Sirolimus Wound Healing Risk Calculator
Why Sirolimus Slows Down Wound Healing
Sirolimus, also known as rapamycin, is an immunosuppressant used after organ transplants to stop the body from rejecting the new organ. It works by blocking a protein called mTOR, which controls cell growth and repair. While this helps protect transplanted kidneys, it also slows down how fast your skin and tissues heal after surgery. The problem isn’t just theoretical - in animal studies, rats given sirolimus at therapeutic doses had wounds that were up to 40% weaker than those not on the drug. Their collagen, the main structural protein in healing tissue, dropped significantly. This isn’t a minor side effect. It’s a direct biological interference with the body’s natural repair process.
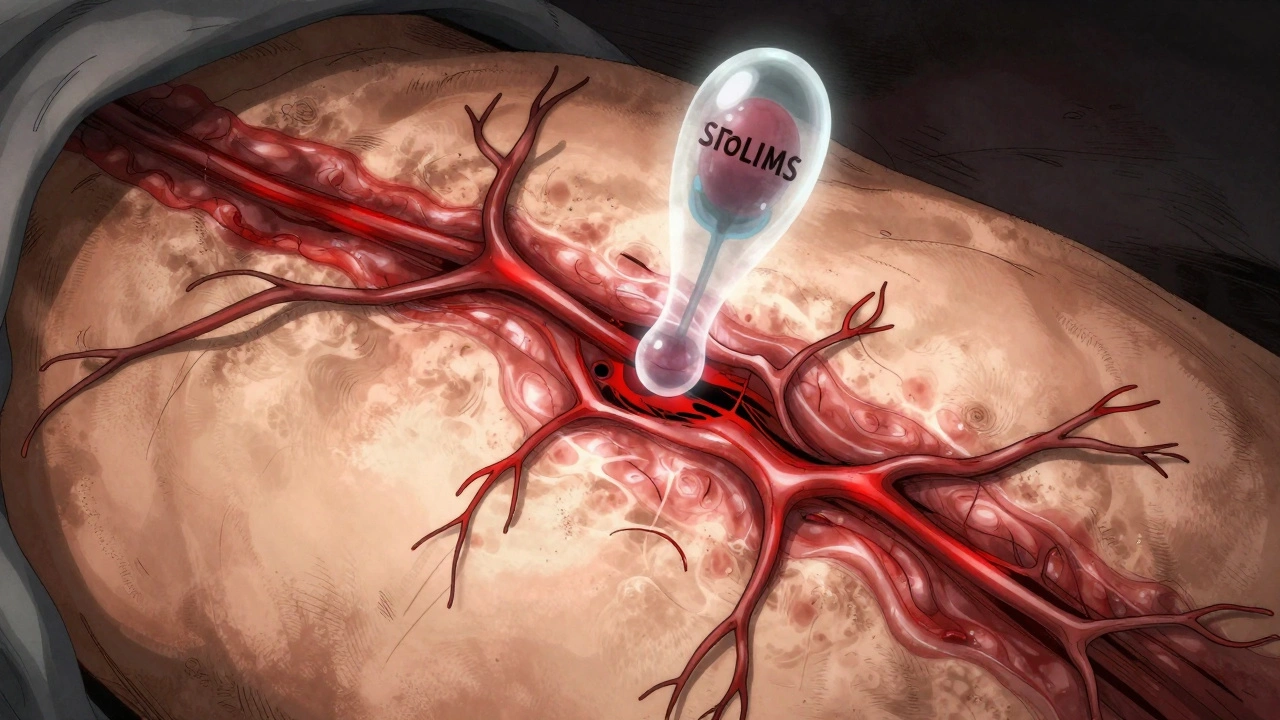
What’s happening inside the wound? Sirolimus cuts off key signals needed for healing. It reduces vascular endothelial growth factor (VEGF), a molecule that tells blood vessels to grow into the wound area. Without enough VEGF, the wound doesn’t get the oxygen and nutrients it needs. It also lowers nitric oxide levels, which helps relax blood vessels and bring in healing cells. Fibroblasts - the cells that build new tissue - stop multiplying. Smooth muscle cells, which help close wounds, don’t move in properly. The result? A wound that takes longer to close, is more likely to split open, and is more prone to infection.
