
Polypharmacy Risk Calculator
How Many Medications Are You Taking?
Polypharmacy is defined as taking five or more medications regularly. This calculator helps you understand potential risks based on your medication count.
Your Medication Risk Assessment
Key Risks at This Level
What You Should Do
Important Safety Note
Never stop medications without consulting your doctor. This tool provides risk information only—do not make treatment changes based on this alone.
When you’re taking five or more medications every day, it’s not just a routine-it’s a risk. Polypharmacy, the term for using five or more drugs at once, is common among older adults and people with chronic conditions. But what looks like proper medical care can actually be putting your health in danger. The problem isn’t always the drugs themselves-it’s how many are piled on top of each other, often without a clear plan.
Why More Medications Don’t Mean Better Health
Many people assume that if a doctor prescribes a medication, it must be necessary. But the truth is, not every pill you take is helping you. In fact, some might be making things worse. A 2016 study in BMJ Open found that people taking 10 or more medications had a 28% higher chance of dying than those taking just one to four. That’s not because the drugs are dangerous on their own-it’s because they interact, overload your body, and cause side effects that lead to new prescriptions. Take a 72-year-old woman with high blood pressure, arthritis, and mild depression. She’s on a beta-blocker, an NSAID, an antidepressant, a statin, a diuretic, a calcium supplement, and a sleep aid. Each one was prescribed for a separate issue. But together, they’re causing dizziness, confusion, and muscle weakness. Her doctor then prescribes a balance medication for the dizziness-and now she’s on eight pills. This is called a medication cascade: one side effect leads to another drug, which causes another problem. Studies show 30-40% of inappropriate prescriptions in older adults start this way.The Real Cost of Too Many Pills
It’s not just your body that suffers. Your wallet does too. In 2022, Medicare data showed that people taking five to nine medications spent an average of $317 per month on drugs. Those taking just one to four paid $78. For someone on a fixed income, that’s the difference between eating well and skipping meals. One patient in California told a clinic he was choosing between his heart medication and groceries. He was taking 12 pills a day-and still couldn’t afford them all. And it’s not just money. A 2021 study in the Journal of General Internal Medicine found that patients on 10 or more medications were 3.2 times more likely to miss doses. Why? Complexity. If you can’t remember whether you took your 8 a.m. pill or your 2 p.m. one, you’ll skip them. Cost and confusion are the top two reasons people stop taking their meds. Side effects come in third.How Polypharmacy Hits Your Body
Your body doesn’t handle drugs the same way when you’re older. Liver and kidney function slow down. Your muscles shrink. Your brain becomes more sensitive to certain chemicals. That means a dose that was safe at 50 might be dangerous at 75. The most common side effects from polypharmacy include:- Falls and fractures (risk increases 1.5 to 2 times with five or more meds)
- Confusion and memory problems (often mistaken for dementia)
- Extreme fatigue or dizziness
- Stomach bleeding from NSAIDs mixed with blood thinners
- Low sodium levels from diuretics and antidepressants combined
What’s the Difference Between Good and Bad Polypharmacy?
Not all multiple medications are bad. Sometimes, you need them. For example, after a heart attack, patients are often put on four drugs: a beta-blocker, a statin, an antiplatelet, and an ACE inhibitor. This combination has been shown to cut death risk by 50-60%. That’s appropriate polypharmacy: targeted, evidence-based, and necessary. Inappropriate polypharmacy is when you’re taking drugs that don’t help-or even hurt. Examples include:- Taking two different painkillers that do the same thing
- Staying on a sleeping pill for years after insomnia is gone
- Prescribing an anticholinergic for allergies when a safer alternative exists
- Keeping a medication that was only meant for short-term use
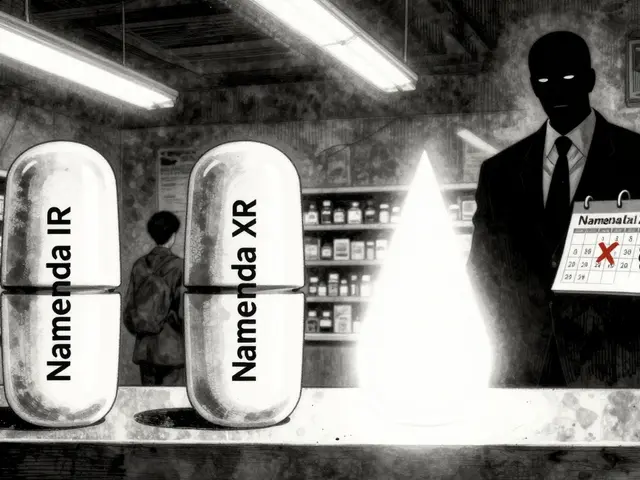
Deprescribing: The Quiet Revolution in Medicine
There’s a growing movement called deprescribing-the careful, planned reduction or stopping of medications that are no longer needed or are doing more harm than good. It’s not about cutting pills randomly. It’s about reviewing every drug with a clear goal: improve safety, reduce side effects, and restore quality of life. The process takes time. Most patients need 3 to 6 months to safely reduce their meds. A 2020 study found that doctors spend 25 to 40 minutes per patient just reviewing their full list-something rarely done in a typical 15-minute appointment. Here’s how it works:- Make a complete list of everything you take-prescriptions, over-the-counter drugs, vitamins, supplements.
