For people with moderate to severe COPD who keep having flare-ups, the goal isn’t just to manage symptoms-it’s to stop those flare-ups before they start. One of the most powerful tools available today is triple inhaler therapy, which combines three medications in one device to tackle airway narrowing, inflammation, and mucus buildup all at once. But it’s not for everyone. Getting it right means understanding who benefits most, how the devices work, and what the real risks are.
What Is Triple Inhaler Therapy?
Triple inhaler therapy means using three types of COPD medications together: a long-acting muscarinic antagonist (LAMA), a long-acting beta-agonist (LABA), and an inhaled corticosteroid (ICS). Each plays a different role:- LAMA (like umeclidinium or glycopyrronium) relaxes the airway muscles by blocking a chemical that causes tightening.
- LABA (like vilanterol or formoterol) works alongside LAMA to open airways further by stimulating receptors in the lungs.
- ICS (like fluticasone or budesonide) reduces chronic inflammation in the airways, which is a key driver of flare-ups.
These three drugs were once taken in separate inhalers-sometimes three different devices. Now, they’re combined into one single-inhaler device, making it easier to stick with the treatment. The most common brands are Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol), Trimbow (budesonide/glycopyrronium/formoterol), and QBreva (beclomethasone/glycopyrronium/formoterol).
Who Actually Benefits?
Not every COPD patient needs triple therapy. In fact, most don’t. The 2024 GOLD guidelines say this treatment should be reserved for people who meet two clear criteria:- They’ve had two or more moderate flare-ups in the past year, or one severe flare-up that required hospitalization.
- They have blood eosinophil counts of 300 cells/µL or higher. This is a marker of allergic-type inflammation in the lungs.
When these two things line up, triple therapy can cut exacerbations by about 25% compared to dual bronchodilator therapy (LAMA/LABA). In the IMPACT trial, patients with eosinophils above 300 saw fewer hospital visits and fewer days spent sick. But if your eosinophil count is below 100, triple therapy offers no extra benefit-and may even raise your risk of pneumonia.
That’s why doctors now check your blood eosinophil level before prescribing this treatment. It’s not a guess. It’s a test. And if your count is low, you’re better off with just a LAMA/LABA combo.
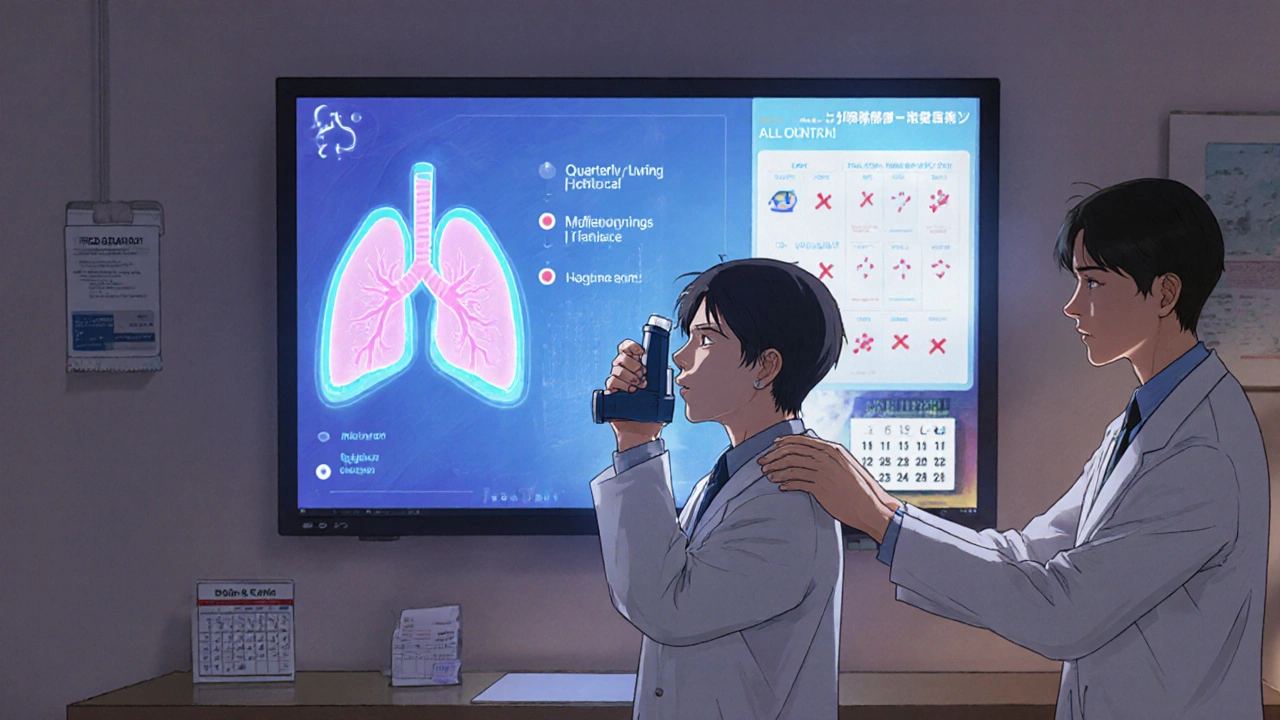
Single vs. Multiple Inhalers: Adherence Matters
Taking three separate inhalers is complicated. Many patients forget which one to use, when to use it, or simply get overwhelmed. Real-world data from the TARGET study shows that people using multiple-inhaler triple therapy (MITT) had only a 62% adherence rate after a year. That means nearly 4 out of 10 stopped taking one or more of their meds.Switching to a single-inhaler device (SITT) like Trelegy Ellipta or Trimbow boosts adherence to nearly 80%. Why? Because it’s one puff, once a day. No more juggling devices. No more confusion. A 2023 study found that 76% of patients who switched from multiple inhalers to a single device said their daily routine became much simpler-and their flare-ups dropped by 37% in the six months after the switch.