The Real Risk: When and How Complications Happen
Early studies painted sirolimus as a major threat to surgical recovery. One 2007 study showed wound strength dropped by 30-50% in rats given doses similar to what humans receive. This led many hospitals to delay starting sirolimus for at least two weeks after surgery. But real-world data tells a more complicated story.
A 2008 Mayo Clinic study looked at 26 transplant patients who got sirolimus after dermatologic surgery. Their infection rate was 19.2% compared to 5.4% in those not on sirolimus. Wound dehiscence - where the surgical cut reopens - happened in 7.7% of sirolimus patients versus 0% in the control group. But here’s the catch: none of those differences were statistically significant. That means the numbers were too small to say for sure if sirolimus caused the problem, or if it was just bad luck. Still, the trend was clear: risk went up.
The bigger issue? Major abdominal surgeries. Most complications - like lymphoceles (fluid collections) or wound breakdown - happen after kidney transplants, where the incision is large and deep. In these cases, sirolimus can delay healing enough to cause serious problems. But for smaller procedures, like skin biopsies or minor excisions, the risk is much lower. The type of surgery matters as much as the drug.
Who’s Most at Risk - And Why
Not everyone on sirolimus will have trouble healing. The real danger comes from a mix of factors that stack up. The biggest one? Body mass index (BMI). A higher BMI means more pressure on the wound, less blood flow to fatty tissue, and more inflammation. Studies show the odds of wound problems jump with every point increase in BMI. This isn’t just a suggestion - it’s a hard clinical predictor.
Other risk factors are just as important. Diabetes? High blood sugar keeps immune cells from working right and slows collagen production. Smoking? Nicotine shrinks blood vessels, starving the wound of oxygen. Protein malnutrition? Your body can’t rebuild tissue without enough protein. Alcohol abuse? It weakens your immune system and damages liver function, which affects how your body processes drugs.
Here’s the good news: most of these are modifiable. You can quit smoking. You can control your blood sugar. You can improve your diet. If you’re planning surgery, getting your nutrition up and your blood sugar stable four to six weeks ahead of time makes a real difference. One study found that fixing these issues reduced complications even in patients on sirolimus.

When to Start Sirolimus - The New Guidelines
For years, the rule was simple: wait two weeks after surgery. But newer evidence shows that’s often too long - and too risky. Delaying sirolimus too long increases the chance of organ rejection, especially in high-risk patients. The goal now isn’t to avoid the drug, but to use it smarter.
Current thinking, backed by the American Society of Transplantation (2021), says timing should be personalized. For low-risk patients - young, non-smokers, normal BMI, no diabetes - sirolimus can be started as early as 5-7 days after surgery. For high-risk patients - obese, diabetic, smokers - wait 10-14 days, and only if the wound looks clean and stable.
There’s also a new trick: monitoring drug levels. Keeping sirolimus trough levels between 4-6 ng/mL in the first 30 days after surgery reduces wound complications without increasing rejection risk. Too high? Healing slows. Too low? Rejection risk goes up. This isn’t guesswork - it’s precision medicine.
What About Other Drugs? The Bigger Picture
Sirolimus isn’t the only immunosuppressant that affects healing. Steroids, mycophenolate, and antithymocyte globulin (ATG) also slow down tissue repair. But here’s the twist: sirolimus is often used because it avoids kidney damage. Tacrolimus and cyclosporine, the more common alternatives, are great at preventing rejection - but they hurt the kidneys over time. For patients with early signs of kidney damage from other drugs, switching to sirolimus might actually improve long-term outcomes, even if healing takes a little longer.
The key is combination therapy. Many patients get sirolimus with low-dose steroids and minimal mycophenolate. This reduces the total immunosuppressive burden while still protecting the transplant. Doctors now look at the whole picture - not just one drug.
