When someone is diagnosed with Huntington’s disease, the conversation rarely starts with hope. It starts with a countdown - a genetic clock ticking inside every cell of their body. There’s no cure. No magic pill. Just a slow, relentless breakdown of movement, thought, and emotion. And yet, for families facing this, the most powerful tool isn’t a drug - it’s care planning.
How Huntington’s Disease Is Passed Down
Huntington’s disease doesn’t skip generations. It doesn’t hide. If one parent has it, each child has a 50% chance of inheriting the faulty gene. It doesn’t matter if you’re male or female. It doesn’t matter where you live. The inheritance is exact, cold, and absolute.The problem lies in a single gene - HTT - on chromosome 4. Inside this gene, a tiny three-letter code, CAG, repeats too many times. Normal copies have 10 to 26 repeats. Anything above 40 means the disease will develop. Between 36 and 39, it’s a gray zone - some people get sick, others don’t. And between 27 and 35? That’s a ticking time bomb for the next generation. A parent with this range won’t show symptoms, but their child might inherit a much longer repeat and develop HD young.
Here’s the cruel twist: when the gene comes from the father, the CAG repeats often grow longer. This is called genetic anticipation. About 85% of juvenile Huntington’s cases - where symptoms start before age 20 - come from the father’s side. These kids don’t just get chorea; they get stiffness, seizures, and rapid decline. Their bodies can’t keep up.
By age 30 to 50, most people with 40 to 50 repeats begin to notice something off. A stumble. A twitch. A mood swing that doesn’t quit. By then, the brain has already lost thousands of neurons in the striatum - the area that controls smooth movement. The damage is silent until it’s too late to stop.
Chorea: The Signature Movement
Chorea is what most people picture when they think of Huntington’s. It’s not a tremor. It’s not a jerk. It’s a dance you didn’t sign up for - random, flowing, unpredictable movements that start in your fingers, then jump to your shoulder, then your foot. You can’t control it. You can’t hide it. And it gets worse when you’re stressed, tired, or trying to focus.Doctors measure chorea using the Unified Huntington’s Disease Rating Scale. A score of 1 means slight, occasional movements. A score of 4 means constant, violent motions that interfere with eating, walking, even breathing. In early stages, chorea is mild - just enough to make you feel embarrassed. By mid-stage, it’s exhausting. By late stage, chorea fades. Not because it’s better - because the brain has lost too many cells to produce it. What’s left is rigidity, slow movements, and difficulty swallowing.
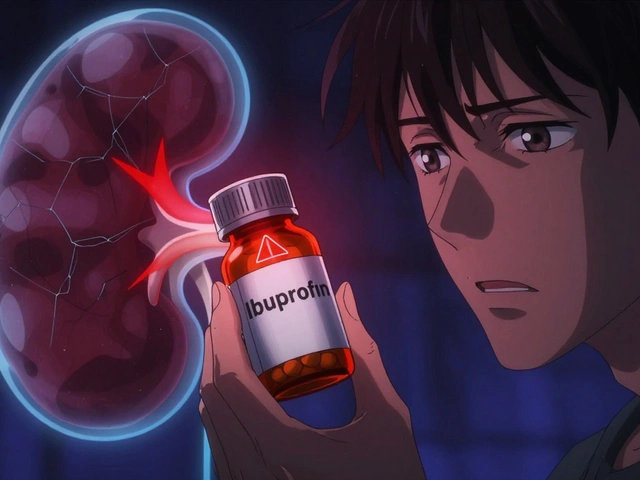
The only FDA-approved drugs specifically for chorea are tetrabenazine and deutetrabenazine (Austedo). They work by lowering dopamine in the brain. But they come with heavy trade-offs. One in five people on these drugs get severely depressed. Some stop taking them because the side effects feel worse than the chorea. Valbenazine (Ingrezza), approved in 2023, offers a similar benefit with slightly fewer mood effects - but it’s expensive, and insurance often fights coverage.
