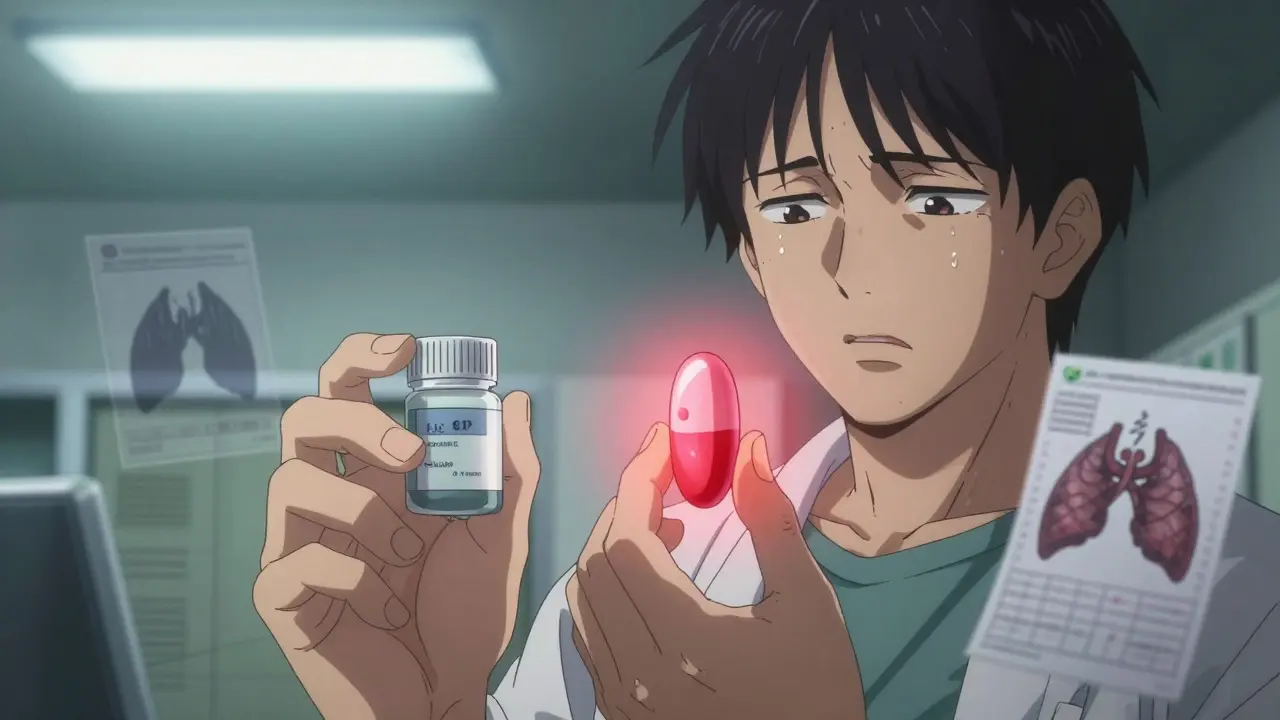
When your pharmacist hands you a new pill that looks completely different from the one you’ve been taking for years, it’s natural to feel uneasy. The color is wrong. The shape is off. The imprint doesn’t match. And suddenly, you’re not sleeping. Or your seizures are coming back. Or your anxiety has spiked. You didn’t change your dose. You didn’t stop taking it. You just switched to a generic version.
This isn’t rare. In fact, it’s standard practice. Around 90% of prescriptions filled in the U.S. are for generic drugs. They’re cheaper, often 80% less than brand-name versions, and the FDA says they’re just as safe and effective. But for some people-especially those on certain high-risk medications-switching generics isn’t harmless. It can trigger real, sometimes dangerous, side effects.
Why Do Generic Switches Cause Problems?
