
Medication Reaction Assessment Tool
Assess Your Medication Reaction
This tool helps you determine if your symptoms require immediate emergency care (911) or if you can contact your doctor later. When in doubt, always call 911.
It’s not rare to feel off after taking a new pill. Maybe your stomach feels queasy, or your skin itches a little. But how do you know if it’s just a side effect-or something that could kill you in minutes? The difference between calling your doctor and calling 911 isn’t always obvious. One wrong choice can mean the difference between a quick fix and a trip to the ICU-or worse.
Not All Reactions Are the Same
Medications can cause a wide range of reactions. Some are harmless. Others are deadly. The key is knowing which is which.Most side effects are mild: nausea, drowsiness, dry mouth, or a mild rash. These usually don’t need emergency care. They’re listed in the drug’s package insert for a reason. But when you start seeing symptoms that involve more than one part of your body at once, you’re no longer dealing with a simple side effect. You might be having an allergic reaction-and time is critical.
According to the Mayo Clinic, serious drug allergies often kick in within an hour of taking the medication. But some reactions, like DRESS syndrome or serum sickness, can take days to show up. That’s why you can’t just wait and see. If something feels wrong, don’t brush it off.
Call 911 If You Have These Symptoms
If you or someone else has any of these symptoms after taking medication, call 911 right away:- Difficulty breathing, wheezing, or feeling like your throat is closing
- Swelling of the tongue, lips, or throat
- A sudden drop in blood pressure-feeling dizzy, lightheaded, or passing out
- A fast, weak, or pounding heartbeat
- Hives or a rash that spreads quickly, especially if it’s combined with vomiting, diarrhea, or stomach cramps
- Loss of consciousness
These are signs of anaphylaxis-a life-threatening allergic reaction. It doesn’t always look like a textbook case. Sometimes it starts with just a little itch and a feeling of dread. That’s because your body is already going into shock.
Dr. Mathai from Regional Hospital puts it simply: “If you have hives, wheezing, and trouble breathing after taking a drug, call 911. Don’t wait. Don’t text your doctor. Don’t Google it.”
Even if you’ve taken the medication before without issues, you can suddenly become allergic. Your immune system doesn’t ask for permission.
Why You Shouldn’t Wait
Anaphylaxis doesn’t wait. Symptoms can go from mild to fatal in under 10 minutes. CPR Seattle’s guidelines say it plainly: “If you aren’t sure if symptoms are severe enough to warrant a 911 call, then you should err on the side of caution.”Too many people delay because they think, “It’s probably not that bad,” or “I’ll wait to see if it gets worse.” But by then, it’s often too late. The Food Allergy Research & Education organization reports that half of all fatal anaphylaxis cases happen because epinephrine was given too late-or not at all.
And here’s something most people don’t know: even if you use an epinephrine auto-injector (like an EpiPen), you still need to call 911. One dose might not be enough. Symptoms can come back hours later-a “biphasic reaction.” That’s why emergency responders are trained to monitor you for at least 4 to 6 hours after an episode.

When It’s Safe to Call Your Doctor
If your reaction is limited to one system, and you’re not feeling like you’re going to pass out, you can usually wait to contact your doctor or visit urgent care.Examples of reactions that don’t require 911:
- A mild rash or hives with no breathing trouble or swelling
- Itching without other symptoms
- Mild nausea or diarrhea that doesn’t come with dizziness or a rash
- Headache or fatigue that started after a new medication
Dr. Payel Gupta, an allergist with the American College of Allergy, Asthma, and Immunology, says: “Nausea and vomiting on their own? That’s common. But if you have hives plus vomiting? That’s a red flag.”
If you’re unsure, take a picture of the rash, note the time you took the medication, and call your doctor. They can help you decide if it’s safe to wait or if you need to head to the ER.
What to Do If You Have an Epinephrine Auto-Injector
If you’ve been prescribed an EpiPen, Auvi-Q, or another epinephrine device, keep it with you at all times. Don’t leave it in your car, in a drawer, or in your purse at home.Use it at the first sign of a severe reaction. Don’t wait for symptoms to get worse. Epinephrine is safe-even for older adults or people with heart conditions. The risk of not using it is far greater than any side effect from the drug itself.
After using it:
- Call 911 immediately.