What’s Changed - And What’s Still a Myth
A decade ago, many surgeons refused to use sirolimus in transplant patients altogether. Now, that’s changing. The old belief that sirolimus always causes bad wounds? That’s a myth. The real story is more nuanced. With better patient selection, tighter drug monitoring, and smarter timing, complications are dropping.
One 2022 review called the early fears about sirolimus and wound healing “old myths” that have been replaced by “new realities.” Clinicians now know that the risk isn’t in the drug itself - it’s in how it’s used. A patient with a BMI of 35, uncontrolled diabetes, and who smokes 20 cigarettes a day? That’s a high-risk case. A 45-year-old non-smoker with a BMI of 22 and normal blood sugar? That’s a low-risk case. The drug doesn’t change - the patient does.
And the benefits? They’re real. Sirolimus reduces the risk of skin cancer - a major threat for transplant patients. It doesn’t damage kidneys like other drugs do. For patients who live 10, 15, or 20 years after a transplant, those long-term benefits can outweigh the short-term healing delay.
Practical Steps for Patients and Providers
If you’re on sirolimus or planning to start it, here’s what you need to do:
- Get your health in order before surgery. Quit smoking at least four weeks ahead. Control your blood sugar. Eat enough protein - aim for 1.2-1.5 grams per kilogram of body weight daily. Fix nutritional gaps now, not after surgery.
- Know your BMI. If your BMI is over 30, talk to your doctor about weight management before surgery. Even a 5-10% drop in body weight can improve healing.
- Ask about drug levels. Don’t just take the dose - ask if your trough level will be checked at day 7 and day 14. Levels between 4-6 ng/mL are the sweet spot.
- Don’t assume you’re too risky. Many patients are turned away from sirolimus unnecessarily. If you’re a good candidate, the benefits can be worth the wait.
- Watch your wound closely. Redness, swelling, or fluid leaking after day 5? Call your surgeon. Don’t wait. Early intervention stops small problems from becoming big ones.
Final Takeaway: It’s Not About Avoiding Sirolimus - It’s About Using It Right
Sirolimus isn’t the enemy of healing. Poor timing, bad patient selection, and ignoring modifiable risks are. The drug has a place in modern transplant care - especially for patients who need to protect their kidneys or avoid cancer. The goal isn’t to avoid it. It’s to start it at the right time, at the right dose, for the right person.
For transplant teams, this means moving away from blanket delays and toward individualized plans. For patients, it means taking control of your health before surgery - because your healing doesn’t just depend on the drug. It depends on you.
Does sirolimus always cause poor wound healing?
No. Sirolimus can slow healing, but complications are not guaranteed. Risk depends on factors like BMI, diabetes, smoking, and timing of drug initiation. Many patients heal normally when sirolimus is started after 7-14 days and kept at therapeutic trough levels (4-6 ng/mL). The drug’s risks are manageable with proper planning.
When should sirolimus be started after surgery?
For low-risk patients (normal BMI, no diabetes, non-smoker), sirolimus can be started as early as 5-7 days after surgery. For high-risk patients (BMI over 30, diabetes, smoker), wait 10-14 days - only if the wound is stable and clean. Always monitor trough levels to keep them between 4-6 ng/mL during the first 30 days.
Can I still take sirolimus if I’m overweight?
Yes, but the risk of wound complications increases with higher BMI. If you’re overweight, focus on improving nutrition, controlling blood sugar, and losing even 5-10% of your body weight before surgery. Many centers will still use sirolimus in obese patients - but only with extra caution and delayed initiation.
Does sirolimus cause more infections than other immunosuppressants?
Studies show a trend toward higher infection rates with sirolimus, but not always statistically significant. The bigger issue is wound dehiscence and lymphocele formation, not general infections. Compared to calcineurin inhibitors like tacrolimus, sirolimus may actually lower the risk of certain viral infections like CMV.
Is sirolimus better than tacrolimus for kidney transplant patients?
It depends. Tacrolimus is more effective at preventing acute rejection, but it damages kidneys over time. Sirolimus doesn’t harm kidneys and reduces cancer risk - making it better for long-term use, especially in patients with early kidney damage or high cancer risk. The choice isn’t about which drug is stronger - it’s about which fits your long-term health goals.
