
Every year, over 80% of adults in the U.S. reach for an over-the-counter (OTC) medication before calling a doctor. It’s quick, easy, and feels harmless-until it isn’t. You might think popping a few pills for a headache or runny nose is no big deal, but the truth is, OTC medications can cause serious harm if used incorrectly. They’re not candy. They’re not harmless. They’re drugs-powerful ones-and knowing how to use them safely could save your life.
What Exactly Are OTC Medications?
OTC medications are drugs you can buy without a prescription. They’re approved by the FDA and similar agencies worldwide for treating minor, self-diagnosable conditions like headaches, allergies, heartburn, coughs, and colds. But don’t be fooled by the label. Just because you don’t need a doctor’s note doesn’t mean these drugs are safe for everyone, all the time.
There are more than 100,000 OTC products on the market in the U.S. alone, containing around 800 different active ingredients. These are grouped into clear categories: pain relievers, cold and flu remedies, allergy meds, stomach treatments, and topical products like antiseptic creams. Each one has a specific purpose, a specific dose, and specific risks.
Pain Relievers: Acetaminophen vs. Ibuprofen
If you’ve ever had a headache or sore muscles, you’ve probably reached for either acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). But they work very differently-and so do their risks.
Acetaminophen is great for reducing fever and easing pain. It’s often the go-to for kids, pregnant people, and those with stomach issues because it doesn’t irritate the gut like NSAIDs. But here’s the catch: it’s hard on your liver. Taking more than 4,000 mg in a day-even spread out over several doses-can cause severe liver damage. In fact, acetaminophen is the leading cause of acute liver failure in the U.S., with 15,000 to 18,000 emergency visits each year from overdoses. Many people don’t realize that acetaminophen is hidden in dozens of cold and flu products. Taking Tylenol for a headache and then a NyQuil for a cough? That’s a recipe for disaster.
Ibuprofen, on the other hand, is an NSAID. It reduces inflammation, which makes it better for sprains, arthritis, or menstrual cramps. But it can cause stomach bleeding, especially if taken on an empty stomach or for long periods. People with kidney problems, high blood pressure, or a history of ulcers should avoid it. The maximum daily dose is 1,200 mg for OTC versions. More than that? You’re stepping into prescription territory-and risk.
Bottom line: Use acetaminophen if you’re worried about your stomach or are pregnant. Use ibuprofen if you need to reduce swelling. Never take both together unless your doctor says so.
Cold and Flu: What Actually Works?
There are dozens of cold and flu meds on the shelf. But most don’t cure anything-they just mask symptoms. And some do more harm than good.
Pseudoephedrine (Sudafed) is one of the few effective decongestants. It shrinks swollen nasal passages. But it’s kept behind the counter because it can be used to make illegal drugs. You need to show ID and buy limited quantities. It can raise blood pressure and cause insomnia, so skip it if you have heart problems.
Dextromethorphan (Delsym, Robitussin) is a cough suppressant. It works for dry, hacking coughs. But it’s also abused by teens. Taking more than the recommended dose (usually 30 mg) can cause hallucinations, dizziness, and even coma. The FDA has warned about this for years, yet it’s still one of the most common OTC drug overdoses in adolescents.
Guaifenesin (Mucinex) is an expectorant. It helps thin mucus so you can cough it up. It’s generally safe, but it won’t make your cold go away faster. Drink plenty of water with it-it works better that way.
And skip multi-symptom formulas unless you have all the symptoms they claim to treat. Taking a product with antihistamines, decongestants, and pain relievers when you only have a sore throat? You’re overdosing on unnecessary chemicals.