- Tell the dispatcher you’ve used epinephrine for a suspected allergic reaction.
- Ask for an ambulance with epinephrine on board.
- Go to the ER-even if you feel better.
Some people think, “I used the EpiPen, so I’m fine.” That’s a dangerous myth. Emergency care is still required. You need to be monitored for rebound symptoms.
What to Bring to the ER or Doctor’s Visit
If you go to the hospital or see your doctor after a reaction, bring:- The medication you took (or its bottle)
- A list of all other drugs and supplements you’re taking
- When you took the medication and when symptoms started
- Any photos of the rash or swelling
This helps your doctor figure out what caused it. Many people don’t realize that even over-the-counter meds, herbal supplements, or contrast dyes used in imaging tests can trigger reactions.
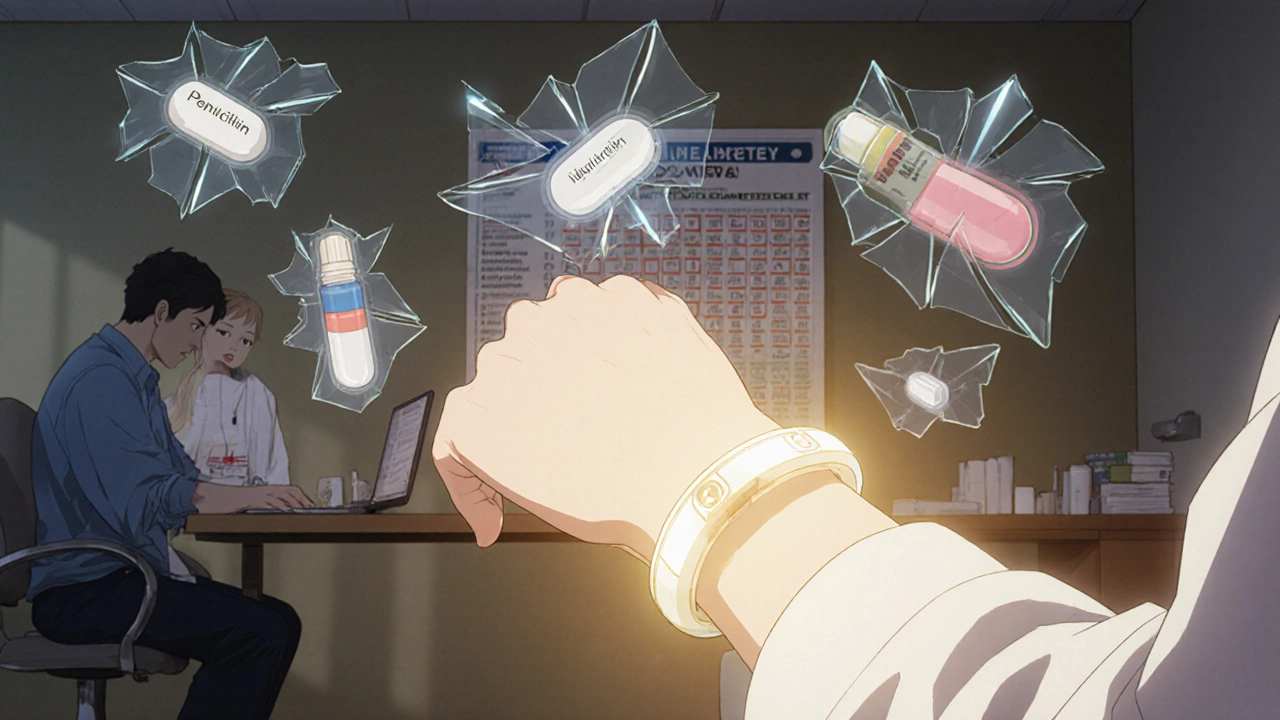
Common Medications That Cause Reactions
Some drugs are more likely to cause allergic reactions than others. According to the American College of Allergy, Asthma, and Immunology, antibiotics like penicillin and sulfa drugs are the most common culprits, accounting for about 15% of all reported drug allergies.Other common triggers include:
- NSAIDs (like ibuprofen or aspirin)
- Chemotherapy drugs
- Seizure medications
- Insulin and other injectables
- Contrast dyes used in CT scans or MRIs
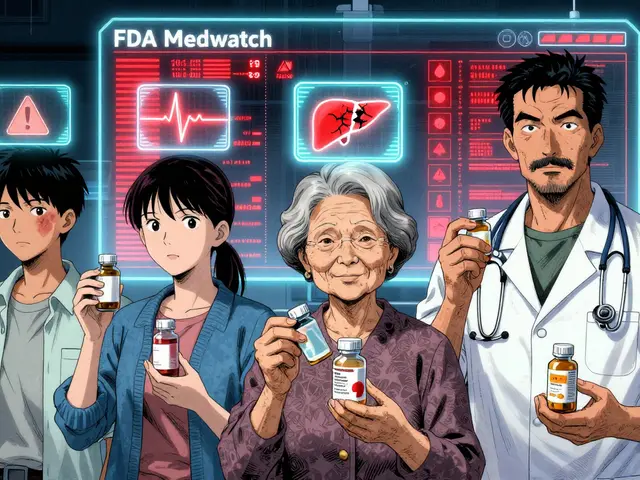
But reactions can happen with any medication-even ones you’ve taken for years. That’s why it’s important to report every new reaction, no matter how small.