- Check each one: Why was it prescribed? Is it still needed? Is it safe with your other meds?
- Use tools like the Beers Criteria to flag risky drugs.
- Start with the most dangerous or least necessary ones first.
- Reduce slowly. Stop one at a time. Watch for changes.
What You Can Do Right Now
You don’t need to wait for your doctor to bring it up. You can take control today:- Bring every pill bottle to your next appointment-even the ones you haven’t taken in months.
- Ask: “Is this still helping me? Could it be causing any of my symptoms?”
- Ask about alternatives: “Is there a safer drug or a non-drug option?”
- Request a full medication review if you’re on five or more drugs.
- Use a pill organizer-but only if you know what’s in it.

The Bigger Picture: Why This Is a System Failure
Polypharmacy isn’t just about individual choices. It’s a system problem. Most doctors don’t get enough training in managing complex medication regimens. Only 12% of medical schools in the U.S. have a dedicated course on polypharmacy. Primary care doctors report that only 28% have systems in place to track complex drug lists. The FDA approved its first deprescribing decision tool, MedWise, in 2022. It flagged dangerous combinations and reduced risky drug pairs by 37% in early trials. But tools like this aren’t widely used yet. The cost of inaction is huge. Polypharmacy causes $300 billion in avoidable healthcare spending each year in the U.S. That includes hospital stays, ER visits, and long-term care. Patients on multiple drugs have 24% more hospital admissions and 32% more emergency visits than those on fewer meds.It’s Not About the Number-It’s About the Need
Some experts argue that focusing on the number five is arbitrary. The real question isn’t “How many pills?” but “Are these pills helping you live better?” A 70-year-old with heart failure, diabetes, and kidney disease might need seven medications to stay alive. That’s not polypharmacy-it’s life-saving care. But a 75-year-old taking a daily sleep pill, an antacid, a muscle relaxant, a vitamin D, a calcium supplement, and a cholesterol drug-all because they were added over time without review-that’s the problem. The goal isn’t to take fewer pills. It’s to take the right ones.What Happens When You Don’t Act
Without changes, the problem will only get worse. By 2035, researchers predict polypharmacy will increase adverse drug events by 40% and add $127 billion to annual healthcare costs. But change is possible. The American Geriatrics Society’s “Choosing Wisely” campaign reduced inappropriate prescribing by 22% in just two years. Patients who worked with their doctors to deprescribe reported better sleep, more energy, and fewer falls. The message is clear: More pills don’t mean better health. Sometimes, less is more.What is considered polypharmacy?
Polypharmacy is generally defined as taking five or more medications regularly. But the real issue isn’t the number-it’s whether each medication is still necessary, safe, and helping you. Some people need more than five for serious conditions; others take far too many that do more harm than good.
Can polypharmacy cause falls in older adults?
Yes. Taking five or more medications increases the risk of falls by 1.5 to 2 times. Common culprits include sedatives, blood pressure drugs, antidepressants, and painkillers. These can cause dizziness, low blood pressure, or confusion-making falls more likely. Falls often lead to fractures, hospital stays, and loss of independence.
How do I know if I’m taking too many medications?
Ask yourself: Do I feel worse since I started taking more pills? Do I have side effects like dizziness, confusion, fatigue, or stomach upset? Do I skip doses because the regimen is too complicated? If you’re on five or more meds, ask your doctor for a full review. Bring all your pills-even supplements-to your appointment.
What is deprescribing?