Allergy Medications: The Drowsy vs. Non-Drowsy Divide
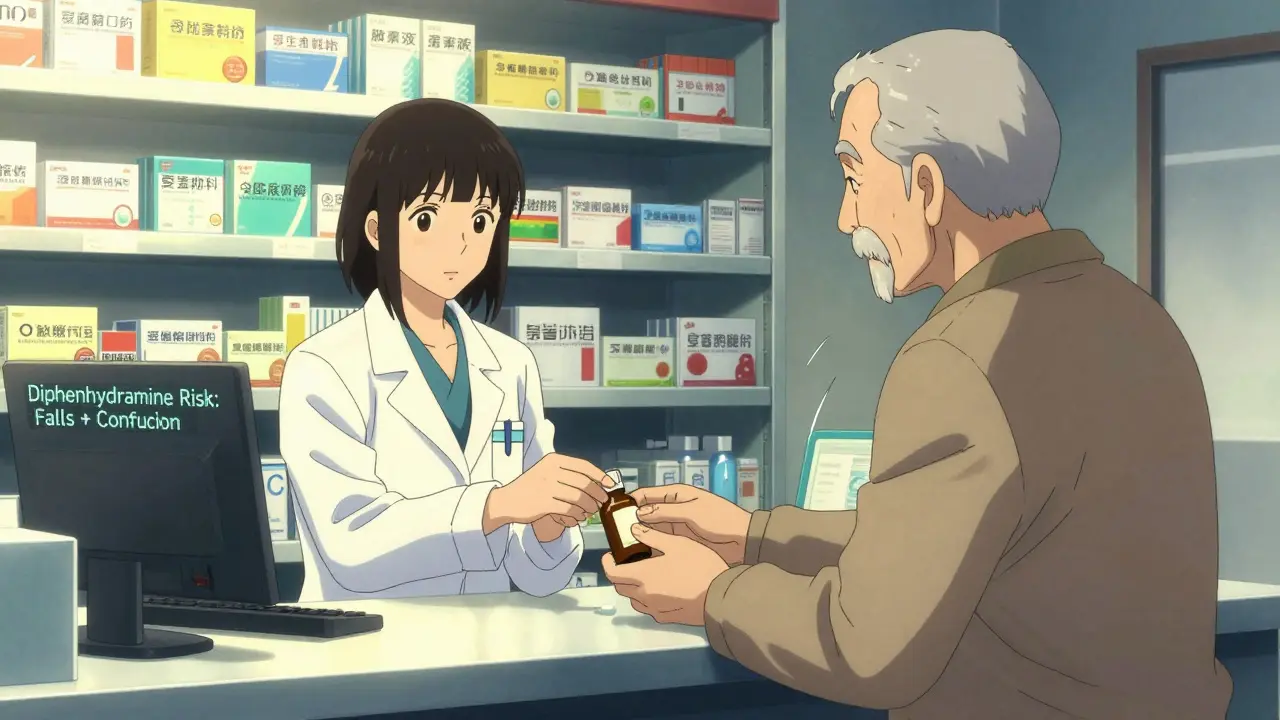
Allergy meds are where people make the biggest mistakes. First-generation antihistamines like diphenhydramine (Benadryl) work fast and cheap. But they make you sleepy-so much so that they’re often used as sleep aids. That’s dangerous. For adults over 65, diphenhydramine increases fall risk by 30%. It can also cause confusion, dry mouth, and urinary retention. The American Geriatrics Society lists it as a medication seniors should avoid.
Second-generation options like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) are far safer. They work just as well for sneezing and itchy eyes but cause little to no drowsiness. Loratadine is dosed at 10 mg once daily. Fexofenadine is 180 mg. Both are fine for long-term use in most people. If you’re on kidney medication, though, talk to your pharmacist. Fexofenadine may need a lower dose if your kidneys aren’t working well.
And don’t forget nasal sprays. Fluticasone (Flonase) is a steroid spray that reduces nasal inflammation. It takes a few days to work, but it’s more effective than oral antihistamines for congestion. It’s safe for daily use and doesn’t cause drowsiness.
Stomach Issues: Heartburn, Diarrhea, and Antacids
Heartburn is common. But treating it the wrong way can lead to bigger problems.
Antacids like Tums (calcium carbonate) give quick relief by neutralizing acid. Fine for occasional use. But if you’re taking them daily, you might be masking something serious like GERD.
H2 blockers like famotidine (Pepcid AC) reduce acid production. They last longer than antacids but aren’t as strong as the next level.
Proton pump inhibitors (PPIs) like omeprazole (Prilosec OTC) are the strongest. They block acid at the source. Great for frequent heartburn. But using them for more than 14 days in a row, or more than three times a year, can increase your risk of kidney disease, bone fractures, and vitamin B12 deficiency. A 2023 study in JAMA Internal Medicine found PPI users had a 20-50% higher risk of chronic kidney disease over time.
For diarrhea, loperamide (Imodium) slows bowel movements. It’s safe for short-term use. But if you have a fever, bloody stool, or it lasts more than two days, stop taking it and see a doctor. It can hide serious infections like C. diff.
Safety Rules You Can’t Ignore
Here’s what you need to remember every time you pick up an OTC medicine:
- Read the Drug Facts label. It’s not just filler. It tells you the active ingredient, purpose, uses, warnings, and directions. If you don’t know what’s in it, don’t take it.
- Check for duplicates. Many cold, flu, and pain products contain the same active ingredient. Taking two at once = overdose.
