Managing bipolar disorder isn’t about finding one magic pill. It’s about balancing two powerful classes of medication-mood stabilizers and antipsychotics-to keep mood swings under control without wrecking your body in the process. For many people, this is a years-long trial-and-error journey, filled with side effects, blood tests, and tough choices. But it doesn’t have to be a guessing game. With the right approach, you can reduce episodes, protect your long-term health, and actually feel like yourself again.
Why These Medications Matter
Bipolar disorder isn’t just mood swings. It’s cycles of deep depression that can leave you unable to get out of bed, and manic episodes that push you into reckless spending, sleepless nights, or dangerous behavior. Without treatment, suicide risk is 15 to 20 times higher than in the general population. That’s why medications like lithium and quetiapine aren’t optional-they’re lifesaving. Lithium, approved by the FDA in 1970, remains the gold standard. Studies show it cuts suicide risk by 80% compared to placebo. Quetiapine, approved for bipolar depression in 2006, works faster-some people feel better in just 7 days. But neither works the same for everyone. And both come with serious trade-offs.Mood Stabilizers: The Foundation
There are four main mood stabilizers used today: lithium, valproate, carbamazepine, and lamotrigine. Each has its own profile. Lithium is the most studied. It’s effective for both mania and depression, and it’s the only one proven to reduce suicide risk long-term. But it’s finicky. You need regular blood tests to keep levels between 0.6 and 1.0 mmol/L. Too low? It won’t work. Too high? You risk toxicity-slurred speech, tremors, even seizures. Side effects are common: constant thirst, frequent urination, hand shakes, weight gain of 10-15 pounds in the first year. Many people quit because they feel like they’re constantly dehydrated. Lamotrigine is the go-to for depression in bipolar disorder. It has a 47% response rate compared to 28% for placebo. The big win? Almost no weight gain. But it comes with a scary risk: a serious skin rash in about 10% of people. That’s why doctors start with tiny doses and increase slowly over weeks. If you get a rash, stop immediately and call your doctor. Valproate works well for mania, especially in rapid-cycling cases. But it’s dangerous for women of childbearing age-it can cause severe birth defects. The FDA has a black box warning for this. It also affects the liver and pancreas, so blood monitoring is critical.Antipsychotics: Fast Action, Heavy Cost
Atypical antipsychotics like quetiapine, olanzapine, risperidone, and aripiprazole are now used just as often as mood stabilizers. They’re not just for psychosis. They’re frontline tools for acute mania and bipolar depression. Quetiapine (Seroquel) is one of the most prescribed. It’s effective for depression and helps with sleep. But 60-70% of users report drowsiness. Weight gain is brutal-on average, people gain 22 pounds in the first year. It also increases diabetes risk by 20-30% over time. Olanzapine (Zyprexa) is even more likely to cause weight gain and metabolic problems. One study showed a 4.6 kg (10 lbs) weight gain in just 6 weeks. That’s why many doctors avoid it unless other options fail. Aripiprazole (Abilify) is a better choice if weight gain is a concern. It’s less likely to cause metabolic issues, but it can cause restlessness-akathisia-which feels like you can’t sit still. Some people describe it as feeling like their nerves are on fire. Cariprazine and lumateperone are newer options approved in recent years. Lumateperone (Caplyta), approved in 2023, causes only 0.8 kg of weight gain in 6 weeks-far less than quetiapine’s 3.5 kg. It’s becoming a preferred first-line for depression.Combining Medications: More Power, More Risk
Many people need more than one medication. Combining a mood stabilizer with an antipsychotic boosts response rates to 70% in treatment-resistant cases. But it also increases side effects by 25-30%. For example: lithium + quetiapine might control both mania and depression well. But now you’re dealing with tremors, thirst, drowsiness, weight gain, and higher diabetes risk-all at once. That’s why doctors start low and go slow. They don’t just throw pills at the problem.
What About Antidepressants?
