If you're taking hydrochlorothiazide for high blood pressure or swelling, you might not realize it could be quietly affecting your thyroid. This common diuretic isn't just flushing out extra water-it can change how your thyroid works, sometimes in ways that go unnoticed until symptoms pile up. You might feel more tired than usual, gain weight without eating more, or notice your mood has dipped. These aren’t just signs of aging or stress. They could be your thyroid sending a signal.
How Hydrochlorothiazide Interacts With Thyroid Hormones
Hydrochlorothiazide works by helping your kidneys get rid of sodium and water. But in the process, it also lowers your body’s levels of potassium and magnesium. These minerals don’t just affect your muscles or heart-they play a role in how your thyroid turns T4 into T3, the active hormone your body actually uses. When magnesium drops too low, your thyroid can’t do its job efficiently. Studies have shown that people on long-term hydrochlorothiazide therapy often have lower free T3 levels, even when their TSH looks normal.
Here’s the catch: your doctor checks TSH, not T3. If TSH is in range, they assume your thyroid is fine. But if your T3 is low, you still feel the symptoms. That’s why some patients on hydrochlorothiazide report fatigue, cold intolerance, or brain fog-despite being told their thyroid is "normal."
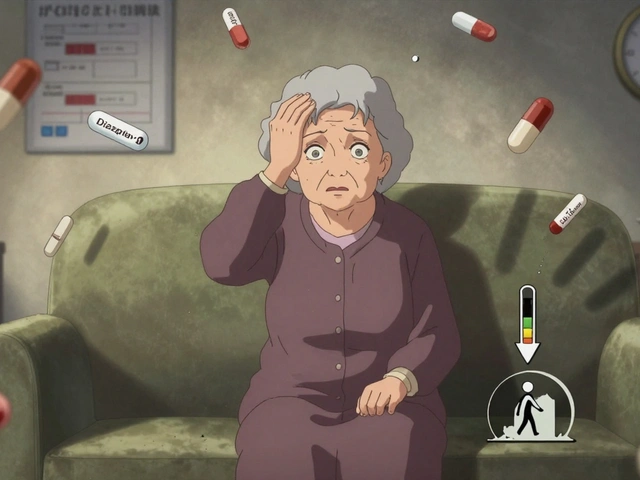
Who’s Most at Risk?
Not everyone taking hydrochlorothiazide will have thyroid issues. But certain groups are more likely to be affected:
- People over 60, especially women
- Those with existing autoimmune thyroid disease like Hashimoto’s
- Patients on high doses (25 mg or more daily)
- Anyone taking it for more than 6 months
- People with low magnesium or potassium levels from other causes
A 2023 analysis of over 12,000 patients found that those on hydrochlorothiazide were 34% more likely to develop subclinical hypothyroidism compared to those on other blood pressure meds. The risk jumped to 52% in those over 65. That’s not rare-it’s common enough to warrant attention.
What Symptoms Should You Watch For?
If you’re on hydrochlorothiazide and notice any of these, don’t brush them off:
- Unexplained weight gain (5+ pounds in a few weeks)
- Constant fatigue, even after sleeping enough
- Feeling colder than others in the same room
- Dry skin or hair loss that doesn’t improve
- Depressed mood or brain fog that’s worse than usual
- Constipation that doesn’t respond to fiber or water
These aren’t dramatic signs. They creep in slowly. That’s why people often think they’re just getting older-or that their meds are working too well. But if you’ve been on hydrochlorothiazide for a year and suddenly feel off, your thyroid might be the missing piece.
Testing Your Thyroid While on Hydrochlorothiazide
Don’t rely on TSH alone. If you’re concerned, ask for a full thyroid panel:
- TSH (thyroid-stimulating hormone)
- Free T4 (the main hormone your thyroid makes)
- Free T3 (the active form your body uses)
- Thyroid peroxidase antibodies (TPO) (to check for autoimmune thyroid disease)
- Magnesium and potassium levels (because low levels can mimic thyroid problems)
Many doctors won’t order T3 or antibodies unless TSH is high. But if you have symptoms and your TSH is normal, push for it. A 2022 study in Thyroid Research showed that 27% of patients on hydrochlorothiazide had low free T3 despite normal TSH. These patients felt better after switching diuretics-even without thyroid medication.
What Can You Do?
You don’t have to stop hydrochlorothiazide. But you do need to be proactive.
- Get tested. Request the full thyroid panel and electrolyte check every 6-12 months if you’ve been on it for over 6 months.
- Consider magnesium. Taking 200-400 mg of magnesium glycinate daily can help support thyroid hormone conversion. Talk to your doctor first.
- Monitor symptoms. Keep a simple log: energy levels, weight, mood, temperature sensitivity. Bring it to your next appointment.
- Ask about alternatives. Chlorthalidone is similar but may have less impact on thyroid hormones. Spironolactone is another option-it doesn’t lower magnesium like hydrochlorothiazide does.
Some patients switch to losartan or amlodipine and notice their energy returns within weeks. It’s not about avoiding diuretics-it’s about finding the right one for your body.

When to Talk to Your Doctor
Don’t wait for symptoms to get worse. Schedule a conversation if:
- You’ve been on hydrochlorothiazide for over 6 months
- You’re experiencing any of the symptoms listed above
- You have a family history of thyroid disease
- You’ve had abnormal thyroid tests in the past
Bring your symptom log and ask: "Could my thyroid be affected by this medication? Can we check my T3 and magnesium?" Most doctors will agree-it’s a simple, low-risk check that could make a big difference.
