrated, your kidneys are struggling, or you’re in shock. Needs emergency care.
Waiting to act until you hit grade 3 or 4 is dangerous. The goal is to stop it at grade 1 or 2.
First-Line Treatment: Loperamide (Imodium)
If you start having loose stools, the first thing to do is take loperamide. Don’t wait. Don’t hope it’ll pass. Take 4 mg right away. Then take 2 mg every 4 hours after each loose stool-but never more than 16 mg total in a day unless you’re on irinotecan (then max is 24 mg).Why loperamide? It slows down your gut. Studies show it works in 60-75% of grade 2 cases. It’s cheap, easy to get, and works faster than other options. But it’s not magic. If diarrhea doesn’t improve after 24 hours, or if it gets worse, you need to move to the next step.
When Loperamide Fails: Octreotide
If you’re still having 4 or more stools a day after 24 hours of high-dose loperamide, it’s time for octreotide. This is a shot you give under the skin. Dose: 100-150 micrograms every 8 hours. It works by shutting down fluid leakage in the intestines.Octreotide isn’t fun. The injection stings. Some patients report pain at the injection site. But it’s effective. In severe cases (grade 3-4), it works in 60-95% of people. Doctors at Yale and Cleveland Clinic say: if you have grade 3 diarrhea, give the first shot within 4 hours. That cuts hospital stays by 35%.
Some patients get a continuous infusion if bolus shots don’t work. That means a small pump delivers it slowly over time. It’s not common at home, but hospitals use it when things get critical.
What NOT to Do: The Big Mistakes
There are dangerous traps here. The biggest one? Using loperamide if you suspect C. difficile. If you have fever over 38.5°C, bloody stools, or you’ve been on antibiotics recently, don’t take loperamide. It can trap toxins in your gut and cause toxic megacolon-a rare but deadly condition. Always get a stool test if you’re unsure.Another mistake? Taking loperamide for more than 48 hours. Studies show that prolonging it, even for “traveler’s diarrhea,” increases your risk of ileus (a paralyzed gut) by 15 times. It’s meant for short-term use, not long-term fixes.
Diet and Hydration: Your Hidden Allies
Medication-induced diarrhea drains your body. You lose water, salt, and potassium. That’s why hydration isn’t optional-it’s medical care.Drink oral rehydration solutions (ORS). Not Gatorade. Not coconut water. Use a solution with 75 mmol/L sodium, 75 mmol/L glucose, and 20 mmol/L potassium. You can buy packets (like Pedialyte) and mix one with 200 mL of water. Sip slowly, especially at night. Dehydration hits hard when you’re sleeping.
Stop milk and high-fat foods. They make diarrhea worse. Stick to bananas, rice, toast, applesauce, and chicken broth. No spicy, greasy, or sugary stuff. This isn’t about being “healthy”-it’s about giving your gut a break.
Special Cases: Antibiotics and C. difficile
If your diarrhea started after antibiotics, C. difficile is the top suspect. Testing is required. Don’t guess. If it’s confirmed, vancomycin is the go-to treatment. It costs more than metronidazole ($1,200 vs. $40), but it works 97% of the time versus 76%. That’s not a price-it’s a lifesaver.Probiotics? Only two strains matter: Lactobacillus rhamnosus GG and Saccharomyces boulardii. Others don’t help. The American Gastroenterological Association says they cut antibiotic diarrhea risk by half. But Mayo Clinic’s research says: only those two strains cut it. Take them daily during and after antibiotics.
What’s New in 2026?
Medicine hasn’t stood still. In 2023, the FDA approved a new drug called onercept for severe chemotherapy diarrhea. It reduces severe cases by 63%. It’s not everywhere yet, but it’s coming.Also, in June 2024, ASCO updated its guidelines. For patients about to start irinotecan, they now recommend taking neomycin (an antibiotic) for 2 days before treatment. It cuts diarrhea risk from 65% down to 32%. That’s huge.
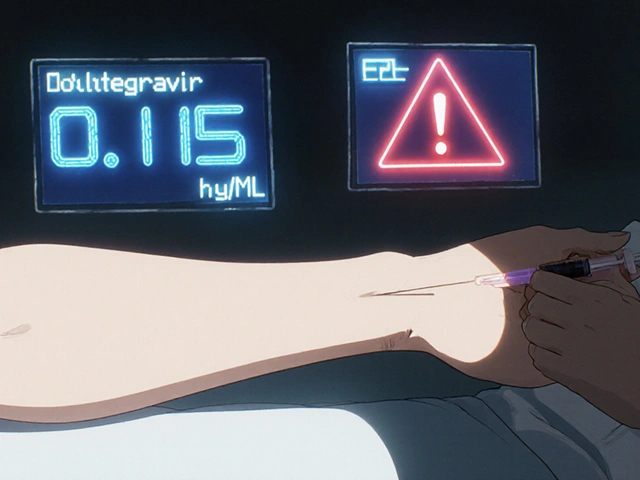
Future tools are even more promising. Blood tests to check your UGT1A1 gene can now predict if you’re likely to get severe diarrhea from irinotecan. If you’re high-risk, doctors can adjust your dose or start preventive treatments before you even get sick.
