Every day, pharmacists hand out millions of generic drugs. In Canada and the U.S., generics make up over 75% of all prescriptions filled. They’re cheaper, widely available, and regulated to be just as safe and effective as brand-name drugs. But what happens when a generic drug doesn’t work the same way for a patient? When someone who’s been stable on a generic for months suddenly has a bad reaction, or their blood pressure spikes, or their seizures return? That’s when the pharmacist’s responsibility kicks in-not just to dispense, but to report.
What Exactly Are Pharmacists Supposed to Report?
Pharmacists aren’t expected to diagnose. But they are expected to notice when something’s off. The FDA defines serious adverse drug events as those that are life-threatening, cause hospitalization, lead to permanent disability, or result in congenital anomalies. But beyond that, there’s another critical category: therapeutic inequivalence.Therapeutic inequivalence means a generic drug isn’t performing like it should-even though it passed FDA bioequivalence tests. A patient might switch from one generic brand to another, or even refill the same generic, and suddenly feel worse. Their medication isn’t working. Their symptoms return. Their lab values shift. These aren’t side effects. These are signs the drug isn’t doing what it’s supposed to do.
The FDA’s MedWatch program specifically asks pharmacists to report these situations. In 2022, the agency added a dedicated "generic drug concern" category to its online reporting form, letting pharmacists flag issues like:
- Therapeutic failure (e.g., seizure control lost after switching generics)
- Unexplained changes in drug levels (e.g., warfarin INR spikes after a generic switch)
- Manufacturing defects (e.g., pills that crumble, change color, or taste different)
- Labeling errors (e.g., wrong dosage printed, missing warnings)
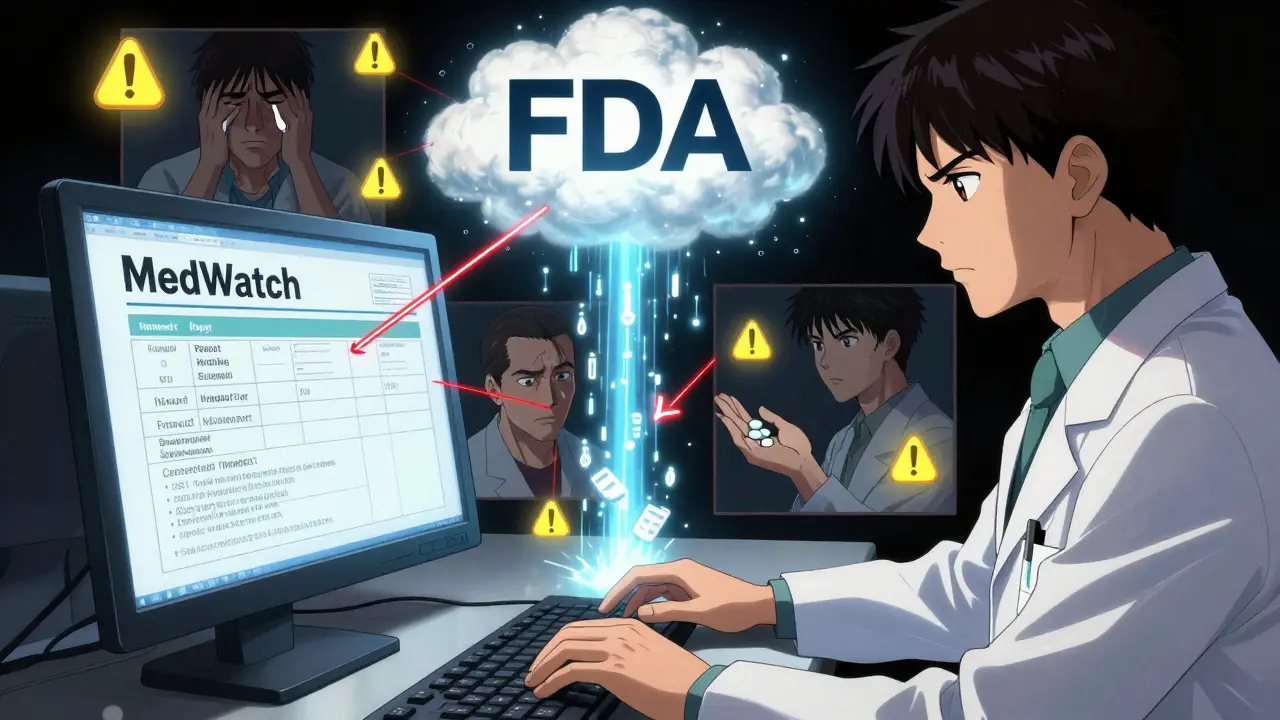
It’s not enough to say, "The patient had a bad reaction." The FDA needs specifics: the patient’s age, the exact drug name, the National Drug Code (NDC), the lot number, and what happened. A vague report gets ignored. A detailed one can trigger a review of the entire product line.
