Proton pump inhibitors, or PPIs, are among the most common medications prescribed for heartburn, acid reflux, and ulcers. You’ve probably seen ads for Prilosec, Nexium, or Prevacid - they’re everywhere. And for good reason: they work. Fast. Effective. But here’s the part no one talks about loud enough - many people stay on them way longer than they should. And that’s where things start to get risky.
How PPIs Work - And Why They’re So Popular
PPIs don’t just mask symptoms. They shut down acid production at the source. They block the proton pumps in your stomach lining - the very cells that make stomach acid. This makes them the most powerful acid-reducing drugs available. For someone with severe esophagitis or a bleeding ulcer, they’re life-saving. But for someone with occasional heartburn? Often, they’re overkill.
Common PPIs include omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), and pantoprazole (Protonix). Prescription versions come in doses from 10mg to 40mg. Over-the-counter ones? Usually capped at 20mg. And the FDA says: don’t use OTC PPIs for more than 14 days in a row, and not more than once every three months. Yet, studies show nearly a quarter of people using them OTC keep going beyond that - sometimes for years.
The Hidden Costs of Long-Term Use
It’s not just about acid anymore. The longer you take PPIs, the more your body’s natural balance starts to shift. Here’s what the evidence actually shows:
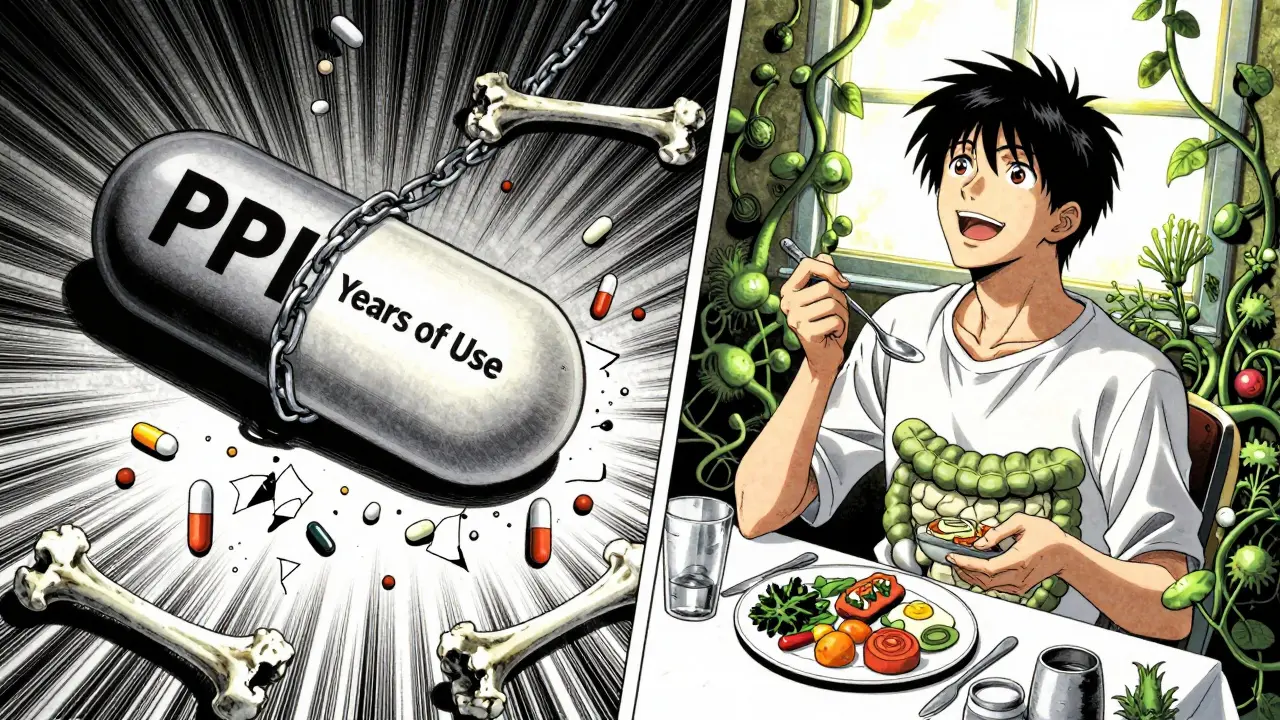
- Bone fractures: Long-term use - especially over four years - increases hip fracture risk by up to 55%. This isn’t a small risk. It’s real. And the good news? It reverses. People who stopped PPIs more than two years ago had fracture risk back to normal levels.
- Magnesium deficiency: Your body needs magnesium to keep muscles and nerves working right. PPIs interfere with absorption. Symptoms? Muscle cramps, fatigue, irregular heartbeat. The FDA now requires doctors to check magnesium levels in anyone on PPIs for over a year.
- Vitamin B12 deficiency: Acid helps break down food to release B12. Less acid? Less absorption. About 10-15% of long-term users develop low B12, which can lead to nerve damage and anemia if left unchecked.
- C. difficile infection: Stomach acid kills harmful bacteria. When you suppress it, you make it easier for C. diff to take over. Risk goes up 1.7 to 2 times. This is especially dangerous in hospitals or nursing homes.