Physical therapy doesn’t stop chorea, but it helps you live with it. Aquatic therapy, in particular, shows real results. People who swim or do water-based exercises three times a week improve balance and coordination more than those doing land-based routines. Water supports the body. It reduces the risk of falls. It gives people back a sense of control - even if just for an hour.

What Happens When the Brain Fades
Huntington’s isn’t just about movement. It’s about losing yourself.Memory fades. Planning becomes impossible. You forget appointments, meals, even names. Decision-making slows. You might know what you want to say, but the words won’t come out right. Speech becomes slurred. Swallowing gets risky. Aspiration pneumonia - when food or saliva enters the lungs - becomes the leading cause of death.
Psychiatric symptoms hit just as hard. Depression affects 40% of patients. Anxiety, irritability, and obsessive behaviors are common. Suicide rates are 7 to 10 times higher than in the general population. Many people don’t realize how much emotional pain HD causes - until it’s too late.
By the time someone is 10 years into the disease, 65% need help with daily tasks like dressing or bathing. By 15 years, 45% need speech therapy because they can’t communicate clearly. And by 20 years, 89% require full-time care in a facility. The average cost? $125,000 a year. Most families aren’t prepared for that.
Care Planning Isn’t Optional - It’s Survival
The best thing you can do after a diagnosis isn’t to search for a miracle drug. It’s to build a plan - and start now.Specialized Huntington’s disease centers, like the 53 certified by the Huntington’s Disease Society of America, offer something general neurologists can’t: coordinated care. A team of neurologists, psychiatrists, physical therapists, social workers, and genetic counselors meet regularly. They track symptoms using the UHDRS. They adjust meds. They help with legal documents. They connect families to support.
People who get this kind of care live 2.3 years longer on average. They’re 32% less likely to end up in the hospital with pneumonia. And their risk of suicide drops by 58%.
But here’s the problem: only 38% of U.S. neurologists follow these guidelines. Only 45% of patients in the U.S. have access to a specialty center. In rural areas, it takes over two years to get a full care team together. That delay costs lives.
Early care planning includes three non-negotiable steps:
- Genetic counseling - before testing, after diagnosis. You need to understand what the results mean for you and your family.
- Advance directives - living wills, healthcare proxies, DNR orders. Only 37% of people in general care do this. At specialty centers, it’s 82%.
- Transition planning - knowing when to move from home care to assisted living, when to stop driving, when to get a feeding tube. These decisions don’t get easier with time.
One caregiver on the HDSA forum wrote: ‘The hardest part isn’t the chorea or even knowing I’ll decline - it’s watching my family try to plan for my deterioration while I’m still here.’ That’s the emotional weight no drug can touch.

The Financial and Emotional Toll
Huntington’s doesn’t just break your body. It breaks your bank account.Out-of-pocket costs for therapies, equipment, home modifications, and medications average $5,000 a year per patient. Many families sell homes, drain savings, or go into debt. Insurance rarely covers physical therapy, speech therapy, or home care aides long-term.
And then there’s the time cost. Caregivers spend 15+ hours a week just managing appointments, prescriptions, and paperwork. Most are spouses, adult children, or siblings. They quit jobs. They cancel vacations. They stop seeing friends.
On Reddit’s r/huntington community, people talk about the guilt of genetic testing. Many at-risk individuals wait until symptoms appear - even though testing is available. They fear knowing. They fear becoming a burden. They fear losing hope before they even need to.
But here’s what the data shows: people who get tested early - and plan - have better outcomes. They make decisions while they still have a voice. They choose their care. They protect their families from last-minute chaos.
What’s Next? Hope on the Horizon
There are 22 clinical trials running right now. One drug, tominersen from Roche, was paused in 2021 after showing no benefit - but restarted in 2023 with lower doses. Another, from Wave Life Sciences, reduced the toxic huntingtin protein by 38% in early trials. These aren’t cures - but they’re steps toward slowing the disease.Still, experts agree: even if gene therapies work tomorrow, they won’t help the 40,000 Americans already living with symptoms. For them, care planning is the only treatment that matters right now.
Dr. Rachel Andre at Johns Hopkins put it simply: ‘Comprehensive care planning isn’t the backup plan. It’s the main plan.’