Deprescribing is the planned, gradual reduction or stopping of medications that are no longer needed, are harmful, or are causing side effects. It’s done under medical supervision to avoid withdrawal or worsening of conditions. It’s not about cutting pills cold turkey-it’s about removing what’s unnecessary to improve safety and quality of life.
Can I stop my meds on my own if I think they’re causing side effects?
No. Stopping some medications suddenly can be dangerous-like blood pressure pills, antidepressants, or seizure drugs. Always talk to your doctor or pharmacist first. They can help you safely adjust your regimen. If you suspect a side effect, write down what you’re feeling and when it started. That helps your provider connect the dots.
Are over-the-counter drugs and supplements part of polypharmacy?
Absolutely. Many people don’t realize that OTC painkillers like ibuprofen, sleep aids like diphenhydramine, or even herbal supplements like St. John’s Wort can interact with prescription drugs and cause side effects. These should be included in any medication review. A pill you buy at the grocery store can be just as risky as a prescription.


Comments (11)
Eileen Reilly
i swear my grandma takes 14 pills a day and still says she's fine. last week she fell and broke her hip and the dr just added another med for 'balance issues'. classic cascade. why not just take away the 4 that make her zombified?
Monica Puglia
this hit so hard 😔 my mom’s on 9 meds and she forgets half of them. i started putting them in a pill organizer with color-coded times... but then she stopped taking the blue ones because 'they made her mouth dry'. we’re scheduled for a med review next month. i’m nervous but hopeful. 🙏
steve ker
polypharmacy is just lazy medicine. doctors dont want to think so they prescribe. easy fix: stop writing scripts like its a vending machine
Rebekah Cobbson
i work in geriatric care and i see this every day. the saddest part? most patients don’t even know why they’re on half the meds. if you’re on 5+ drugs, ask for a med reconciliation. pharmacists can help. seriously. they’re the unsung heroes here.
Rinky Tandon
the systemic failure is palpable. polypharmacy is not merely a pharmacological phenomenon-it’s a manifestation of biomedical reductionism in an aging population devoid of holistic care infrastructure. the Beers Criteria are a band-aid on a hemorrhaging artery. deprescribing requires paradigmatic reorientation, not just clinical protocols.
Darryl Perry
This is why we need mandatory continuing education for physicians on geriatric pharmacology. 12% of med schools teach it? That’s unacceptable. The FDA tool is a start but it’s not being used. Hospitals need centralized med reconciliation teams. End of story.
Windie Wilson
oh honey. my aunt took a vitamin that made her dizzy. so the dr gave her a dizziness pill. then the dizziness pill made her constipated so now she’s on a laxative. and the laxative made her lose potassium so now she’s on a potassium pill. she’s on 11 meds now. i swear the pharmacy has her on a subscription.
Daniel Pate
It's interesting how we equate 'more treatment' with 'better care.' But medicine isn't a stack of blocks. It's a dynamic system. Each drug alters homeostasis. The body doesn't have infinite buffering capacity. We treat symptoms without seeing the cascade. We're not curing-we're managing side effects of side effects. Is that healing? Or just noise?
Amanda Eichstaedt
i had a friend who was on 13 meds after a minor stroke. she was confused all the time. her kids brought her to a geriatric pharmacist who did a full review. cut out 5-sleep aid, antacid, muscle relaxer, two vitamins that did nothing. within 3 weeks she was sleeping better, walking without a cane, and remembered her own birthday. it wasn't magic. it was just stopping the nonsense.
Abner San Diego
this is why america is broke. people take pills like candy and then cry when they get sick. if you're old and taking 5 meds, you're probably just lazy and want to avoid walking. get off your butt. no one cares how much you paid for your supplements.
Cecelia Alta
okay but let’s be real-this isn’t just about doctors. it’s about the whole damn system. insurance doesn’t pay for time. so your doc has 8 minutes to see you. they don’t have time to ask if you still need that 2017 anxiety med. they just refill it. then the pharmacist sees 12 meds and says ‘yep, all good.’ Meanwhile, you’re on a cocktail that could knock out a horse. and don’t even get me started on the OTC stuff. i saw a woman at Walmart buy 3 different sleep aids and a muscle cream and a probiotic and a turmeric pill and a magnesium thing and a fish oil and a glucosamine and a vitamin D and a B12 and a collagen powder. and she’s 67. and she thinks she’s ‘being proactive.’ honey. you’re not a pharmacy. you’re a walking side effect waiting to happen.