But it’s not just about convenience. Proper technique matters too. The Ellipta device requires a specific breathing pattern: inhale deeply and hold your breath. If you don’t, the medicine won’t reach deep into your lungs. Studies show it takes about 7 minutes of coaching to get it right. Many patients are never properly trained-and that’s why up to 70% of people who seem to “not respond” to treatment are actually just using their inhaler wrong.

The Pneumonia Risk You Can’t Ignore
Inhaled steroids reduce inflammation, but they also suppress the immune system in the lungs. That’s why pneumonia is the biggest safety concern with triple therapy. The risk is real:- Fluticasone-based triple therapy (like Trelegy) carries a 1.83 times higher risk of pneumonia than budesonide-based options (like Trimbow).
- Every year, about 1 in 10 patients on ICS-containing regimens gets pneumonia.
- The FDA requires a black box warning on all ICS inhalers for this exact reason.
That’s why doctors don’t just prescribe it and walk away. They monitor you. If you start coughing more, running a fever, or feeling unusually tired, you need to get checked. Some clinics now schedule quarterly visits to watch for early signs of lung infection. And if you’ve had pneumonia before, triple therapy might not be the right choice at all.
Cost and Access: The Hidden Barrier
These inhalers are expensive. In the U.S., a month’s supply of Trelegy Ellipta can cost $75 to $150 out-of-pocket. For Medicare beneficiaries on fixed incomes, that’s a lot. A 2022 study found that 22% of patients skipped doses because they couldn’t afford it. That’s not just a financial problem-it’s a health crisis. Skipping doses leads to more flare-ups, more ER visits, and more hospital stays.Some pharmacies offer savings cards or patient assistance programs. Others use medication synchronization to deliver all your COPD meds on the same day each month, making refills easier. But the cost barrier remains one of the biggest reasons triple therapy isn’t used more widely-even when it’s the right choice.
What Experts Really Think
There’s disagreement in the medical community-and it’s not just about the drugs. Some researchers, like Professor Jadwiga Wedzicha, argue the data clearly shows benefit for high-eosinophil patients. Others, like Dr. John Blakey, point out that many trials compared triple therapy to dual therapy where patients had their ICS abruptly stopped. That’s not fair. If you take away an anti-inflammatory drug suddenly, of course the patient will flare up. The real question is: does triple therapy do better than keeping the ICS and adding a second bronchodilator?The FDA and EMA both rejected claims that triple therapy reduces death rates. It doesn’t. But it does reduce hospitalizations. That matters. A hospital stay for a COPD flare-up costs tens of thousands of dollars and can lead to permanent lung damage. Preventing one flare-up can change a person’s life.
The consensus? Use it wisely. Don’t use it as a default. Don’t use it if your eosinophils are low. Don’t use it if you can’t afford it or can’t use the device properly. But if you’re a high-risk patient with clear inflammation markers, it’s one of the most effective tools we have.
What Comes Next?
The future of COPD treatment is getting smarter. Researchers are testing new biomarkers like fractional exhaled nitric oxide (FeNO) to see if it’s a better predictor of who will respond to steroids than eosinophils. Meanwhile, biologics like dupilumab-originally used for asthma and eczema-are showing promise in early trials for COPD patients with high eosinophils. These are injectable drugs that target specific inflammation pathways.By 2027, experts predict most advanced COPD patients will be guided by blood tests and breathing biomarkers, not just symptoms. Triple therapy won’t disappear-it will become more targeted. For now, it’s a powerful option for a specific group: those with frequent flare-ups and elevated eosinophils who can afford it, use it correctly, and are monitored for side effects.