How to Prevent Future Reactions
Once you’ve had a reaction, you need to take steps to avoid it in the future:- Ask your doctor to document the reaction in your medical file
- Wear a medical alert bracelet that lists your drug allergies
- Keep a written list of all medications you’re allergic to-and share it with every new provider
- Ask for allergy testing if you’re unsure what caused the reaction
Many people avoid going to the allergist because they think, “I already know what made me sick.” But sometimes, it’s not the drug itself-it’s a filler, dye, or preservative in the pill. Testing can help you avoid unnecessary restrictions and identify safer alternatives.
Bottom Line: When in Doubt, Call 911
There’s no shame in calling emergency services. It’s better to be safe than sorry. Emergency responders are trained to handle these situations. They won’t judge you for being cautious.Medication reactions are serious-but they’re also preventable if you act fast. Know the signs. Keep your epinephrine handy. And never wait to see if symptoms get worse.
If you’re ever unsure, ask yourself: “Could this be affecting my breathing, heart, or ability to stay awake?” If the answer is yes, call 911. Right now. Don’t wait. Don’t text. Don’t call your doctor first. Emergency care saves lives.
Can I just wait and see if my medication reaction gets worse?
No. If you have symptoms like trouble breathing, swelling, dizziness, or a rapid heartbeat, waiting could be deadly. Anaphylaxis can progress from mild to life-threatening in under 10 minutes. Even if symptoms seem mild at first, they can suddenly worsen. If you’re unsure, call 911 immediately.
What if I use my EpiPen and feel better-do I still need to go to the hospital?
Yes. One dose of epinephrine may not be enough. Symptoms can return hours later in what’s called a biphasic reaction. Emergency rooms have the tools and staff to monitor you for at least 4 to 6 hours. Skipping this step puts you at risk of a second, potentially fatal reaction.
Are all rashes from medications dangerous?
Not all rashes are dangerous. A mild, itchy rash with no swelling, breathing issues, or vomiting is usually not an emergency. But if the rash spreads quickly, is accompanied by hives, fever, blistering, or swelling, or if you feel unwell, call 911. A rash combined with other symptoms is a red flag for a serious allergic reaction.
Can I have a reaction to a medication I’ve taken before without problems?
Yes. Your immune system can suddenly start reacting to a drug you’ve taken safely for years. This is especially common with antibiotics, NSAIDs, and chemotherapy drugs. Never assume you’re “immune” to a reaction just because you’ve taken the drug before.
How long after taking a medication can a reaction happen?
Serious reactions like anaphylaxis usually happen within minutes to an hour after taking the drug. But some delayed reactions, like DRESS syndrome or serum sickness, can take days or even weeks to show up. If you develop a rash, fever, or joint pain days after starting a new medication, contact your doctor-even if you thought the reaction was over.
Is epinephrine safe for older adults or people with heart conditions?
Yes. While epinephrine can raise heart rate and blood pressure, the risk of not using it during anaphylaxis is far greater. Medical guidelines from the American Heart Association and the National Institute of Allergy and Infectious Diseases state that epinephrine should still be used in elderly patients and those with heart disease. The danger of untreated anaphylaxis outweighs the risks of the medication.