This is one of the most debated topics. Antidepressants like fluoxetine or sertraline can help with bipolar depression. But they carry a real risk: triggering mania. Studies show 10-15% of people switch into mania when taking them alone. That’s why they’re never used without a mood stabilizer. Some experts, like Dr. Gary Sachs at Harvard, say avoid them entirely. Others, like Dr. David Miklowitz at UCLA, say they’re okay if used carefully with a mood stabilizer. The bottom line: if you’re on an antidepressant, your doctor should be watching you closely for signs of mania-increased energy, less sleep, impulsivity.Monitoring: The Unseen Part of Treatment
Medication management isn’t just about taking pills. It’s about tracking your body. If you’re on lithium, you need blood tests every 2-3 months once stable. More often when starting. Your doctor checks your kidney and thyroid function, too. Lithium can damage both over time. If you’re on an antipsychotic, you need quarterly checks for weight, waist size, blood sugar, and cholesterol. The goal? Catch metabolic syndrome early. A waist over 40 inches for men or 35 for women is a red flag. Fasting glucose above 100 mg/dL means you’re heading toward diabetes. Many patients skip these tests. They feel fine. But damage builds silently. One man on olanzapine gained 50 pounds over two years and didn’t realize his blood sugar was rising until he had a pre-diabetes diagnosis.Real People, Real Struggles
Online communities like r/BipolarReddit and PatientsLikeMe are full of raw stories. One person wrote: “Lithium made me drink 3 liters of water a day and still feel dehydrated. I switched to lamotrigine-now I can’t sleep at all.” Another said: “After three meds failed, lithium finally worked. I gained 15 pounds, but I haven’t had a suicidal week in two years. Worth it.” A 2022 NAMI survey of 1,200 people found 45% quit their meds because of side effects. Top reasons? Weight gain (78%), brain fog (65%), and sexual problems (52%). But there’s hope. One Reddit user shared: “I started metformin for the weight gain from quetiapine. Lost 18 pounds in 6 months. Still tired, but I’m alive.”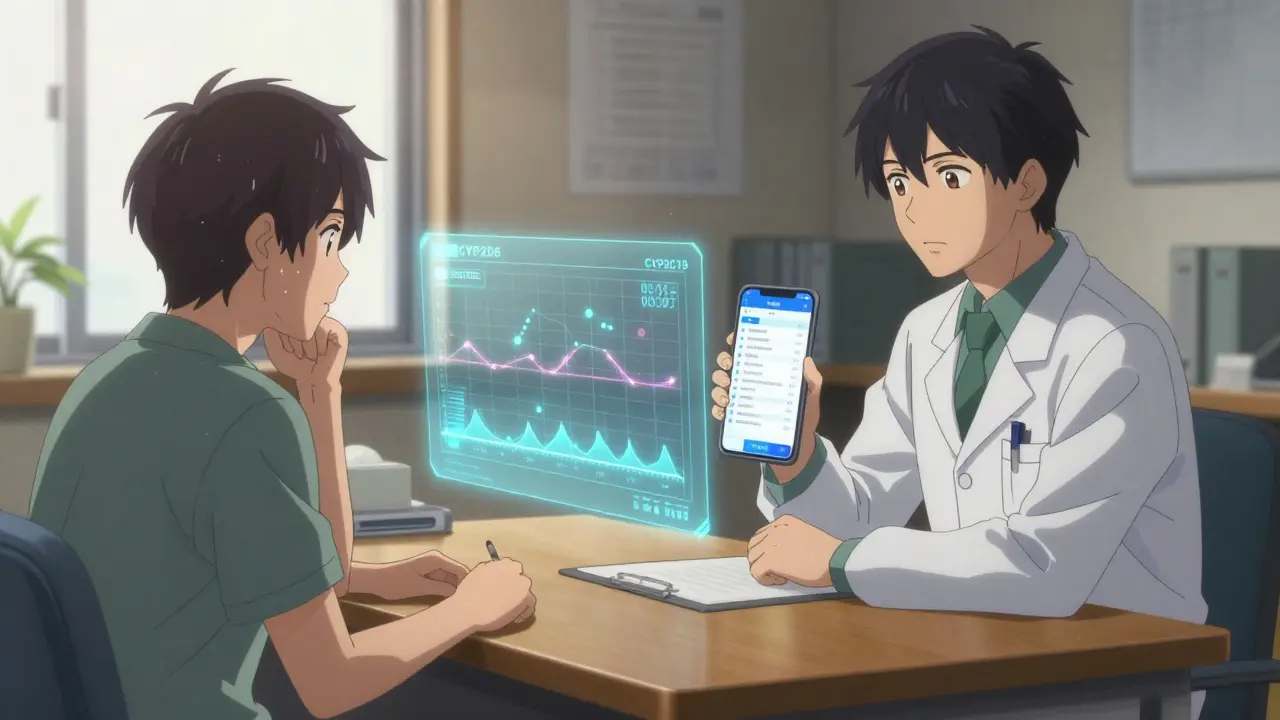
