
What Is REM Sleep Behavior Disorder?
REM sleep behavior disorder (RBD) isn’t just tossing and turning in your sleep. It’s when your body doesn’t shut down during REM sleep-the stage where most dreaming happens. Normally, your muscles are paralyzed during this phase to keep you from acting out dreams. With RBD, that paralysis fails. You might punch, kick, yell, or jump out of bed while dreaming about being chased, fighting, or falling. These aren’t random movements. They’re direct enactments of vivid, often violent dreams.
People with RBD often don’t remember the episodes themselves. But their bed partners do. One woman told her doctor her husband had broken her collarbone during a dream about defending himself from an intruder. Another man kicked so hard he shattered a bedside lamp. These aren’t rare cases. Studies show up to 78% of people with RBD make changes to their bedrooms-removing sharp furniture, installing bed rails, or even sleeping in separate rooms to avoid injury.
What makes RBD especially concerning is what it might signal. About 90% of people diagnosed with RBD eventually develop a neurodegenerative disease like Parkinson’s, dementia with Lewy bodies, or multiple system atrophy. For many, RBD appears years-sometimes decades-before other symptoms. That’s why doctors now see RBD not just as a sleep problem, but as an early warning sign.
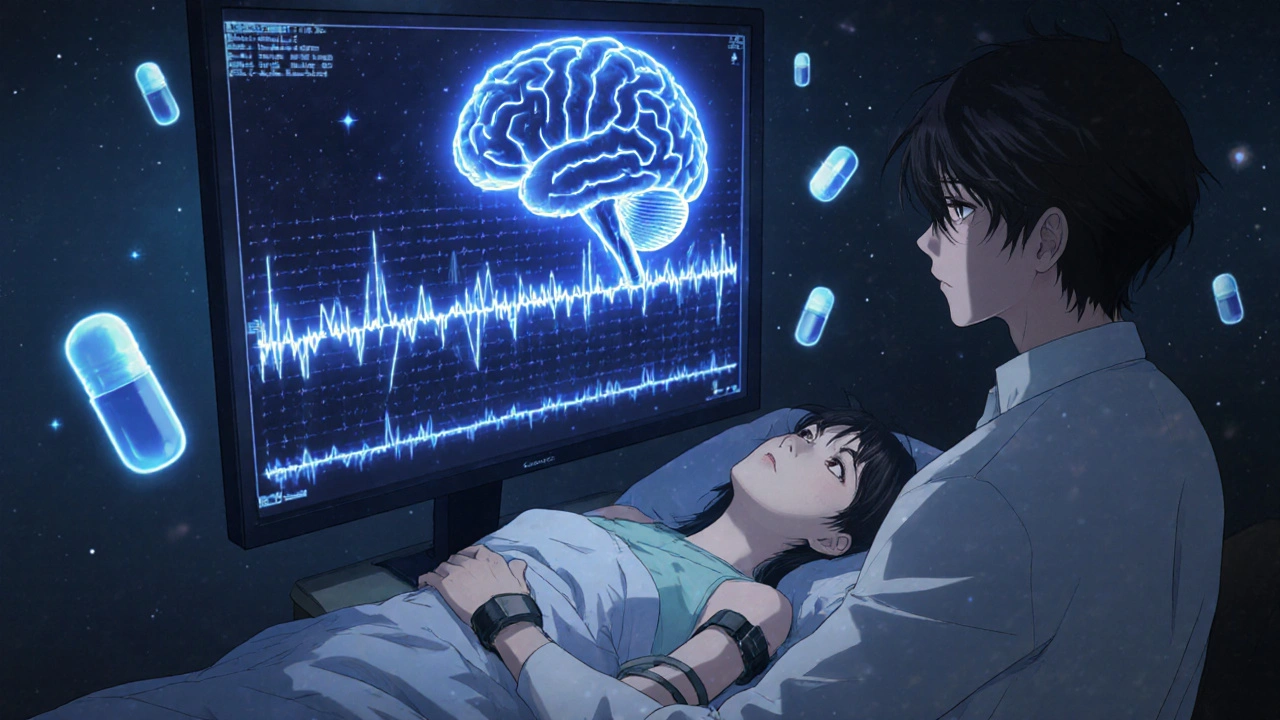
How Is RBD Diagnosed?
You can’t diagnose RBD with a questionnaire alone. The gold standard is a sleep study called polysomnography (PSG). During this overnight test, sensors track brain waves, eye movements, heart rate, breathing, and muscle activity. The key finding? REM sleep without atonia (RSWA). That means your muscles are active during REM sleep when they should be completely still.