Key Takeaways
- Triple inhaler therapy (LAMA/LABA/ICS) reduces COPD flare-ups by about 25% in patients with frequent exacerbations and blood eosinophil counts ≥300 cells/µL.
- Single-inhaler devices (like Trelegy Ellipta) improve adherence by 15-20% compared to multiple inhalers.
- Pneumonia risk is real-especially with fluticasone-based products. Budesonide-based options carry lower risk.
- Triple therapy offers no benefit-and may increase harm-for patients with eosinophil counts below 100 cells/µL.
- Cost is a major barrier: $75-$150/month out-of-pocket in the U.S. leads many to skip doses.
- Proper inhaler technique is critical. Up to 70% of apparent treatment failures are due to incorrect use.
- Doctors should check eosinophil levels before prescribing and monitor for pneumonia symptoms quarterly.
Is triple inhaler therapy right for everyone with COPD?
No. Triple therapy is only recommended for people with moderate-to-severe COPD who’ve had two or more flare-ups in the past year AND have blood eosinophil counts of 300 cells/µL or higher. If you don’t meet both criteria, it won’t help-and could raise your risk of pneumonia. Most COPD patients are better off with just a LAMA/LABA combination.
What’s the difference between Trelegy and Trimbow?
Trelegy Ellipta contains fluticasone furoate, umeclidinium, and vilanterol. It’s taken once daily. Trimbow has budesonide, glycopyrronium, and formoterol, and is taken twice daily. Trelegy has a higher pneumonia risk because of fluticasone. Trimbow’s budesonide is considered safer for the lungs. Trimbow also uses extrafine particles, which may reach deeper into the lungs. Cost and dosing frequency are also factors-once-daily is easier to stick with.
Can I switch from two inhalers to one triple inhaler?
Yes, and many patients benefit from the switch. If you’re on separate LAMA and LABA inhalers and your doctor thinks you’re a candidate for ICS, switching to a single-inhaler triple therapy can improve adherence and reduce flare-ups. But you should never stop your current meds without medical guidance. Your doctor will guide you through a safe transition, often with overlap to avoid sudden withdrawal.
Why do I need a blood test before starting triple therapy?
Your blood eosinophil count tells your doctor whether your COPD has an inflammatory component that responds to steroids. If your count is below 100, adding an inhaled steroid won’t help and increases your pneumonia risk. If it’s above 300, you’re likely to get a strong benefit. This test turns triple therapy from a guess into a targeted treatment.
What should I do if I miss a dose of my triple inhaler?
If you miss a dose, take it as soon as you remember-but don’t double up. For once-daily devices like Trelegy, skip the missed dose if it’s already close to your next scheduled time. For twice-daily devices like Trimbow, take the missed dose if it’s within a few hours. Consistency matters more than perfection. If you’re missing doses often, talk to your doctor about switching to a simpler regimen or getting help with adherence tools.
How do I know if my inhaler technique is correct?
Ask your doctor or pharmacist to watch you use your inhaler. Most devices have specific steps-for example, with Trelegy Ellipta, you must inhale deeply and hold your breath for 5 seconds. Many people think they’re doing it right, but studies show up to 70% use their inhalers incorrectly. Clinics often use checklists to verify technique. If you’re still having flare-ups despite taking your meds, poor technique is likely the culprit.
Next Steps If You’re Considering Triple Therapy
- Ask your doctor to check your blood eosinophil count if you’ve had frequent COPD flare-ups.
- If your count is ≥300 cells/µL and you’ve had two or more exacerbations in the past year, discuss whether triple therapy is right for you.
- Ask about device options: single-inhaler vs. multiple, once-daily vs. twice-daily, cost, and pneumonia risk.
- Request a hands-on training session with your pharmacist to master your inhaler technique.
- Set up quarterly follow-ups to monitor for pneumonia symptoms and lung function changes.
- Explore patient assistance programs if cost is a barrier-many manufacturers offer copay cards.
Triple inhaler therapy isn’t a miracle cure. But for the right person, it can mean the difference between staying out of the hospital and ending up there again and again. It’s not about using the most powerful drug-it’s about using the right drug, the right way, for the right person.