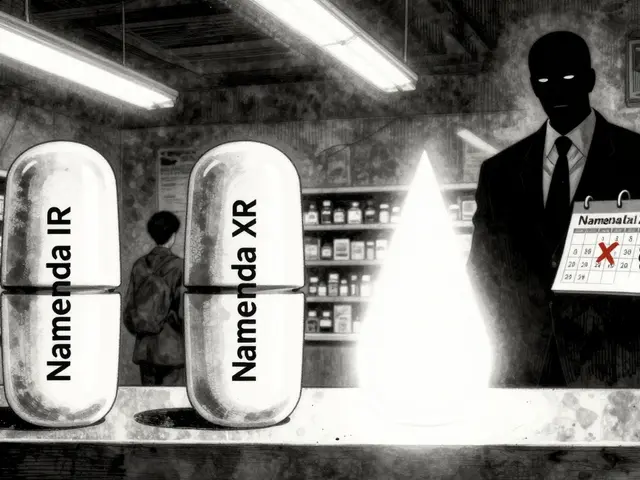
Cost, Access, and New Options
Lithium costs $4 to $40 a month. Brand-name antipsychotics like Vraylar can run $1,200. Most people take generics. New options are emerging. Long-acting injectables like Abilify Maintena mean you only need one shot a month-no daily pills. That helps with adherence. Genetic testing is becoming more common. Tests like Genomind look at your liver enzymes (CYP2D6, CYP2C19) to predict how you’ll process meds. One study showed 30% better results when doctors used this info. Digital tools like reSET-BD, a smartphone app approved by the FDA, help track moods and medication adherence. In trials, it cut relapse by 22%.What’s Next?
By 2027, experts predict personalized treatment will be standard. That means using your genetics, your side effect history, and your lifestyle to pick the right med-not just trial and error. New drugs targeting glutamate (like ketamine derivatives) are in trials. They could work in hours, not weeks. But they’re not ready yet. For now, the best approach is simple: find the lowest effective dose. Monitor your body. Don’t quit without talking to your doctor. And remember: it’s okay to switch. What works for someone else might not work for you. That’s not failure. That’s medicine.Practical Tips for Staying on Track
- Take lithium with food to reduce nausea.
- Split your daily dose into two-morning and evening-to reduce side effects.
- Use metformin if you’re gaining weight on antipsychotics-it’s safe and effective.
- Keep a mood journal. Note sleep, energy, and irritability daily.
- Never stop a mood stabilizer cold turkey. It can trigger a rapid switch into mania or depression.
- Ask your doctor about a 24-hour urine test if you’re on lithium and drinking a lot. It shows if your kidneys are struggling.
Medication isn’t the whole picture-but for most people with bipolar disorder, it’s the most important piece. Done right, it doesn’t just manage symptoms. It gives you back your life.
Can I stop my bipolar meds if I feel fine?