What should I do if I think I had a reaction but didn’t take any new medication?
Reactions can be triggered by things you don’t expect: new supplements, herbal remedies, over-the-counter painkillers, or even contrast dye used in imaging tests. If you’re unsure what caused it, bring a list of everything you’ve taken in the past 72 hours to your doctor. Even vitamins and teas can cause reactions in some people.
Can I get tested to find out what drug I’m allergic to?
Yes. Allergists can perform skin tests or blood tests to identify specific drug allergies. This is especially helpful if you’ve had a serious reaction and need to avoid certain medications in the future. Testing can also reveal whether the reaction was truly allergic or just a side effect-so you don’t unnecessarily avoid safe drugs.



Comments (8)
Alyssa Torres
Y’all I just had a mild rash after taking ibuprofen last week and I panicked so hard I called 911. They showed up, checked me out, laughed a little, and said ‘you’re fine, but good job not waiting.’ I felt like a drama queen… until I read this post. Now I’m not ashamed. If your body says something’s off, listen. No one ever died from calling 911 too early.
Epinephrine auto-injector in my purse 24/7 now. No excuses.
Summer Joy
OMG I KNEW IT 😭 I took amoxicillin in 2020 and got a rash but didn’t call 911 because I thought it was ‘just a reaction’… and then I got DRESS syndrome. Spent 3 weeks in the hospital. My skin was PEELING. I didn’t even know that was a thing. THIS POST IS A LIFESAVER. WHY DOESN’T EVERYONE KNOW THIS?!?!!?!
Aruna Urban Planner
The distinction between systemic and localized immune responses is clinically significant. While mild cutaneous manifestations often reflect pharmacodynamic idiosyncrasies, the emergence of multi-organ involvement-particularly respiratory or cardiovascular compromise-indicates a Type I hypersensitivity cascade with potential for anaphylactic shock.
Delayed-onset reactions such as DRESS syndrome involve T-cell-mediated inflammation, typically peaking 2–6 weeks post-exposure. This necessitates longitudinal monitoring, not merely acute intervention. The absence of immediate symptoms does not imply safety; it implies latency.
Pharmacovigilance requires patient education not just on symptoms, but on temporal patterns of immune activation. The ‘wait and see’ mentality is a cognitive bias rooted in availability heuristic-people underestimate risk because they’ve never seen it happen to them. But biology doesn’t care about your anecdotal evidence.
Nicole Ziegler
me: *takes new pill*
my body: 🚨🚨🚨
me: ‘it’s probably just… indigestion?’
my body: 😭
me: *calls 911*
paramedics: ‘good call’
me: *still alive*
epipen in my sock drawer. never again.
Nosipho Mbambo
Wait… so if I get a little itch after taking a pill, I’m supposed to call 911?!?!?! That’s insane!! I mean, what if everyone did that?! Hospitals would be flooded with people who just have a tingly arm!! I’ve taken penicillin 5 times and never had an issue!! Why are we turning everything into a medical emergency now?!?!?!
Katie Magnus
Why are we treating every little rash like a horror movie? I had a rash from Advil once and I just took Benadryl. I didn’t need 911. This post is fearmongering. People are dying from anxiety, not allergies. Stop making everyone paranoid.
King Over
Been on antibiotics for 12 years. Never had a reaction. Don't need a lecture. Just take the pill. If you feel weird, stop. Simple. No drama. No 911 unless you're dying. End of story.
Johannah Lavin
My mom had anaphylaxis from a flu shot in 2018. She didn’t know she was allergic. Thought it was just a bad cold. Took her 20 minutes to realize she couldn’t breathe. She used her EpiPen, called 911, and they saved her.
She’s fine now. But she wears a medical bracelet. She carries two EpiPens. She tells every doctor, every pharmacy, every nurse. And she’s not embarrassed. She’s grateful.
If you’re reading this and you’re scared you’ll look silly for calling 911… just remember: your life is worth more than someone else’s judgment. You don’t owe anyone a ‘normal’ reaction. You owe yourself survival.
And if you’re the one who’s ever said ‘it’s probably nothing’ to someone having a reaction? Stop. Just stop. Be the person who says ‘I’ve got you.’
💛