
When your prescription switches from the brand-name drug you’ve been taking to a cheaper version, it’s normal to feel uneasy. What if it doesn’t work the same? What if something goes wrong? You’re not alone. But if the new version is an authorized generic, you’re getting the exact same medicine - same active ingredients, same factory, same pill - just without the brand name on the box.
What Exactly Is an Authorized Generic?
An authorized generic isn’t just another generic. It’s the brand-name drug made by the same company, sold under a different label. Think of it like a car manufacturer selling the same model under a private label at a discount store. The engine, the seats, the paint - everything’s identical. The only difference? The logo’s gone. The FDA requires these to be listed in the Orange Book, and they’re approved under the original brand’s New Drug Application (NDA). That means no extra testing for bioequivalence. No guesswork. It’s the same drug, same batch, same everything. That’s why pharmacists say patients rarely notice any change - because there isn’t one.Why Switch? The Real Cost Difference
Brand-name drugs can cost $200, $300, even $500 a month. Authorized generics? Often under $30. Some patients save $15 to $30 per prescription just by switching. That’s not a small amount when you’re paying out of pocket or have a high deductible. Medicare Part D data from 2022 shows that when an authorized generic is available, 80-90% of prescriptions are automatically filled with it. Insurance plans push for it because it saves them money - and they pass some of those savings to you. In some cases, the price drop is immediate: 8.4% to 18.2% lower than the brand, even before other generics hit the market. And here’s the kicker: authorized generics often launch during the 180-day exclusivity window when only one generic is allowed. That’s when prices drop the most. The FTC found retail prices fell 4-8% and wholesale prices dropped 7-14% when authorized generics entered the market during that time.How to Confirm You’re Getting the Real Thing
Not every generic is an authorized generic. Many are made by different companies, in different factories, with different fillers. That’s fine - they’re still safe. But if you want the exact same pill you’ve always taken, you need to check. Go to the FDA’s website and search their quarterly list of authorized generics. Type in your drug’s name - say, “Lisinopril” - and see if any authorized versions are listed. If you see the brand name (like “Zestril”) listed alongside a generic version made by the same company, you’ve found it. Pharmacists can help too. Ask: “Is this an authorized generic?” They’ll know. Some even have alerts in their systems now that flag when an authorized version is available. Don’t assume. Verify.What If the Pill Looks Different?
This is the #1 question patients ask. “The pill is a different color. It’s smaller. The imprint changed. Is this still the same?” Yes. It’s still the same. Authorized generics are made by the brand company, so sometimes they look exactly like the original - same shape, same color, same markings. But sometimes, the packaging changes. Maybe the brand used a blue pill with “ABC123” on it. The authorized generic might be white with “AG123.” That’s because the brand company doesn’t want to confuse customers with identical packaging. The FDA says appearance doesn’t affect how the drug works. The active ingredient, dosage, and release profile are unchanged. Still, if you’re used to a certain look, it can trigger anxiety. That’s normal. Talk to your pharmacist. They can show you the FDA list and explain why the change happened.
Insurance and Prior Authorization: What You Need to Know
Most insurance plans will automatically switch you to an authorized generic when it’s available. You won’t even be asked. That’s good - it means lower costs. But if you’re on a specialty medication, you might need prior authorization. Check your plan’s formulary. Look for the drug name and see if “authorized generic” is listed as preferred. If you’re denied coverage for the brand, it’s usually because the plan requires the cheaper version. That’s legal. It’s also smart. If you’re worried about switching, call your insurer. Ask: “Will my authorized generic be covered at the same tier as the brand?” If they say yes, you’re good. If they say no, ask why - and whether you can appeal.What About Side Effects or Effectiveness?