Can I stop sirolimus if my wound isn’t healing?
Never stop sirolimus without talking to your transplant team. Stopping suddenly can cause organ rejection. If healing is slow, your doctor may temporarily lower the dose, delay the next dose, or switch to a different immunosuppressant - but only under close monitoring. Self-discontinuation is dangerous.





Comments (12)
Sean McCarthy
Sirolimus slows healing. Period. Don't let them sugarcoat it with 'personalized medicine'. If your wound isn't closing, it's because the drug is doing exactly what it's designed to do: stop cells from growing. Stop pretending it's a choice.
Kshitij Shah
In India we see this all the time. Patients on sirolimus come back with wounds that look like they've been left in a desert. But you know what? They're alive. And that's what matters. Sometimes you trade skin for survival.
Dennis Jesuyon Balogun
The mTOR pathway is evolutionarily conserved across eukaryotes - this isn't merely a pharmacological side effect, it's a fundamental disruption of cellular homeostasis. The reduction in VEGF and nitric oxide isn't incidental; it's a direct consequence of mTORC1 inhibition. When we prioritize transplant survival over wound integrity, we are engaging in a biopolitical calculus that privileges systemic longevity over local tissue autonomy. The body is not a machine to be optimized - it is a dynamic, emergent system. To reduce healing to a dosing algorithm is to commit epistemic violence.
Grant Hurley
i just had a kidney transplant last month and started sirolimus at day 6. wound looks fine. no drama. maybe it's not as bad as they say? also i quit smoking 2 months ago and started eating eggs every day. small wins.
Lucinda Bresnehan
I'm a nurse in transplant unit and I've seen this so many times. The real issue isn't the drug - it's that we don't prep patients enough. Someone comes in with a BMI of 40, smokes, has HbA1c of 9, and we just say 'here's your meds.' No wonder wounds break open. We need to treat the whole person, not just the organ.
Shannon Gabrielle
So let me get this straight. We're supposed to wait two weeks so your fat ass can heal better? Meanwhile your new kidney is like 'yo I'm about to get rejected.' I'm all for 'personalized medicine' until it means I'm paying for your bad life choices.
ANN JACOBS
The biological mechanisms underlying mTOR inhibition are profoundly complex, and while the clinical implications for wound healing are indeed significant, one must also consider the broader ontological framework of immunosuppressive therapy in the context of chronic graft survival. The temporal dynamics of fibroblast proliferation, collagen deposition, and angiogenic signaling are not merely pharmacokinetic variables - they are integral components of a systemic, homeostatic equilibrium that must be delicately calibrated. To reduce this to a binary 'start or delay' protocol is to misunderstand the very essence of post-transplant physiology.
Nnaemeka Kingsley
bro if you overweight and diabetic and still smoke, sirolimus is the least of your problems. fix your diet first. walk 30 mins a day. drink water. no magic pill will save you if you dont help yourself.
Linda Migdal
This is why American healthcare is broken. We let people live like animals, then act shocked when they can't heal. We give them a new kidney, then blame the drug when their body falls apart. Where's the accountability?
Tommy Walton
mTOR = master regulator of cellular fate 🧬✨. Sirolimus isn't 'bad' - it's a philosophical statement. We choose longevity over immediacy. We choose the soul of the organ over the skin of the wound. 🌌💎 #TransplantPhilosophy
James Steele
The pharmacodynamic profile of sirolimus necessitates a nuanced understanding of its pleiotropic effects on the extracellular matrix. The suppression of collagen synthesis via downregulation of TGF-β and HIF-1α pathways is not a flaw - it's a feature. The real pathology lies in the clinical inertia of adhering to outdated 14-day protocols when pharmacokinetic monitoring enables precision dosing. We are not managing patients; we are optimizing biological systems.
Louise Girvan
They're hiding something. Why is sirolimus only used in transplant patients? Why not in cancer? Why are they pushing this now? The FDA approved it in 2000 - but the wound healing data? Buried. The real reason they want you on it? So you can't sue them later when your skin falls off. They know. They all know.