- Know your limits. Acetaminophen max = 4,000 mg/day. Ibuprofen max = 1,200 mg/day. Naproxen max = 660 mg/day. Don’t guess. Measure.
- Don’t use for chronic conditions. OTC meds aren’t meant for daily, long-term use. If you need pain relief every day for a month, see a doctor. You’re treating a symptom, not the cause.
- Watch for interactions. OTC meds can interfere with prescription drugs. For example, ibuprofen can reduce the effect of blood pressure meds. Antihistamines can worsen glaucoma or prostate problems.
- Store properly. Keep meds in a cool, dry place. Heat and moisture ruin them. Don’t leave them in the bathroom or car.
- Check expiration dates. Expired meds don’t work as well-and some can break down into harmful substances.
Special Populations: Kids, Seniors, and Pregnant People
Not everyone can take the same OTC meds.
Children under 4: The FDA bans cough and cold meds for this age group. They don’t work and have caused deaths. Use saline drops and a bulb syringe for congestion. Acetaminophen or ibuprofen (in child-appropriate doses) are fine for fever or pain.
Pregnant people: Acetaminophen is the only recommended pain reliever. Avoid NSAIDs after 20 weeks-they can affect fetal kidney development. Antihistamines like loratadine are considered safe. Avoid decongestants like pseudoephedrine in the first trimester.
Seniors over 65: Avoid diphenhydramine for sleep. It increases confusion and fall risk. Use melatonin or behavioral changes instead. NSAIDs can cause kidney damage and stomach bleeding in older adults. Always check with a pharmacist before taking anything new.
When to Call a Doctor
OTC meds are great for short-term relief. But they’re not a substitute for medical care. See a doctor if:
- Your symptoms last more than 7-10 days without improvement
- You have a fever over 102°F that doesn’t break
- You’re vomiting blood, passing black stools, or have severe abdominal pain
- You develop a rash, swelling, or trouble breathing after taking a med
- You’re taking more than the recommended dose for more than a few days
Many people delay seeing a doctor because they think OTC meds should fix everything. But if your body isn’t responding, it’s not because you need a stronger pill-it’s because you need a diagnosis.
The Role of Pharmacists
Pharmacists are your best resource for OTC safety. They’re trained to spot dangerous combinations, check for allergies, and recommend the right product for your situation. Nearly 93% of Americans live within five miles of a pharmacy. Use that resource. Don’t just grab the cheapest option off the shelf. Ask: "Is this safe for me?"
Many pharmacies now offer free OTC consultations. Some even use apps to scan your prescriptions and warn you about interactions. Take advantage of it.
What’s Changing in 2025?
Regulations are tightening. The FDA now requires clearer Drug Facts labels with bigger fonts and standardized wording. Some states are expanding pharmacists’ authority to prescribe certain OTC meds for minor conditions-like urinary tract infections or eczema-without a doctor’s visit.
Technology is also stepping in. CVS Health launched an AI tool called "OTC Advisor" that asks you about your symptoms, current meds, and health conditions, then recommends safe options. It’s not perfect, but it’s a step toward smarter self-care.
Still, the biggest problem remains: people think OTC means "safe." It doesn’t. It means "available." And availability doesn’t equal safety.
Use OTC meds wisely. Know what’s in them. Know your limits. When in doubt, ask a pharmacist. Your body will thank you.
Can I take acetaminophen and ibuprofen together?
Yes, but only if you stick to the recommended doses for each. Taking them together can give better pain relief than either alone. But don’t exceed 4,000 mg of acetaminophen per day or 1,200 mg of ibuprofen. Avoid this combo if you have liver or kidney disease. Always space doses at least 4-6 hours apart.
Is it safe to use OTC cold medicine for more than a week?
No. Most OTC cold meds are designed for short-term use-usually 5-7 days. Using them longer can mask serious conditions like sinus infections, bronchitis, or even pneumonia. Decongestants can raise blood pressure with prolonged use. Antihistamines can cause drowsiness, dry mouth, and urinary retention. If symptoms last beyond a week, see a doctor.
Why are some OTC meds kept behind the counter?
Some ingredients, like pseudoephedrine, can be used to make illegal drugs like methamphetamine. To prevent this, federal law requires these products to be stored behind the counter. You need to show ID and sign a log. You’re also limited to buying a small amount per day. This doesn’t mean they’re unsafe-it means they’re regulated to prevent misuse.
Can OTC meds affect my ability to drive?