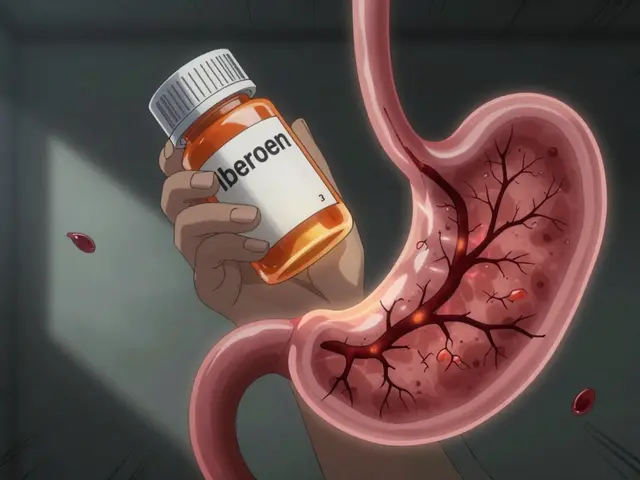
A 2018 study published in the National Center for Biotechnology Information tracked patients who switched from brand to authorized generic. Results? No difference in hospitalization rates. No increase in medication discontinuation. No drop in adherence. The American Academy of Allergy, Asthma & Immunology confirms: authorized generics have the same inactive ingredients as the brand. That’s important for people with sensitivities - like lactose intolerance or dye allergies. If your brand doesn’t contain gluten or FD&C Red 40, the authorized generic won’t either. Still, if you feel different after switching - even slightly - tell your doctor. It’s rare, but possible. Sometimes, the change in pill size or coating affects absorption in people with severe digestive issues. But for 99% of patients, there’s no issue.How to Make the Switch Smooth
Here’s a simple 5-step plan:- Check your prescription. Is it still the brand name? Ask your doctor if switching is an option.
- Visit the FDA’s authorized generic list and confirm one exists for your drug.
- Call your pharmacy. Ask if they carry the authorized version and if it’s in stock.
- Ask your pharmacist to explain the difference between the brand and the authorized generic. Write it down if you need to.
- Fill the prescription. Keep the old bottle for a few days in case you have questions.
What If Your Doctor Refuses to Switch?
Some doctors still prefer brand names out of habit. Or they’re not aware of the authorized generic option. That’s okay. But you have the right to ask for a switch. Bring the FDA list with you. Say: “I found an authorized generic for this drug. It’s made by the same company. Can we try it?” Most doctors will agree. If they say no, ask why. Is it because of a medical reason? Or just because they’ve always prescribed the brand? You’re not asking for a favor. You’re asking for a cost-effective, clinically equivalent option. That’s your right.Long-Term Trends: Is This Here to Stay?
Authorized generics are growing. From 2020 to 2022, their introductions jumped 22% year over year. By 2025, analysts predict 45% of top-selling brand drugs will have an authorized version within six months of generic competition. Why? Because it’s smart business for manufacturers. They keep market share, avoid price crashes from multiple generics, and still offer savings to patients. And with the FDA improving transparency - now integrating AG data into pharmacy systems - it’s easier than ever to know what you’re getting. The future? More authorized generics for complex drugs, including biosimilars. Morgan Stanley predicts 35% of biologics losing patent protection by 2028 will have authorized versions. That’s huge for patients with conditions like rheumatoid arthritis or diabetes who pay hundreds a month for injectables.Final Thought: You’re Not Taking a Risk - You’re Making a Smart Choice
Switching from brand to authorized generic isn’t a compromise. It’s a win. You get the same medicine. Same effectiveness. Same safety. Lower price. No downside. The fear comes from confusion. Once you understand that an authorized generic isn’t a knockoff - it’s the real thing with a different label - the choice becomes obvious. Next time your pharmacy calls to say your prescription changed, don’t panic. Check the label. Check the FDA list. Ask a question. You might just save yourself hundreds a year - without changing how you feel.Is an authorized generic the same as a regular generic?
No. A regular generic is made by a different company and must prove it’s bioequivalent to the brand. An authorized generic is made by the original brand company, using the exact same formula, ingredients, and manufacturing process. It’s the same pill, just sold without the brand name.
Can I ask my doctor to prescribe an authorized generic?