That means: start now. Talk to your doctor about a specialty center. Fill out your legal documents. Get your family in the room. Learn what’s covered. Ask for help. Don’t wait for the worst to happen before you act.
Huntington’s disease doesn’t wait. Neither should you.

Comments (10)
Arup Kuri
They say care planning saves lives but nobody talks about how the system is rigged against poor folks
My cousin got diagnosed and the hospital wanted $20k just to see a specialist
Insurance said no
Now he's dying in a village with no therapy and his sister works three jobs just to buy him rice
They call this medicine but it's just a luxury for the rich
Patricia McElhinney
While I appreciate the attempt at outlining clinical pathways, the article fundamentally misrepresents the biological inevitability of HD progression. The notion that 'care planning' can alter neurodegenerative trajectories is not supported by peer-reviewed literature-only palliative measures are validated. The HDSA guidelines, while well-intentioned, lack robust longitudinal data. Moreover, the emphasis on genetic counseling without addressing the ethical quagmire of predictive testing in minors is grossly irresponsible. This is not medicine-it’s performative compassion.
Dolapo Eniola
Nigeria has no HD centers but we still care
My uncle had it and we used ginger tea and prayers
He lived 12 years after diagnosis
USA thinks money fixes everything
But real love? That's free
Stop selling hope with bills
😂
Agastya Shukla
Interesting breakdown of CAG repeat dynamics-especially the paternal anticipation effect. The 85% stat aligns with recent Nature Genetics papers from 2022. But I'm curious: how do you account for modifier genes like DNA repair variants (MLH1, MSH3) that might influence expansion rates? Also, the UHDRS scoring system has been criticized for low inter-rater reliability in rural settings. Has any study validated its use in low-resource environments?
Pallab Dasgupta
Let me tell you something real
I watched my dad go from fixing cars to forgetting how to hold a wrench
He cried every night because he couldn't tie his shoes
But we didn't wait for a specialist
We got a pool, bought a cheap walker, and started cooking soft meals
And yeah-we fought insurance
And yeah-we cried
But we didn't let the system decide when we gave up
Don't wait for permission to love someone
Just start now
❤️
Ellen Sales
It's not just about planning-it's about dignity
My mom chose her own feeding tube timing
She picked her hospice
She told us when to stop driving
She didn't wait for someone else to decide for her
That's power
That's love
That's what they don't tell you in the brochures
Planning isn't giving up-it's taking back control
And if you're waiting for the 'right time'-you're already too late
giselle kate
Of course the system is broken. America spends billions on military drones but can't fund a neurologist for a dying man
They let people rot in waiting rooms while billionaires get gene therapies in Switzerland
HD isn't a medical problem-it's a moral failure
And you want me to be grateful for a 'care plan' when the government won't even cover speech therapy?
Wake up.
Emily Craig
So let me get this straight-you're telling me the only thing that gives people 2.3 extra years is… paperwork?
Not a cure
Not a miracle
Just… forms
And somehow that’s supposed to make us feel better?
Wow.
What a beautiful, tragic, deeply American way to die.
At least we have our checklists.
Leisha Haynes
I'm a caregiver for my sister
She's 34
She can't say her own name anymore
But she still smiles when I play her favorite song
And you know what?
We didn't need a specialist to know that
She didn't need a form to feel loved
But I'm glad someone's writing this
Because maybe one family will read it and start talking before it's too late
Thank you for not staying silent
Shivam Goel
The article is dangerously oversimplified. It ignores epigenetic modulation of HTT expression, omits the role of microglial activation in neuroinflammation, and fails to contextualize the 38% compliance rate within the structural constraints of Medicaid reimbursement codes. Moreover, the assertion that 'care planning is the main plan' is a euphemism for medical abandonment under capitalism. The real tragedy isn't HD-it's the commodification of human suffering into a checklist for insurance auditors. Tetrabenazine’s depression risk? 20%. But the suicide risk from bureaucratic neglect? Unmeasured. Unreported. Unpunished.