Yes. First-generation antihistamines like diphenhydramine cause drowsiness and slow reaction times. Even second-generation ones can affect some people. The FAA prohibits pilots from flying within 12 hours of taking diphenhydramine. For drivers, if you feel sleepy, dizzy, or less alert after taking a med, don’t drive. Always check the label for warnings like "may cause drowsiness."
Are OTC medications safe during pregnancy?
Some are, some aren’t. Acetaminophen is considered safe for pain and fever throughout pregnancy. Avoid NSAIDs like ibuprofen after 20 weeks-they can harm fetal kidneys. For allergies, loratadine and cetirizine are preferred. Avoid decongestants like pseudoephedrine in the first trimester. Always check with your OB-GYN before taking any OTC med, even if it’s "safe for most people."
What should I do if I accidentally take too much of an OTC med?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. Acetaminophen overdose can cause liver damage without immediate signs. If you took more than the maximum daily dose-even by a little-get help. Time matters. Keep the medication bottle with you when you call.
Do OTC meds expire, and is it dangerous to use them after?
Yes, they expire. Most OTC meds are good for 2-3 years from manufacture. After that, they lose potency. While most expired meds aren’t toxic, some-like liquid antibiotics or nitroglycerin-can break down into harmful substances. Don’t use expired meds for serious conditions. For minor issues, it’s better to replace them. Store them properly to extend shelf life.
Why do some OTC meds have sugar in them?
Many liquid syrups and chewable tablets use sugar for flavor and texture. This can be a problem for people with diabetes. Always check the ingredient list for "sucrose," "sorbitol," or "high fructose corn syrup." Sugar-free versions exist for most common meds. Ask your pharmacist for them if you have diabetes or are watching your sugar intake.




Comments (14)
Ryan Cheng
Man, I used to pop Tylenol like candy until I learned it was hiding in every cold medicine under the sun. Now I always check the label. One time I took NyQuil and Advil together and woke up feeling like my liver was judging me. Never again.
wendy parrales fong
It's wild how we treat pills like snacks. We forget they're chemicals that change how our bodies work. Maybe if we thought of them like vitamins we'd be more careful. Not magic, just medicine.
Jeanette Jeffrey
Wow. Another preachy article about how dumb people are. Congrats, you just told everyone what they already know. The real issue? Pharma companies make billions off this ignorance. And you're just here to pat yourself on the back for reading the label. 🙄
Shreyash Gupta
bro i took 3 advil for my back and then a cold med with acetaminophen... i was fine 😎 but my friend took 5 tylenol and cried in the bathroom... so maybe just chill? 🤷♂️
Ellie Stretshberry
i always forget to check the ingredients and then wonder why i feel weird after taking something... i think i need to start writing stuff down or something... maybe a note on my phone? 🤔
Zina Constantin
As someone who grew up in a household where medicine was never discussed, this article feels like a lifeline. My mom used to give me aspirin for headaches and call it a day. I wish I'd known this stuff sooner. Thank you for writing this.
Dan Alatepe
yo i once took a whole bottle of melatonin 'cause i thought it was candy... turned out it was just a bad nap. But my cousin? He took dextromethorphan 'cause his friend said it was 'trippy'. He ended up in the ER. Bro. Read the label. 🙏
Angela Spagnolo
I... I didn't realize that... I mean, I knew, but... I guess I just... forgot? I've been taking ibuprofen every day for my knees... I think I need to call my pharmacist... maybe... tomorrow?
Sarah Holmes
This is exactly the kind of condescending, oversimplified, fear-mongering drivel that makes people distrust medicine. You treat patients like children who can't be trusted with information. The real problem is not OTC meds-it's the medical industrial complex that profits from your paranoia.
Jay Ara
good post man i always just grab what looks good but now i check the label like you said... its crazy how many things have acetaminophen in em
Michael Bond
Don’t take more than you need.
Kuldipsinh Rathod
My grandma used to say, 'If it's on the shelf, it's not a cure.' She never took anything unless she had to. Wish more people thought like that.
SHAKTI BHARDWAJ
OMG I JUST REALIZED I'VE BEEN TAKING FLONASE FOR 3 YEARS AND I DIDN'T EVEN KNOW IT WAS A STEROID?? I'M GONNA DIE?? I'M GONNA DIE??
Bryan Woods
While I appreciate the intent of this article, I think the tone risks alienating the very people it aims to help. Many of us aren't reckless-we're overwhelmed. A system that makes safe information hard to access, then blames individuals for not reading labels, is broken. Pharmacists should be the first line of defense, not an afterthought.