Yes. You can ask your doctor to write the prescription for the authorized generic specifically. Some doctors do this automatically. Others may need to be reminded that it’s an option. Bring the FDA’s list to your appointment to make it easier.
Why does my authorized generic look different from the brand?
Even though it’s made by the same company, the packaging and pill appearance might change to avoid confusion with the brand version. Color, shape, or imprint differences are cosmetic and don’t affect how the drug works. The active ingredient and dosage are identical.
Will my insurance cover the authorized generic?
Yes - and it usually will automatically. Most insurance plans require you to use the authorized generic if it’s available because it’s cheaper. You’ll typically pay less out of pocket. If you’re denied, ask for a formulary exception or appeal.
Are there any risks in switching to an authorized generic?
For the vast majority of people, there are no risks. Authorized generics are identical to the brand in every way that matters: active ingredients, dosage, safety, and effectiveness. Rare cases of sensitivity to inactive ingredients can occur, but these are the same in both the brand and the authorized version. If you feel unusual symptoms after switching, contact your doctor.


Comments (14)
Margaret Stearns
i was scared to switch too but my script went from $210 to $28 and i didnt feel any different. the pill just looked weird at first lol
Scotia Corley
It is imperative to underscore that the regulatory equivalence of authorized generics is not merely a marketing ploy-it is a scientifically validated reality under the auspices of the FDA’s Orange Book. To conflate this with standard generics is to misunderstand the pharmacological integrity of the supply chain.
Debbie Naquin
the real question isn't whether it's the same pill-it's why the system forces us to question the very thing we're prescribed. if the drug is identical, why does the brand even exist? capitalism turned medicine into a branding exercise. the pill doesn't care about logos.
Karandeep Singh
usa pharma is scam. india generics better. cheaper and same. why pay more?
Mary Ngo
have you ever considered that the FDA and big pharma are in cahoots? the 'authorized generic' is a trap. they're testing subtle psychological conditioning on patients-making you accept lower quality while paying less. next they'll say your insulin is 'equivalent' even if it's made in a factory that uses tap water.
James Allen
so let me get this straight-some guy in a lab coat says the pill is the same, but it's got a different color? that's not science, that's a conspiracy. and now you're telling me my insurance company is the hero? please. america's healthcare system is a joke. i'm sticking with the brand. if it ain't broke, don't fix it.
Kelly Essenpreis
why do we even have brand names if theyre the same thing this is ridiculous
Alexander Williams
the bioequivalence metrics for authorized generics are functionally identical to the NDA, but the inactive excipient profiles are often obfuscated in the FDA’s public database. unless you cross-reference the ANDA supplement filings, you're operating on incomplete data.
Suzanne Mollaneda Padin
i work in a pharmacy and i see this every day. patients panic when the pill changes color, but 9 out of 10 say they feel better after switching because their bills are lower. we keep a printed list of authorized generics behind the counter. if you’re unsure, just ask. we’re here to help.
Erin Nemo
my mom switched to the authorized generic for her blood pressure med and now she has extra cash for groceries. no side effects. no drama. just cheaper pills. why is this even a thing?
ariel nicholas
...but what if... the authorized generic... is actually... a placebo... with... the same active ingredient?... and... the... FDA... is... complicit... because... they... are... funded... by... pharma...?
Rachel Stanton
if you're on a complex med like a biologic or a long-acting injectable, the authorized generic isn't just about cost-it's about access. many patients can't afford the brand, and without the AG option, they skip doses or stop entirely. this isn't just economics-it's public health.
Bonnie Youn
you guys are overthinking this. if it's the same pill, just cheaper, why are you still scared? you're not losing anything. you're gaining money. go get that generic and treat yourself to coffee with the savings. you deserve it!
Edward Hyde
pharma is a racket. they make you pay $300 for a pill that costs 50 cents to make, then they slap a fake label on it and call it 'authorized' like that makes it ethical. this isn't innovation-it's exploitation dressed up as savings.