Why Don’t More Pharmacists Report?
In 2023, pharmacists dispensed about 5.8 billion prescriptions in the U.S.-and 75% of those were generics. Yet, only 2.3% of all adverse event reports to the FDA came from pharmacists. That’s a massive gap.Why? Three big reasons.
First, time. Community pharmacists are overwhelmed. Between filling scripts, answering questions, managing insurance issues, and counseling patients, reporting feels like another chore. A 2023 survey found 68.4% of pharmacists say they simply don’t have time to file a report.
Second, uncertainty. Many pharmacists aren’t sure if what they’re seeing is a real problem or just a patient’s fluctuating condition. "Was it the drug? Or did they skip meals? Did they start a new medication?" That doubt stops them from acting.
Third, attribution. When a patient says, "I took my blood pressure pill," they don’t know if it was Aurobindo, Teva, or Mylan. Pharmacists often don’t either-unless they check the label. And if they don’t know the manufacturer, they can’t report it properly. That’s a huge problem because the FDA needs to know which company’s product is causing trouble.
There’s another layer: legal confusion. After the 2011 Supreme Court case PLIVA v. Mensing, generic manufacturers can’t be sued for failing to update warning labels. The law says they must copy the brand-name label exactly. That means if a drug causes harm, the manufacturer can’t change the warning-even if they know about it. So who’s left to speak up? The pharmacist.
What Happens When You Report?
Reporting isn’t just paperwork. It’s a lifeline.In 2022, the FDA’s Office of Generic Drugs received 1,842 reports of therapeutic inequivalence. Of those, 387 came from pharmacists. That’s up from 354 the year before. Those reports led to 147 generic drugs being put under extra review. Twelve of them resulted in direct warnings to prescribers and patients.
One case: A pharmacist in Ohio noticed three patients on the same generic levothyroxine had sudden hypothyroid symptoms. All had been stable for years. All switched to the same new generic batch. The pharmacist filed a report. The FDA reviewed the lot. Turns out, the dissolution rate was off-meaning the drug wasn’t releasing properly in the body. The batch was recalled. Patients were switched back. No one died. But without that report, more people might have.
Pharmacists aren’t just reporters. They’re early warning systems. A 2023 study in JAMA Internal Medicine found that 63% of the 478 generic drugs flagged for potential safety issues were first identified by pharmacists spotting patterns across multiple patients.
State Rules Are Getting Stricter
Federal law doesn’t force pharmacists to report. But some states do.California, Illinois, Massachusetts, and New York now require pharmacists to report serious adverse events. The California State Board of Pharmacy’s 2022 Standard of Care Report says pharmacists must "maintain a system for identifying, documenting, and reporting adverse drug reactions and therapeutic failures."
Other states are following. In 2023, 28 states had some form of reporting expectation written into pharmacy board regulations. The trend is clear: regulators are recognizing that pharmacists are on the front lines. They see what doctors don’t. They hear what patients forget to mention.
How to Report: A Simple Step-by-Step
You don’t need a degree in pharmacovigilance. Here’s how to report in under 10 minutes:- Identify the issue. Did the patient’s condition worsen after switching generics? Did they have a new side effect? Did the pill look or taste different?
- Check the label. Write down the drug name, manufacturer, NDC, and lot number. If you’re unsure, call the wholesaler.
- Document the patient’s story. What symptoms? When did they start? What other meds are they on? Did they miss doses? Did they change diet or lifestyle?
- Go to MedWatch. Visit the FDA’s online portal: www.fda.gov/medwatch. Use Form 3500. Select "Generic Drug Concern" and choose the right category: therapeutic inequivalence, manufacturing issue, or labeling error.