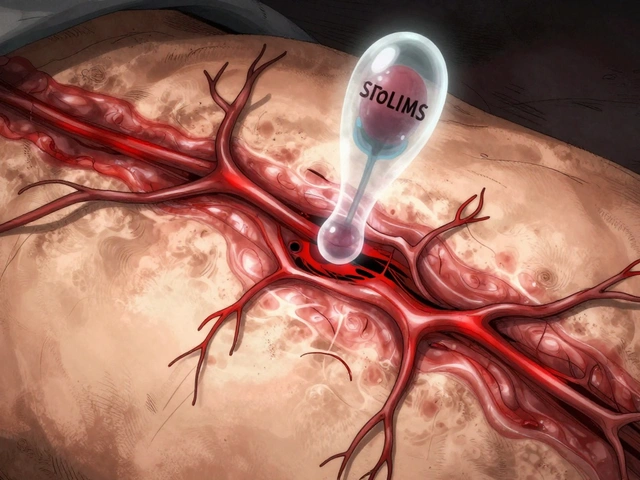
The FDA requires generics to contain the same active ingredient as the brand-name drug and to be bioequivalent, meaning they must deliver 80% to 125% of the drug’s concentration in your bloodstream compared to the brand. On paper, that sounds fine. But here’s the catch: that 45% total range (from 80% to 125%) can mean big differences for people who are extremely sensitive to small changes in drug levels.
Think of it like this: if you’re taking a medication where even a 10% drop in blood levels causes your condition to flare up, then switching from a generic that delivers 85% to one that delivers 115% could mean your body is getting nearly 35% more or less of the drug. That’s not a minor fluctuation. That’s enough to trigger a seizure, a blood clot, or a psychotic episode.
These risks aren’t theoretical. They’re documented. A 2019 study in BMJ Open found that patients with heart disease who switched between different generic versions of the same drug had a 12.3% higher chance of being hospitalized within 30 days. That’s not a small number. That’s one in eight people.
Which Medications Are Most Likely to Cause Problems?
Not all drugs are created equal when it comes to switching. Some are forgiving. Others aren’t. The FDA calls these high-risk medications “narrow therapeutic index” (NTI) drugs. That means the difference between a safe dose and a toxic one is tiny.
Here are the top five categories where switching generics can be risky:
- Antiepileptics (like phenytoin, levetiracetam, divalproex): Even small changes in blood levels can cause breakthrough seizures. A 2021 survey of 147 neurologists found that 68.7% believed generic switches increased seizure risk.
- Thyroid meds (like levothyroxine): Too little and you’re fatigued and gaining weight. Too much and your heart races, you lose bone density, and you risk atrial fibrillation. One study showed patients switching between generic levothyroxine brands had abnormal TSH levels in over 30% of cases.
- Anticoagulants (like warfarin): A slight increase in blood levels can cause dangerous bleeding. A drop can lead to a stroke. Warfarin is especially tricky because it interacts with so many other drugs and foods-adding formulation changes makes it even harder to control.
- Immunosuppressants (like tacrolimus and cyclosporine): After an organ transplant, your body is on a tightrope. Too little drug and your body rejects the new organ. Too much and you get kidney damage or infections. Studies show switching these generics increases rejection risk by up to 15%.
- Psychiatric meds (especially extended-release ADHD drugs like Adderall XR or bupropion XL): Patients report sudden return of symptoms, new anxiety, insomnia, or mood swings within 24 to 72 hours of switching. One Reddit thread with 842 comments found 78% of users had negative experiences after switching generic Adderall.
These aren’t edge cases. These are people who rely on these drugs to function, to survive. And when their medication changes without warning, their health can unravel.
Why Do Pharmacists Keep Switching Them?
It’s not about your health. It’s about money.
Pharmacy benefit managers (PBMs)-companies like CVS Caremark, Express Scripts, and OptumRx-control which generics pharmacies stock. They don’t pick based on safety or consistency. They pick based on rebates. The manufacturer that offers the biggest kickback gets the contract. That means your pharmacy might switch your generic every few months, sometimes even every refill, just to get paid more.
A 2022 Senate investigation found PBMs change preferred generic manufacturers an average of 4.7 times per year per drug. For someone on a monthly medication, that’s nearly five different pills in a year. And you might not even know.
Levothyroxine alone has 12 approved generic manufacturers. Each one uses a different filler, coating, or release mechanism. The FDA allows this. But your body doesn’t care about the paperwork. It cares about what’s in the pill-and how it gets absorbed.

What Are the Real Symptoms People Experience?
Patients aren’t imagining this. Thousands have reported consistent patterns after switching:
- ADHD meds: Loss of focus, irritability, fatigue, new-onset anxiety, insomnia, headaches. One study found 63.2% of patients noticed decreased effectiveness after a manufacturer switch.
- Thyroid meds: Weight gain, cold intolerance, brain fog, hair loss, heart palpitations. One patient described it as “feeling like I was drowning in slow motion.”
- Antiseizure meds: Sudden seizures, aura episodes, confusion, dizziness. One woman had her first seizure in 12 years after switching to a new generic phenytoin.