Comments (12)
Kyle Swatt
Man, this triple inhaler stuff is wild. I’ve seen guys on Trelegy go from gasping on the porch to walking their dog without stopping. But then I’ve also seen folks on it get pneumonia so bad they ended up on a ventilator. It’s not magic-it’s a scalpel. Use it right, and it saves lives. Use it wrong, and it’s just another expensive cough suppressant with a side of lung infection. The eosinophil test? That’s the gatekeeper. Skip it, and you’re gambling with your lungs.
Jessica Healey
i hate how doctors just throw this at you like its a cure all. my aunt got prescribed trelegy and now she’s got pneumonia twice in 8 months. they never even checked her eosinophils. she’s 72, on medicaid, and now she’s scared to even breathe too hard. this is profit-driven medicine disguised as science.
satya pradeep
From India, here. We don’t even have access to these fancy triple inhalers. Most patients here use one nebulizer and hope. The cost? In my city, a single inhaler costs more than a week’s salary for a laborer. We need affordable alternatives-not just fancy devices for rich countries. Also, technique training? Ha. Most clinics don’t even have a nurse who knows how to demonstrate it.
Elia DOnald Maluleke
While the science presented is commendable and meticulously structured, one must not overlook the socio-economic dissonance inherent in such therapeutic paradigms. In nations where access to clean air is a luxury, and where the very notion of a quarterly pulmonary follow-up is a distant dream, the privileging of biomarker-guided inhalation regimens becomes an exercise in epistemic colonialism. The eosinophil count, though statistically significant, is but a metric of the privileged.
Tarryne Rolle
So let me get this straight-we’re giving people steroids in their lungs to prevent flare-ups, but we’re ignoring the fact that air pollution, secondhand smoke, and poor housing are the real causes? This is like putting a bandage on a bullet wound and calling it medicine. We’re treating symptoms like they’re the disease. Meanwhile, the real culprits-corporate polluters, housing inequality, lack of public health infrastructure-are untouched. Triple inhalers? More like triple distractions.
Leslie Douglas-Churchwell
Did you know the FDA’s black box warning was almost buried? 🤫 Big Pharma knew ICS increases pneumonia risk but pushed the narrative that "benefits outweigh risks"-while quietly funding studies that downplayed the data. And now we’re told to trust "experts"? Lol. The same people who said vaping was safe. The same people who told us cigarettes were fine. 🧠👁️🗨️ This isn’t medicine-it’s a controlled experiment on the elderly.
Levi Hobbs
I really appreciate how thorough this breakdown is. The adherence stats-62% vs. 80%-are staggering. And the technique point? So true. I’ve seen patients who think they’re using their inhaler right, but they’re just exhaling into it. It’s heartbreaking. Maybe we need mandatory inhaler certification, like a driver’s license for your lungs? Also, kudos on mentioning Trimbow’s extrafine particles-most people don’t know that matters.
Joseph Peel
There’s a cultural blind spot here. In many households, especially among older adults, the idea of "one puff, once a day" sounds too simple to be effective. There’s a deep-seated belief that more pills = better medicine. That’s why even when single-inhaler therapy is prescribed, patients sometimes add back their old inhalers "just in case." Education has to go beyond the clinic-it needs to reach kitchens, living rooms, and family gatherings.
Prem Hungry
As a respiratory therapist in Mumbai, I can confirm: 80% of COPD patients don’t know how to use their inhalers. We train them with plastic demo devices, YouTube videos, and sometimes just hand gestures. The triple inhaler? We can’t even get them LAMA/LABA consistently. But if someone *does* get access, we push for Trimbow over Trelegy-budesonide is safer, cheaper, and works just as well. Also, cost is everything. A patient once asked me: "Can I use my asthma inhaler instead?"
Jeremy Hernandez
They’re selling this like it’s a miracle, but the real story? It’s a corporate cash grab. Triple inhalers cost 3x more than dual. Insurance pushes them because they’re branded. Doctors push them because reps give them free lunches. Patients? They’re stuck paying the bill. And if you’re poor? Too bad. Your lungs don’t matter as much as the bottom line. This isn’t medicine. It’s capitalism with a stethoscope.
henry mariono
I just want to say thank you for writing this without hype. I’ve been on Trimbow for a year. My eosinophils were 410. I used to go to the ER every other month. Now it’s been 11 months. I still use my inhaler wrong sometimes. My pharmacist caught it last month. We fixed it. It’s not perfect. But it’s working. And that’s enough.
Bill Machi
Let’s be honest. This whole triple therapy trend is a distraction from the real issue: America’s failure to regulate industrial pollution and tobacco sales. We spend billions on expensive inhalers while factories keep dumping toxins into the air. We treat the symptom, not the cause. And we wonder why COPD rates keep climbing. This isn’t innovation. It’s damage control for a broken system. If we cared about lungs, we’d clean the air-not just sell more puffs.