- Rebound acid hypersecretion: This one catches people off guard. When you stop PPIs suddenly after months or years, your stomach goes into overdrive. Acid production spikes - worse than before. That’s why so many people think they “need” the drug. It’s not the disease coming back. It’s your body reacting to the sudden absence of the drug.
Some studies have linked PPIs to dementia, kidney disease, or heart problems. But here’s the catch: those studies often didn’t isolate PPIs as the cause. People on long-term PPIs are often older, sicker, or taking other meds. It’s hard to say if the PPI caused the problem - or if the underlying illness did.
When Should You Stop? The Real Guidelines
Not everyone needs to quit. But if you’re taking PPIs daily and don’t have a confirmed diagnosis like Barrett’s esophagus, active ulcer, or severe esophagitis - you should reconsider.
The American College of Gastroenterology says: Use the lowest dose for the shortest time possible. That means:
- If you were prescribed PPIs for 4-8 weeks to heal reflux damage - you should try to stop after that.
- If you’re on it for “just in case” heartburn - you’re probably not in the right group.
- If you’re using OTC PPIs for more than 14 days at a time - you need to talk to a doctor.
Here’s a simple rule: If you’ve been on PPIs daily for more than 3 months, ask your doctor if you still need it.
How to Stop Safely - No Rebound, No Panic
Stopping cold turkey? Bad idea. You’ll likely get worse heartburn than before - for weeks. Instead, follow this plan:
- Reduce your dose by half. If you’re taking 20mg daily, go to 10mg.
- Wait 1-2 weeks. If symptoms are mild, stay there.
- Switch to on-demand use. Only take it when you feel symptoms - not daily.
- Try H2 blockers like famotidine (Pepcid) or ranitidine (if available) for breakthrough symptoms. They’re less potent but don’t cause rebound.
- After a few weeks, try going completely off. Use antacids like Tums or Rolaids for occasional relief.
Some people need help. If you’ve been on PPIs for over a year, your doctor might suggest a gradual taper over 2-3 months. And yes - it’s okay to feel some discomfort. It doesn’t mean you’re getting sicker. It means your stomach is readjusting.
What Else Can You Do?
PPIs aren’t the only answer. Lifestyle changes work - and they’re safer long-term:
- Don’t eat 3 hours before bed.
- Avoid spicy foods, caffeine, alcohol, and chocolate - common triggers.
- Elevate the head of your bed by 6 inches.
- Lose weight if you’re carrying extra pounds around the middle.
- Stop smoking. It relaxes the lower esophageal sphincter - the valve that keeps acid down.
For many, these changes cut symptoms in half - or eliminate them entirely. And they don’t come with a risk list.
The Bigger Picture
Over 15 million Americans take prescription PPIs. Another 7 million use OTC versions regularly. That’s tens of billions of dollars spent every year. And research suggests up to 70% of those prescriptions aren’t truly necessary.
Why does this happen? Doctors sometimes prescribe them out of habit. Patients feel better and assume they need to keep going. Pharmacies sell them like candy. But here’s the truth: medication isn’t always the answer - especially when the side effects are hidden and slow to show up.
It’s not about fear. It’s about awareness. PPIs are powerful tools - but like any tool, they’re meant for specific jobs. You wouldn’t use a chainsaw to trim your hedges. Don’t use a PPI for a one-time heartburn flare-up.
Can I stop PPIs cold turkey?
No. Stopping suddenly after long-term use can cause severe rebound acid reflux. Symptoms may last weeks and feel worse than before. Always taper under medical supervision - reduce the dose gradually, then switch to on-demand use before quitting entirely.
How long is too long to be on PPIs?
For most conditions like GERD or ulcers, 4-8 weeks is enough. If you still need daily PPIs after that, your doctor should reassess. Long-term use (over 1 year) increases risks like fractures, low magnesium, and B12 deficiency. Regular check-ups are essential.
Are OTC PPIs safer than prescription ones?
No. OTC and prescription PPIs have the same active ingredients and risks. The FDA limits OTC use to 14 days because long-term self-medication is dangerous. Using them beyond that without a doctor’s advice increases your risk of side effects.
Do PPIs cause kidney damage?
There’s a link to acute interstitial nephritis - a rare but serious kidney inflammation - especially in the first few months of use. Chronic kidney disease is less clear. Some studies suggest a small increased risk, but it’s likely tied to other health problems. Still, if you’re on PPIs long-term, your doctor should monitor kidney function.
What are alternatives to PPIs?
For occasional heartburn, antacids (Tums, Rolaids) or H2 blockers (Pepcid, Zantac) are safer short-term options. Lifestyle changes - like eating earlier, avoiding triggers, losing weight, and elevating your head while sleeping - can be very effective. For chronic conditions, your doctor may recommend endoscopy or newer drugs like vonoprazan, though long-term safety data are still limited.
Final Thought
PPIs are not evil. They’re essential for people who truly need them. But they’re not harmless, either. The biggest danger isn’t the drug - it’s the assumption that because it works, you should keep taking it forever. If you’ve been on PPIs for more than a few months without a clear reason, talk to your doctor. You might be surprised how much better you feel without it.