The International Classification of Sleep Disorders requires that muscle activity during REM sleep exceeds 15% of the time in at least one 30-second epoch. In practical terms, this means doctors see clear spikes in leg or arm movement on the EEG readout while you’re dreaming. On average, people with RBD show complex movements about 4.2 times per hour during sleep.
Doctors also rule out other causes. Seizures, sleep apnea, or even certain medications can mimic RBD. A full neurological exam is part of the process. If you’re over 50 and have no known neurological condition but are acting out dreams, RBD is likely. If you’re younger, doctors will check for possible triggers like antidepressants or substance use.
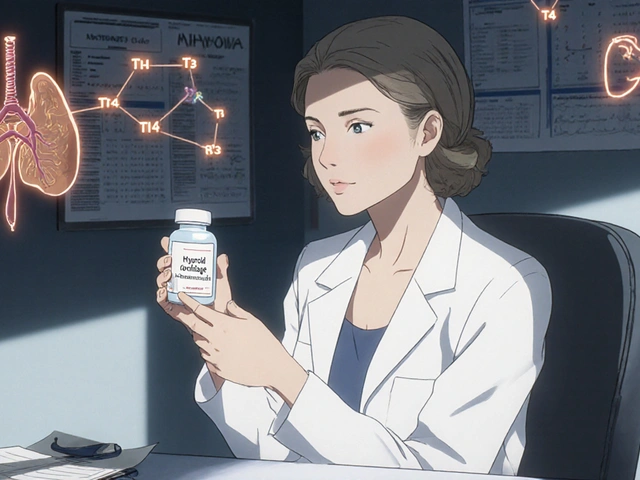
First-Line Medications: Melatonin and Clonazepam
There are no FDA-approved drugs specifically for RBD. That means doctors rely on off-label treatments with strong clinical support. The two most common are melatonin and clonazepam.
Melatonin is a natural hormone your body makes to regulate sleep. In RBD, high-dose melatonin (3-12 mg) helps restore muscle inhibition during REM sleep. A 2010 randomized trial found 62.5% of patients saw a significant drop in dream enactment. Side effects are mild: occasional morning grogginess or headaches. One 68-year-old patient reduced his weekly episodes from seven to one after starting 6 mg nightly. Most doctors start at 3 mg and increase by 3 mg every two weeks until symptoms improve or side effects appear.
Clonazepam, a benzodiazepine, works faster and more powerfully. It boosts GABA, a calming brain chemical that suppresses muscle movement. Studies show 80-90% of patients respond. In one 2000 study, 88.7% had fewer or no episodes after starting 0.5 mg at bedtime. Many see results in just a few days. But it comes with risks. Dizziness affects 22% of users. Unsteadiness? 18%. Daytime sleepiness? 15%. For older adults, the risk of falls increases by 34%. Some patients stop taking it after just three months because they feel unsteady walking or fear falling.
Many neurologists now prefer melatonin as the first try-especially for older adults or those with balance issues. About 58% of neurologists start with melatonin, according to a 2022 survey of 450 specialists. Only 32% start with clonazepam.
Other Medications and Emerging Options
When melatonin and clonazepam don’t work-or aren’t safe-doctors turn to other options. Pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome, helps about 60% of RBD patients. It’s often chosen if the person also has RLS. Doses are low: 0.125-0.5 mg daily.
Rivastigmine, a cholinesterase inhibitor used in Alzheimer’s and dementia, showed promise in one small trial for patients with RBD and mild cognitive decline who didn’t respond to standard treatment. It’s not widely used yet, but it’s a potential option for those already showing early memory issues.
The most exciting new direction involves dual orexin receptor antagonists. Orexin is a brain chemical that regulates wakefulness. Drugs like suvorexant (Belsomra) and the experimental NBI-1117568 block orexin receptors, which may calm overactive motor circuits during REM sleep. Mount Sinai research in October 2023 showed a 78% drop in dream enactment behaviors in animal models. The FDA granted Fast Track status to NBI-1117568 in January 2023. Phase II trials are underway, with results expected in 2024. If successful, these could offer effective relief without the dizziness, dependence, or fall risks of current drugs.
Neurological Monitoring: Why It Matters
Treating RBD isn’t just about stopping the kicks and yells. It’s about watching for what comes next. About 73.5% of people with idiopathic RBD (meaning no known cause) develop Parkinson’s, dementia with Lewy bodies, or multiple system atrophy within 12 years. That’s not a guess-it’s backed by long-term studies published in the Journal of Clinical Sleep Medicine.
Because of this, the American Academy of Neurology recommends annual neurological checkups for anyone diagnosed with RBD. These aren’t just for confirmation. They’re for early detection. Doctors look for subtle signs: reduced sense of smell, constipation, slight tremors, or changes in voice or facial expression. These can appear years before a Parkinson’s diagnosis.