Real Patient Experiences
A 2022 survey of 1,247 cancer patients found 68% struggled to stick to loperamide schedules. Taking 2 mg every 4 hours while awake? Hard to do at night. Many missed doses and ended up in the ER.One Reddit user said: “I had to inject octreotide four times a day. My thigh was bruised. But I didn’t get hospitalized. Worth it.”
Another patient from Mayo Clinic said: “My nurse gave me a printed chart: ‘If you have 4 loose stools in 24 hours, call your oncologist.’ I did. They gave me octreotide the next day. I never went back to the hospital.”
The pattern? People who act fast survive better. Those who wait, pay the price.
What You Need to Do Right Now
If you’re on a drug that causes diarrhea:- Know your risk. Ask your doctor: “Is this drug likely to cause diarrhea?”
- Have loperamide on hand. Don’t wait for a prescription. Keep it at home.
- Start immediately. First loose stool? Take 4 mg now.
- Track your stools. Count them. Write them down. Show your doctor.
- Hydrate. Drink ORS every day, even if you feel fine.
- Call your provider if: Diarrhea lasts over 24 hours, you have fever, bloody stools, or more than 4 loose stools in a day.
There’s no shame in needing help. Medications save lives. But they also come with risks. Managing diarrhea isn’t weakness-it’s smart self-care.
Can I use Imodium for any type of medication-induced diarrhea?
You can use loperamide (Imodium) for most cases, except when you suspect a Clostridioides difficile infection. If you’ve been on antibiotics recently, have a fever over 38.5°C, or see blood in your stool, don’t take it. It can trap toxins and cause a dangerous condition called toxic megacolon. Always get a stool test if you’re unsure.
How long should I take loperamide before calling my doctor?
If your diarrhea doesn’t improve after 24 hours of taking loperamide as directed (4 mg initially, then 2 mg every 4 hours), it’s time to call. Also call if you have more than 4 loose stools in 24 hours, or if you develop fever, abdominal pain, or blood in your stool. Waiting too long increases your risk of severe complications.
Is octreotide safe to use at home?
Yes, octreotide is safe to use at home with proper training. It’s given as a subcutaneous injection, usually in the abdomen or thigh. Many patients learn to self-administer it. Nurses often provide step-by-step guides. The main side effect is pain at the injection site, which usually fades after a few days. It’s not a cure-all, but it’s the most effective treatment for severe, loperamide-resistant diarrhea.
Can probiotics prevent medication-induced diarrhea?
Only two probiotics have strong evidence: Lactobacillus rhamnosus GG and Saccharomyces boulardii. These reduce the risk of antibiotic-associated diarrhea by about half. Other probiotics don’t work as well. Take them daily during and for a week after antibiotics. They’re not a magic shield, but they help-especially if you’re prone to gut issues.
Why can’t I just drink more water instead of using oral rehydration solutions?
Plain water doesn’t replace what you lose. Diarrhea washes out sodium, potassium, and glucose. Drinking only water can dilute your electrolytes further, making you feel worse. Oral rehydration solutions (ORS) have the exact balance of salt, sugar, and minerals your body needs to absorb fluids properly. Use a pre-made ORS packet-don’t guess with sports drinks or homemade mixes.
Are there new treatments for medication-induced diarrhea in 2026?
Yes. In 2023, the FDA approved onercept, a new drug that reduces severe chemotherapy-induced diarrhea by 63%. Also, in 2024, ASCO updated guidelines to recommend neomycin prophylaxis before irinotecan treatment, cutting diarrhea risk from 65% to 32%. Blood tests to check your UGT1A1 gene are now used to predict who’s at high risk, allowing doctors to personalize treatment before it starts.



Comments (1)
Andy Cortez
So let me get this straight-you’re telling me I should just chug Imodium like it’s candy if my chemo starts giving me the runs? Bro. I had a friend take 16mg a day for a week because he was ‘too busy’ to call his oncologist. Ended up in the ER with a paralytic ileus. Loperamide ain’t a bandaid, it’s a time bomb if you ignore the signs. Don’t be that guy.