- Submit. You don’t need patient consent to report. The FDA protects patient privacy. If you’re unsure whether it’s serious enough, report anyway. The FDA says: "Report even if you’re not certain the drug caused it."
There’s also a free 30-minute training module on the MedWatch portal. It’s updated every year. Take it. Your state board might require it soon.

Why This Matters More Than You Think
Generic drugs save the U.S. healthcare system over $300 billion a year. But that savings only works if the drugs are safe and effective. If 1 in 100 generic pills doesn’t work right, that’s 58 million pills a year failing patients. That’s not a glitch. That’s a system failure.Pharmacists are the only professionals who see every single generic drug dispensed. We’re the ones who notice when a patient says, "This one doesn’t feel right." We’re the ones who catch the pattern before it becomes an outbreak.
When you report, you’re not just helping one patient. You’re helping thousands. You’re telling the FDA: "This batch is bad." "This manufacturer needs to fix this." "This generic isn’t interchangeable."
And if you don’t report? No one else will. Manufacturers aren’t incentivized to report their own failures. Doctors rarely know what generic a patient got. Patients don’t know how to report. That leaves you.
What’s Holding You Back? Let’s Fix It
If you’re not reporting, here’s what you can do today:- Put a checklist on your counter: "Did the patient report a change? Check NDC and lot. Report if unsure."
- Ask every patient who switches generics: "How’s it going? Any different from before?"
- Keep a log of any unusual reactions-even if you don’t report them yet. Patterns emerge over time.
- Talk to your pharmacy manager. Ask if your pharmacy tracks adverse events. If not, suggest it.
- Use the FDA’s free training. It’s online. It takes 30 minutes. You’ll know exactly what to look for.
You don’t need to be perfect. You just need to be consistent. One report can start a chain reaction. A recall. A warning. A life saved.
Pharmacists are the last line of defense. Don’t wait for someone else to speak up. If you see something, say something. The system depends on it.
Do pharmacists have to report generic drug problems by law?
No, federal law in the U.S. doesn’t require pharmacists to report generic drug problems. But the FDA strongly encourages it, and several states-including California, Illinois, Massachusetts, and New York-have made it mandatory for serious adverse events. Even where it’s not required, professional guidelines from ASHP and ISMP treat it as a core responsibility.
What’s the difference between a side effect and therapeutic inequivalence?
A side effect is an unwanted reaction that’s known and listed on the label-like dizziness or nausea. Therapeutic inequivalence means the drug isn’t working as it should, even if it’s not listed as a side effect. For example, a patient on generic levothyroxine who suddenly has high TSH levels after switching brands isn’t having a side effect-they’re having a failure of the drug to do its job. That’s therapeutic inequivalence.
Can I report if I don’t know the manufacturer or lot number?
Yes, you can still report. The FDA accepts reports without all details, but the more information you provide, the more likely your report will trigger action. If you don’t know the lot number, write "unknown" or check your pharmacy’s dispensing record. If you don’t know the manufacturer, look at the pill imprint or call your wholesaler. Even partial reports help identify trends.
Why do manufacturers report more than pharmacists?
Manufacturers are legally required to report adverse events they become aware of. Pharmacists aren’t. Also, manufacturers have dedicated safety teams and software to track reports. Pharmacists are often overworked and lack tools to document and submit reports easily. That’s why pharmacists, despite dispensing 90% of generics, only contribute about 2.3% of reports.
Will reporting get me in trouble with my pharmacy?
No. Reporting adverse events is a protected professional activity. The FDA keeps reports confidential and does not share them with employers. Your pharmacy’s liability is not increased by your report. In fact, many pharmacies are now building safety programs around reporting because it reduces risk long-term. If your pharmacy discourages reporting, it’s not protecting you-it’s ignoring a critical safety tool.
How long do I have to file a report?
For serious adverse events (life-threatening, hospitalization, death), the FDA recommends reporting within 15 calendar days of becoming aware of the event. For non-serious but unexpected events, report as soon as possible. There’s no penalty for late reporting, but delays can slow down safety investigations.
Is it worth reporting if I only see one patient with the issue?
Yes. Single reports can be the first sign of a larger problem. The FDA’s database has over 25 million reports. Many safety signals started with just one pharmacist noticing something odd. If you see a pattern-even with one patient-write it down. If you see the same issue again, report it. Your report could be the trigger that saves someone else.