- Anticoagulants: Bruising easily, nosebleeds, blood in urine, dizziness. One man ended up in the ER with a brain bleed after his warfarin generic changed.
- Immunosuppressants: Fever, swelling, pain at transplant site, elevated liver enzymes. Transplant patients have been hospitalized after switching generics.
And it’s not just about the drug itself. Some patients get confused by the new pill’s appearance and accidentally take two doses. A 2023 hospital study found 11.5% of patients didn’t recognize their medication after a switch-and 20% of those who duplicated their dose ended up with serious side effects, including serotonin syndrome.
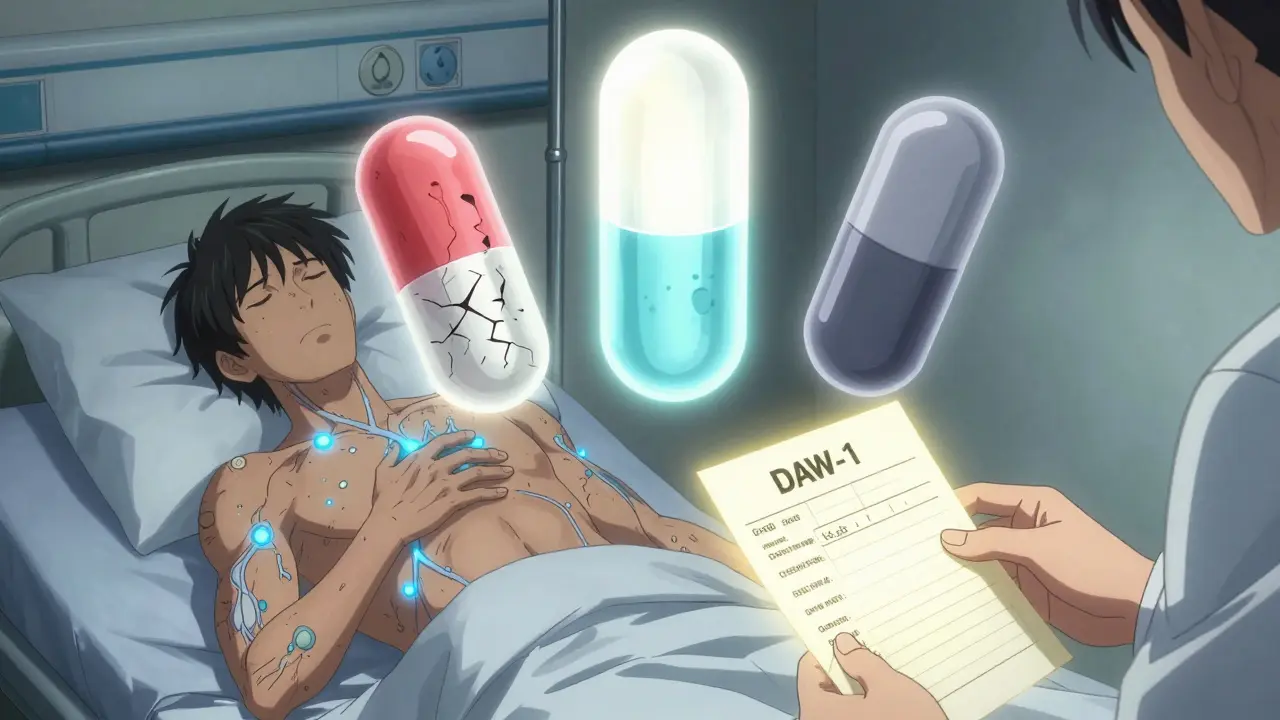
What Should You Do If You Think Your Generic Is Causing Problems?
If you notice new or worsening symptoms after switching to a generic, don’t ignore it. Don’t assume it’s “just in your head.” Here’s what to do:
- Check the pill. Look at the color, shape, and imprint. Write down the name on the pill. Compare it to your last refill. If it’s different, that’s your clue.
- Check the NDC code. It’s on the bottle. Write it down. If it changes, your manufacturer changed. That’s not random-it’s a switch.
- Call your doctor. Tell them exactly when the change happened and what symptoms started. Don’t say “I think it’s the generic.” Say: “I switched to a new generic on [date] and since then I’ve had [symptoms].”
- Ask for a DAW-1 prescription. That means “dispense as written.” It tells the pharmacist not to substitute. You have the right to request this, especially for NTI drugs.