One 2019 study in Lancet Neurology found that 6.3% of RBD patients convert to a neurodegenerative disease each year. That means over a decade, nearly two-thirds will show signs. Early detection gives patients time to plan, join clinical trials, or start neuroprotective strategies. It also helps families prepare emotionally and logistically.
Safety First: Modifying the Sleep Environment
Medication helps-but it doesn’t always stop every episode. That’s why safety modifications are just as important. The Cleveland Clinic recommends these steps for anyone with moderate to severe RBD:
- Remove all weapons, sharp objects, or glass from the bedroom
- Pad sharp corners of furniture with foam or cushions
- Place thick rugs or mats beside the bed
- Install bed rails or use a mattress on the floor
- Consider sleeping in separate beds or rooms if episodes are violent or frequent
These aren’t extreme measures. In fact, 78% of RBD patients already make at least one of these changes. One husband who used to punch his wife during dreams now sleeps on a mattress on the floor. His wife says she hasn’t been hurt since.
Alcohol is another hidden trigger. Even one or two drinks can worsen RBD in 65% of patients. So if you have RBD, avoid alcohol entirely-especially close to bedtime.
What to Expect When Starting Treatment
Medication response varies. With melatonin, it takes time. Most patients need to stay at each dose (3 mg, then 6 mg, then 9 mg) for two to four weeks before seeing results. Don’t give up after a week. Clonazepam often works faster-sometimes within days-but must be tapered slowly. Stopping abruptly can cause rebound nightmares or agitation in 38% of people.
Side effects matter. If you feel dizzy, unsteady, or overly sleepy after starting clonazepam, talk to your doctor. Lowering the dose or switching to melatonin might be safer. Melatonin’s side effects are rare and mild, making it a better long-term option for many.
Track your episodes. Keep a simple log: date, time, type of movement, intensity, and whether you woke up during it. Share this with your neurologist at each visit. It helps them adjust treatment and spot patterns.
Why RBD Is More Than a Sleep Problem
RBD is a window into the brain’s future. It’s one of the strongest predictors of neurodegenerative disease we have. That’s why researchers are now focusing on RBD not just as a symptom to treat-but as a target for prevention.
Drug companies are pouring money into this space. The global RBD treatment market is projected to grow to $1.2 billion by 2023 and keep rising. Clinical trials are testing drugs that might slow or stop the brain changes that lead to Parkinson’s. If successful, treating RBD could one day prevent Parkinson’s altogether.
For now, the goal is safety and symptom control. But the bigger picture is hope: that by catching RBD early, we might one day stop neurodegenerative diseases before they start.
Frequently Asked Questions
Can REM sleep behavior disorder go away on its own?
No, RBD does not resolve on its own. It’s a chronic condition that typically worsens over time without treatment. While medications can control symptoms effectively, the underlying neurological changes linked to RBD-especially the risk of developing Parkinson’s or dementia with Lewy bodies-progress independently. Stopping treatment often leads to a return of dream enactment behaviors, sometimes even more severe than before.
Is melatonin safer than clonazepam for older adults with RBD?
Yes, melatonin is generally safer for older adults. Clonazepam increases the risk of falls, dizziness, confusion, and daytime sedation-risks that rise sharply after age 65. Melatonin, on the other hand, has minimal side effects, with only about 8% of users reporting mild headaches or grogginess. For elderly patients, especially those with balance issues or a history of falls, melatonin is the preferred first-line treatment according to the American Academy of Sleep Medicine’s 2023 guidelines.
How long does it take for RBD medication to work?
Clonazepam often works within a few days-many patients report fewer episodes after the first night. Melatonin takes longer: it usually requires 2 to 4 weeks at a given dose to show full effect. Doctors recommend staying at 3 mg for at least two weeks before increasing to 6 mg, then waiting again before going higher. Patience is key with melatonin, but the results are often more sustainable and safer long-term.
Can antidepressants cause RBD?
Yes. Certain antidepressants-especially SSRIs and SNRIs-are known to trigger or worsen RBD symptoms in susceptible individuals. In fact, up to 50% of RBD cases diagnosed in younger adults are linked to antidepressant use. If RBD develops after starting an antidepressant, a neurologist may consider switching medications or adding melatonin to counteract the effect. Never stop antidepressants without medical supervision.
Should I sleep in a separate room if I have RBD?
It depends on the severity. Many couples choose separate rooms for safety, especially if episodes involve violent movements, kicks, or punches. About 42% of RBD patients end up sleeping apart from their partners, even with medication. If your partner is at risk of injury, or if you both aren’t getting rest, separate sleeping arrangements are a reasonable, practical step-not a failure. Safety and sleep quality for both people are the top priorities.
Is RBD hereditary?