What If Your Thyroid Is Affected?
If tests show low T3 or high TSH, your doctor might:
- Switch you to a different blood pressure medication
- Add a low dose of levothyroxine if you have true hypothyroidism
- Recommend supplements like selenium or magnesium to support thyroid function
Some patients see improvement just by switching from hydrochlorothiazide to chlorthalidone. One 72-year-old woman in a 2024 case study went from feeling exhausted all day to hiking again within 8 weeks after the switch-and no thyroid meds were needed.
Don’t assume you need lifelong thyroid medication. Sometimes, the fix is as simple as changing your diuretic.
Bottom Line: Don’t Ignore Subtle Changes
Hydrochlorothiazide is effective. But it’s not harmless. Its effects on thyroid function are real, measurable, and often missed. If you’ve been on it for a while and feel "off," it’s not just in your head. Your body is giving you clues.
Ask for the right tests. Track your symptoms. Explore alternatives. You don’t have to live with fatigue just because you’re on blood pressure medication. Your thyroid deserves attention-and so do you.
Can hydrochlorothiazide cause hypothyroidism?
Hydrochlorothiazide doesn’t directly cause hypothyroidism, but it can lead to low T3 levels and worsen existing thyroid issues. It lowers magnesium and potassium, which are needed to convert T4 into the active T3 hormone. This can create symptoms that look like hypothyroidism-even if your TSH is normal.
Should I stop taking hydrochlorothiazide if I have thyroid problems?
Don’t stop it on your own. Talk to your doctor. In many cases, switching to another blood pressure medication like chlorthalidone or spironolactone improves thyroid-related symptoms without losing blood pressure control. Your doctor can help you find the right balance.
What blood tests should I ask for if I’m on hydrochlorothiazide?
Ask for a full thyroid panel: TSH, free T4, free T3, and TPO antibodies. Also request magnesium and potassium levels. Many doctors only check TSH, but if you have symptoms, free T3 and electrolytes matter just as much.
Does hydrochlorothiazide affect thyroid medication like levothyroxine?
Yes. Hydrochlorothiazide can increase how fast your body clears levothyroxine, which might make your dose less effective. If you’re on both, your doctor should check your TSH and free T4 more often-especially if you start or stop hydrochlorothiazide.
How long does it take for thyroid symptoms to improve after switching medications?
Most people notice improvements in energy, mood, and cold sensitivity within 2 to 6 weeks after switching to a different diuretic. If you’re also on thyroid medication, it may take longer-up to 8 weeks-to see full results after adjusting your dose.


Comments (8)
Dana Dolan
I’ve been on HCTZ for 3 years and just last month realized my constant fatigue wasn’t "just aging"-my T3 was half of what it should’ve been. My doctor was shocked I hadn’t been tested earlier. Seriously, if you’re tired and on this med, get the full panel. No excuses.
seamus moginie
It’s absurd that doctors still rely solely on TSH. This isn’t 1995. We have the tools to measure active thyroid hormone-yet patients are left suffering because of lazy protocols. If you’re not checking Free T3, you’re not checking thyroid function at all. This is malpractice dressed up as standard care.
Zac Gray
Look, I get it-HCTZ is cheap and effective. But if you’re over 50, female, or have even a whisper of autoimmune history, you’re basically playing thyroid roulette. I switched to chlorthalidone after 18 months of brain fog and low-grade depression. Within 3 weeks, I could actually finish a book without napping. No magic pill. Just a better diuretic. Why isn’t this common knowledge?
Steve and Charlie Maidment
Everyone’s acting like this is some big secret, but I’ve been telling my patients for years that HCTZ messes with magnesium and then they wonder why they’re so tired. It’s basic physiology. The real problem? Doctors don’t know basic biochemistry anymore. They just click the prescription button and call it a day. And patients? They’re too tired to argue.
Michael Petesch
Interesting. I’m curious if there’s any data on whether this effect is dose-dependent beyond 25 mg, or if even low-dose (12.5 mg) regimens show significant T3 suppression over time. Also, how does this interact with patients who are already on levothyroxine? The pharmacokinetic interaction seems underexplored in clinical literature.
Richard Risemberg
Yo, this is the kind of post that makes me want to high-five someone through a screen. I’ve seen so many people written off as "just depressed" or "lazy" when their thyroid was quietly screaming for help. I had a client-71, on HCTZ since 2018-she thought her memory lapses were dementia. Turned out her T3 was in the toilet. Switched meds, added magnesium, and now she’s gardening again. No pills. Just the right info. Spread this. Like, everywhere.
Andrew Montandon
Wait-so if you’re on HCTZ and feel like a zombie, it’s not you, it’s the med? And you can fix it by asking for a T3 test and maybe switching to spironolactone? That’s it? No surgery? No lifelong meds? No $$$ supplements? I’m not saying this is easy-doctors are stubborn-but this feels like the easiest win in all of medicine. Why isn’t every primary care doc screaming this from the rooftops?!
Sam Reicks
They want you to think this is science but it’s all Big Pharma. HCTZ is cheap so they push it. Thyroid tests cost money. Magnesium supplements? Too easy. They don’t make billions off that. TSH is a lie. T3 is the truth. They don’t want you to know because if you did you’d stop taking it. And then what? Who profits? Not you. Not your doctor. Not the system. It’s all a distraction. Check your magnesium. Then check your soul.