- Ask for a specific manufacturer. If your doctor agrees, ask them to write: “Do not substitute” or specify the brand name of the generic (e.g., “Teva levothyroxine” or “Actavis Adderall XR”). Pharmacies can often order it.
- Keep a log. Track your medication: date, manufacturer, dose, symptoms. This helps your doctor spot patterns.
A 2021 study showed patients who got counseling from a pharmacist about switching risks were 37% less likely to have bad outcomes. Knowledge is power.
What’s Being Done to Fix This?
There’s growing pressure to change. In 2023, Medicare Part D rules limited generic switches to no more than twice a year. The FDA launched a $15.7 million initiative to improve testing for complex generics like extended-release pills and inhalers. In January 2024, the American Society of Health-System Pharmacists published new guidelines advising against automatic substitution for 17 specific drugs, including tacrolimus, bupropion XL, and phenytoin.
Some hospitals are even using “medication fingerprinting”-keeping patients on the same generic manufacturer long-term. One system cut switching-related problems by over 50%.
But the system still favors cost over consistency. The $165 billion in annual savings from generics is real. But so is the $2.1 billion spent each year on preventable hospitalizations from bad switches.
Final Thought: You Have a Right to Stability
Generic drugs saved millions of people money. That’s good. But no one should have to risk their health because of a rebate deal.
If you’re on a high-risk medication, your stability matters more than a few dollars. You’re not being difficult. You’re being smart. You’re paying attention to your body-and that’s the most important thing.
Ask for the same manufacturer. Ask for a DAW-1. Ask your pharmacist to call your doctor. If they push back, ask to speak to the pharmacist-in-charge. You’re not asking for a luxury. You’re asking for the same treatment you had before.
And if you’ve been switched and you’re feeling off? Don’t wait. Speak up. Your life might depend on it.
Can switching to a generic drug really cause serious side effects?
Yes, for certain medications-especially those with a narrow therapeutic index like antiepileptics, thyroid hormones, blood thinners, immunosuppressants, and extended-release psychiatric drugs-switching between generic manufacturers can lead to real side effects. These include breakthrough seizures, unstable thyroid levels, dangerous bleeding, organ rejection, or sudden return of anxiety and ADHD symptoms. While the FDA considers generics bioequivalent, small differences in how the drug is absorbed can trigger problems in sensitive individuals.
Which generic drugs are most likely to cause problems when switched?
The highest-risk categories include antiepileptic drugs (like phenytoin and divalproex), levothyroxine (thyroid hormone), warfarin (blood thinner), tacrolimus and cyclosporine (transplant drugs), and extended-release ADHD medications like Adderall XR and bupropion XL. These drugs require very precise blood levels, and even small changes in absorption can lead to treatment failure or toxicity.
Why do pharmacies keep switching my generic medication?
Pharmacies switch generics because pharmacy benefit managers (PBMs) pay them rebates to use certain manufacturers. The PBM chooses the cheapest option with the highest rebate-not the most consistent or safest. This means your medication might change every few months, even if you’ve been stable on one version. It’s a business decision, not a medical one.
How can I stop my generic medication from being switched?
Ask your doctor to write a prescription with “DAW-1” (dispense as written) or specify the manufacturer name (e.g., “Teva levothyroxine”). You can also request the same generic brand each time by checking the NDC code on your bottle. If your pharmacy refuses, ask to speak to the pharmacist-in-charge-they often have the authority to order a specific brand.
What should I do if I think my new generic is making me sick?
Track your symptoms and the date you started the new pill. Note the manufacturer name from the NDC code on your bottle. Call your doctor immediately and say: “I switched to a new generic on [date] and since then I’ve had [symptoms].” Don’t wait. Bring your pill bottle to your appointment. You may need to switch back or get a DAW-1 prescription to prevent future changes.
Is it legal for a pharmacy to switch my generic without telling me?
Yes, unless your prescription says “DAW-1” or specifies a brand, pharmacists are allowed to substitute generics without notifying you. This is standard under state substitution laws. But you have the right to refuse the substitution and request the original brand or manufacturer. Always check your pill before leaving the pharmacy.
Are brand-name drugs safer than generics?
Not necessarily. Brand-name and generic drugs contain the same active ingredient and must meet the same FDA standards for safety. The difference lies in the inactive ingredients and manufacturing processes, which can affect how the drug is absorbed. For most people, generics are perfectly safe. But for those on high-risk medications, the consistency of one manufacturer may be safer than switching between multiple generics.