No. Stopping mood stabilizers or antipsychotics suddenly can trigger a severe mood episode-sometimes within days. Even if you feel stable, your brain still needs the medication to stay balanced. Always work with your doctor to taper off slowly, if at all. Most people need to stay on medication long-term to prevent relapse.
Which medication has the least weight gain?
Lamotrigine and aripiprazole cause the least weight gain among common bipolar medications. Lamotrigine often causes no weight change at all. Aripiprazole may lead to slight weight gain, but far less than quetiapine or olanzapine. Newer options like lumateperone and cariprazine also have minimal metabolic impact. If weight is a major concern, discuss these first-line options with your doctor.
How often do I need blood tests on lithium?
When you first start lithium, you’ll need blood tests weekly to find the right dose. Once your levels are stable, testing drops to every 2-3 months. If you’re over 65, your doctor may check more often-older adults process lithium slower. You’ll also get kidney and thyroid tests at least once a year. Skipping tests risks toxicity or organ damage.
Do antipsychotics make you feel numb or emotionless?
Some people report feeling emotionally flat or “numb” on antipsychotics, especially at higher doses. This isn’t the same as the emotional blunting of depression-it’s a side effect of dopamine blockade. Lowering the dose or switching to a different antipsychotic like aripiprazole (which works differently) often helps. If you feel disconnected from joy, grief, or anger, tell your doctor. This isn’t normal or unavoidable.
Is there a difference between generic and brand-name antipsychotics?
For most people, generic versions work just as well as brand-name drugs. Lithium, valproate, and quetiapine generics are widely used and effective. But with some medications, like extended-release forms or complex delivery systems, small differences in absorption can matter. If you switch from brand to generic and notice mood changes or new side effects, tell your doctor. Don’t assume it’s all in your head.
Can I drink alcohol while on bipolar meds?
It’s not recommended. Alcohol can worsen depression, increase sedation from antipsychotics, and interfere with lithium’s balance in your body. It can also trigger manic episodes in some people. Even one drink can throw off your mood stability. If you choose to drink, do so very rarely and in tiny amounts-and always talk to your doctor first.
What should I do if I miss a dose?
If you miss a dose of lithium or an antipsychotic, take it as soon as you remember-unless it’s close to your next dose. Never double up. Missing one dose usually won’t cause a crisis, but missing several can. Set phone reminders. Use a pill organizer. If you’re struggling with adherence, ask about long-acting injections or apps that track doses. Consistency matters more than perfection.


Comments (9)
Louis Paré
This post reads like a pharmaceutical sales pitch dressed up as medical advice. Everyone's got their favorite drug cocktail, but let's be real-most of these meds turn you into a zombie with a side of diabetes. And don't even get me started on the blood tests. I've spent more time in labs than at my own wedding. Who the hell designed this system? It's not treatment, it's endurance testing.
And yet, somehow, we're supposed to be grateful? No thanks. I'd rather ride the mood swings than be medicated into a coma.
Janette Martens
lithium made me so thirsty i started drinking outta the toilet i swear to god. and then my doc said 'maybe try lamotrigine' like its some kind of herbal tea. no. no no no. i need my meds to stop me from jumping off bridges. but god forbid i gain 20 lbs or my liver breaks. this system is broken. someone please fix it. or at least give us better snacks in the waiting room.
Manan Pandya
Thank you for this thorough breakdown. As someone who’s been on lithium for over a decade, I can confirm the thirst is real-but so is the stability. I’ve had two full manic episodes before starting it. Now, I’m able to hold a job, pay bills, and hug my daughter without fearing I’ll say something I can’t take back.
Yes, the side effects are brutal. Yes, the bloodwork is a pain. But this isn’t about convenience-it’s about survival. I wish more people understood that. You don’t quit because it’s hard. You adapt. You monitor. You advocate. And if one drug fails, you try another. That’s not weakness. That’s wisdom.