RBD itself isn’t directly inherited, but there may be a genetic predisposition to the neurodegenerative diseases it predicts-like Parkinson’s or dementia with Lewy bodies. Some families have multiple members with these conditions, suggesting shared genetic risk factors. However, most cases of RBD occur in people with no family history. The main risk factors are age (over 50), male gender, and the presence of other neurological symptoms.

Comments (12)
Rachel Wusowicz
I've been watching this for years... and let me tell you, the government knows about RBD. They've been suppressing the truth: it's not just neurodegeneration, it's electromagnetic mind control triggering REM atonia failure. The pills they give you? Placebos laced with neurotoxins to keep you docile. I've modified my bedroom with aluminum foil-lined walls, salt crystals under the mattress, and a Faraday cage around my bed. I haven't kicked anyone in 14 months. They don't want you to know this.
Melanie Taylor
OMG this is SO important!! 🙌 I just started melatonin after my husband nearly threw our TV across the room during a dream about fighting aliens... and now he sleeps like a baby 😊 I wish more people knew how safe it is!! #RBDWarrior #MelatoninIsMagic
Teresa Smith
The clinical data presented here is methodologically sound and aligns with current neurology consensus. The prioritization of melatonin over clonazepam in elderly populations reflects a responsible risk-benefit calculus grounded in geriatric pharmacology. Furthermore, the longitudinal neurological monitoring protocol recommended by the AAN is not merely prudent-it is ethically imperative. This post constitutes a model of evidence-based patient education.
ZAK SCHADER
Melatonin? That's just sugar pills made in China. Clonazepam is the real deal. Why are they pushing this hippie nonsense? In my day, we just locked the door and let 'em scream. America used to be strong. Now we give out vitamins instead of real medicine. Wake up people.
Danish dan iwan Adventure
RBD is a prodromal biomarker of synucleinopathy. The RSWA on PSG is the electrophysiological signature. Melatonin modulates MT1/MT2 receptors in the SCN, restoring GABAergic inhibition. Clonazepam enhances GABA-A activity. The real issue is neuroinflammation. You're treating symptoms, not the underlying alpha-synuclein aggregation. You need disease-modifying agents.
Ankit Right-hand for this but 2 qty HK 21
All this talk about melatonin and clonazepam? Total Western weakness. In India, we just slap them awake. No meds. No pillows. No bed rails. If you're dreaming you're fighting a tiger, you better be ready to fight. Sleep is for the weak. You want to live? Train your brain. No pills. No fear.
Oyejobi Olufemi
You think this is about sleep? NO. This is about the collapse of the human spirit. We've become so disconnected from our primal selves that our brains rebel in REM. The pharmaceutical industry profits from your fear. They sell you melatonin like it's holy water. But the truth? You're being slowly poisoned by processed food, WiFi, and emotional repression. The body doesn't lie. It kicks. It screams. It remembers what your soul forgot.
Daniel Stewart
There's a certain tragic poetry to RBD-it’s the unconscious mind’s last act of rebellion against the constraints of waking life. We suppress our instincts, our rage, our primal fears, and then, in the sanctuary of sleep, the body erupts. Perhaps the real treatment isn’t medication, but the courage to confront what we refuse to acknowledge while awake.
Latrisha M.
This is one of the most clear-headed, practical guides I've seen on RBD. Safety first-removing sharp objects, sleeping apart if needed, avoiding alcohol. No drama. No hype. Just facts. Melatonin is the way to go for most people. And tracking episodes? Essential. If you're reading this and you're scared-start here. You're not alone.
Jamie Watts
Bro melatonin is just a supplement so it dont even count as real medicine. Clonazepam is the only thing that works. I tried the melatonin thing for 3 weeks and my wife still got kicked in the face. Then I went to my doc and got the real stuff. 0.5mg and boom no more nightmares. You think its safe? It is if you dont drink and dont drive. Stop listening to influencers and talk to a real neurologist
John Mwalwala
RBD is a gateway. The brain’s motor cortex is being hijacked by prions. The REM atonia failure? That’s the first crack in the blood-brain barrier. The 90% statistic? That’s not coincidence-that’s a countdown. The FDA knows. The pharma giants know. They’re testing orexin blockers because they’re not trying to cure RBD-they’re trying to stop the next pandemic of neurodegeneration. We’re all walking time bombs. This isn’t sleep. It’s surveillance.
Deepak Mishra
I had RBD for 5 years!!! 😭 My wife left me bc I kicked her in the ribs during a dream about being chased by a dragon!!! 😭 Then I tried melatonin 9mg and now I just twitch a little 😍 I even made a TikTok about it and got 12k followers!!! 🙌 #RBDRecovery #SleepWarrior #DreamsAreReal