Stability in medication isn’t a luxury. It’s a necessity. If your body has adapted to a specific formulation, changing it without warning isn’t just inconvenient-it can be dangerous. You’re not alone in this. Thousands have been through the same thing. And you have the right to demand consistency.

Comments (10)
Mike Berrange
I've been on levothyroxine for 12 years. Switched generics last month. Suddenly my heart was racing, I couldn't sleep, and I gained 8 pounds in two weeks. My doctor said it was 'probably stress.' I showed him the bottle. He called the pharmacy. They switched me back. Don't let them gaslight you. This isn't placebo. It's real.
Nishant Garg
In India, we don't have this problem-because generics are the only option. But here’s the twist: we have 20+ brands of levothyroxine, and people stick to one. Why? Because their body remembers. Your body isn’t a spreadsheet. It doesn’t care about FDA bioequivalence percentages. It cares about consistency. If your thyroid meds feel different, they are different. And yes, your doctor should listen.
Amy Ehinger
I used to work at a pharmacy. We had to switch generics based on what the PBM told us. No warning. No notice. I saw patients cry because their seizure meds changed and they had a breakthrough episode. I quit after that. The system is broken. It’s not about safety-it’s about who gave the biggest rebate this quarter. And we’re the ones who have to clean up the mess.
Crystel Ann
This post saved my life. I thought I was losing my mind after switching Adderall generics. I was crying for no reason, couldn’t focus, felt like I was underwater. I didn’t know it was the pill. I thought I was just depressed. Reading this made me realize I wasn’t crazy. I called my doctor. We got the DAW-1. I’m back to normal. Thank you.
Frank Geurts
It is imperative to note, with the utmost seriousness, that the FDA's bioequivalence standards-while statistically acceptable-are not physiologically uniform across all patient populations. The 80–125% range, though mathematically compliant, permits a 45% variance in systemic exposure, which is clinically significant for narrow-therapeutic-index agents. The current regulatory framework prioritizes cost-efficiency over patient-specific pharmacokinetic stability. This constitutes a systemic failure in pharmacovigilance, and legislative reform is not merely advisable-it is an ethical imperative.
Nilesh Khedekar
Oh wow, so you’re telling me that capitalism isn’t perfect? Shocking. I mean, who knew that corporations would choose profit over people? Next you’ll tell me water is wet. I’ve been on warfarin for 15 years. Switched generics. Started bleeding out of my gums. Went to the ER. The pharmacist said, ‘It’s probably just your diet.’ I asked for the old one. They said, ‘We don’t stock it.’ I paid $12 extra to get it from another pharmacy. My insurance didn’t care. Neither did the FDA. But I’m alive. So… congrats, system. You win.
Jami Reynolds
This is all a setup. The FDA, PBMs, and Big Pharma are working together to make you dependent on expensive brand drugs by making generics unreliable. Then they’ll say, ‘See? You need the brand.’ That’s how they get you hooked. They’ve been doing it since the 80s. They even control the NDC codes. I’ve seen the documents. They’re not random switches. They’re targeted. They want you to panic. Then they sell you the brand. Don’t fall for it. Demand transparency. Or they’ll keep doing this to you.
RUTH DE OLIVEIRA ALVES
As a clinical pharmacist with over two decades of experience, I can confirm that the variability in generic formulations-particularly for extended-release and NTI drugs-is not adequately tracked in real-world settings. The FDA’s approval process is based on average bioequivalence, not individual patient response. We have documented cases where patients experienced clinically significant fluctuations after switching manufacturers, even within the same generic brand. The solution is not to eliminate generics-it is to implement mandatory manufacturer tracking, patient education, and pharmacist-led substitution protocols. This is a solvable problem.
Arjun Seth
You people are weak. My grandfather took five different generics at once and lived to 98. You think your body is special? It’s not. You’re just lazy. Stop whining. Take the pill. Get over it. If you can’t handle a different color, you shouldn’t be on medication. The system works. You’re just too soft to use it.
Dan Mack
They’re putting microchips in the fillers. That’s why the side effects are so weird. The same company makes the Adderall and the new generic. They’re testing behavioral responses. You think your seizures are from the pill? Nah. It’s the AI in the coating. They’re mapping your brainwaves. I know this because I read it on a forum. And my cousin’s neighbor’s dog got sick after a pill change too. Coincidence? I think not.