Aliza Efraimov
I just want to say-this post saved my life. Seriously. I was about to quit everything after gaining 30 pounds on quetiapine and feeling like a hollow shell. Then I read about metformin and tried it. Lost 18 lbs in 5 months. My therapist cried when she saw my progress. I’m not ‘cured’-but I’m alive. I can laugh again. I can cry without shame. I can sit in silence without wanting to scream.
To anyone reading this who feels hopeless: you’re not broken. You’re just on the wrong cocktail. Keep going. Find your person. Find your dose. Find your peace. You deserve to feel like yourself again. I’m proof it’s possible.
Nisha Marwaha
From a clinical pharmacology standpoint, the polypharmacological approach to bipolar disorder remains suboptimal due to the high interindividual variability in CYP450 enzyme expression, particularly CYP2D6 and CYP2C19 polymorphisms, which significantly alter drug clearance kinetics. Consequently, therapeutic drug monitoring (TDM) is not merely advisable-it is imperative.
Furthermore, the metabolic syndrome risk profile associated with second-generation antipsychotics necessitates a proactive, multidisciplinary intervention strategy incorporating endocrinology, nutrition, and behavioral medicine. The integration of digital phenotyping via FDA-cleared platforms such as reSET-BD represents a paradigm shift toward precision psychiatry. We are no longer in the era of empirical dosing-we are entering the age of algorithm-guided therapeutics.
Paige Shipe
Okay but why do we even have to take this crap? I mean, why can't we just... be normal? Like, I get it, brain chemistry, blah blah. But why is it always me? Why do I have to be the one with the blood tests and the weight gain and the doctor who talks like I'm a lab rat? I'm tired. I'm so tired. And now I'm reading about new drugs that cost $1,200? Like, what even is this? I work two jobs and still can't afford my meds. Someone please tell me this isn't real. It's not fair. It's not right. It's not right. It's not right. 😔😭💔
Tamar Dunlop
Allow me to express, with the utmost sincerity and profound respect for the gravity of this subject, that the narrative presented herein constitutes not merely a clinical overview, but a deeply human testament to resilience. The statistical data, while compelling, pales in comparison to the silent, daily battles waged by individuals navigating the treacherous terrain of neurochemical imbalance.
One must not underestimate the dignity inherent in continuing to rise each morning, despite the tremors, the thirst, the weight, the fear. This is not a medical condition. It is a crucible. And those who endure it, who persist, who seek alternatives, who advocate for themselves-these are the unsung heroes of our time.
Thank you for this document. It is not merely informative. It is sacred.
David Chase
THIS IS WHY AMERICA NEEDS MEDICARE FOR ALL!!! 😤💊📉
Who the F*** lets a person go broke just to stay alive?! I'm on Abilify and I pay $800/month because my insurance 'doesn't cover it properly'-but my landlord? He gets a discount on rent. My dog? He gets cheaper vet care than I do. I'm not a number. I'm not a statistic. I'm a person who needs to not kill herself.
Also-lamotrigine saved me. But I almost died from the rash. DOCTORS DON'T WARN YOU ENOUGH. I had to Google it myself. This system is a joke. And lithium? It's 1970s tech. We're in 2025. Fix it. Or I'm moving to Canada. 🇨🇦 #BipolarAndBroke #StopProfiteeringFromMentalIllness
Manan Pandya
Manan, I hear you. I’ve been on lithium too-11 years now. The thirst never leaves, but neither does the peace. What you said about adaptation? That’s the real treatment. Not the pill. The daily choice to show up, even when your body feels like it’s betraying you.
And to the person who said they almost quit after the rash-don’t. Lamotrigine is worth the slow climb. I started at 25mg. Took 10 months to get to 200mg. My skin held. My mood stabilized. I got my life back. It’s not glamorous. But it’s real.
And yes-metformin is a game-changer. I started it at 500mg at night. Lost 15 lbs. My A1C dropped. My doctor called it ‘a miracle.’ I called it ‘survival.’
You’re not alone. Keep going. One day at a time.