
Take a pill, and within minutes your skin breaks out in itchy red bumps. Or maybe it’s days later-your body feels like it’s fighting a fever, your joints ache, and a rash spreads across your chest. You didn’t get sick from the flu. You might be having a drug allergy.
Not every bad reaction to medicine is an allergy. Some are just side effects-nausea from antibiotics, dizziness from blood pressure pills. But a true drug allergy means your immune system mistakes the medication for a threat and attacks it. That’s when things get dangerous.
What a Drug Allergy Actually Feels Like
Drug allergies don’t look the same for everyone. Some people get a mild rash. Others go into full-blown shock. The most common sign? A skin reaction. It might be hives-raised, red, itchy welts that come and go. Or it could be a flat, red rash that spreads slowly over days. Itching is almost always there. Sometimes, your lips or eyelids swell up. That’s angioedema. It’s not just uncomfortable-it can block your airway.
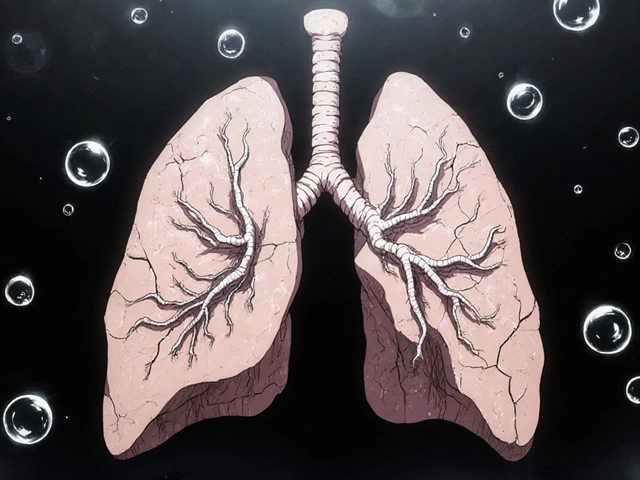
But skin isn’t the only place symptoms show up. If your throat tightens, you start wheezing, or you feel like you can’t breathe, that’s a red flag. Nausea, vomiting, diarrhea, or dizziness can also be part of the picture. The real danger comes when two or more systems react at once. A rash plus trouble breathing? That’s anaphylaxis. It’s not a guess. It’s an emergency.
One study found that over 10% of people in the U.S. think they’re allergic to penicillin. But more than 90% of them aren’t. They had a rash as a kid, got labeled allergic, and never got tested. That’s a problem. Doctors end up prescribing stronger, more expensive antibiotics that can cause worse side effects-like a dangerous gut infection from C. diff. Accurate diagnosis saves lives and money.
Timing Matters: When Symptoms Show Up
Not all drug reactions happen right away. The timing tells you a lot about what you’re dealing with.
If you get hives, swelling, or trouble breathing within an hour of taking a pill, it’s likely an IgE-mediated reaction. That’s the classic allergic response. Penicillin, sulfa drugs, and some painkillers like ibuprofen or naproxen are common triggers. These reactions can escalate fast. One minute you feel fine. The next, you’re struggling to breathe.
Delayed reactions are trickier. A rash might show up three to five days after starting a new medicine. It often looks like small red spots that blend together. Fever, swollen glands, or joint pain might come with it. That could be serum sickness-like syndrome. Or it could be DRESS syndrome-Drug Rash with Eosinophilia and Systemic Symptoms. That one’s rare but serious. It can damage your liver, kidneys, or lungs. Symptoms can linger for weeks after stopping the drug.
Then there’s Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN). These are medical emergencies. You get blisters on your skin and inside your mouth, eyes, or genitals. Large patches of skin start peeling off. It’s like a severe burn from the inside out. These reactions usually happen within weeks of starting a new drug-often antibiotics, seizure meds, or gout treatments.

When to Call 911: The Emergency Red Flags
You don’t need to wait for a doctor if you’re having a severe reaction. Call 911 right away if you have:
- Difficulty breathing or wheezing
- Swelling of the tongue, lips, or throat
- Dizziness, fainting, or a rapid, weak pulse
- Multiple symptoms at once-like a rash plus vomiting or trouble breathing
These are signs of anaphylaxis. It can kill in minutes. Don’t wait to see if it gets better. Don’t drive yourself. Call for help. If you have an epinephrine auto-injector (like an EpiPen), use it immediately. Then call 911 anyway-even if you feel better after the shot. The reaction can come back.
Even if you’re not sure it’s an allergy, don’t ignore it. If you’ve never had a reaction before and suddenly develop a rash after starting a new drug, stop taking it and call your doctor. Take a picture of the rash. That helps them identify it later.
How Doctors Diagnose a Drug Allergy
There’s no blood test that can catch every drug allergy. That’s why diagnosis is often based on your story.
Your doctor will ask: When did you take the drug? What exactly happened? How long did it take for symptoms to show up? Did you have more than one symptom? Did you get better after stopping the medicine? Did you take the same drug again? (Don’t try this at home.)
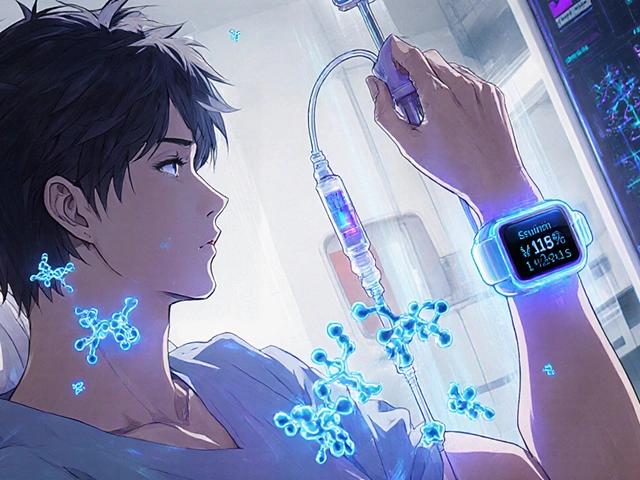
For penicillin, there’s a reliable test. A skin prick test uses tiny amounts of penicillin to see if your skin reacts. If that’s negative, you might get a small oral dose under supervision. If you don’t react, you’re not allergic. Most people who think they are, aren’t.
For other drugs, testing is harder. If you had a severe delayed reaction like DRESS or SJS, your doctor might order blood tests to check for high white blood cell counts or liver damage. But there’s no simple skin test for most antibiotics, painkillers, or chemotherapy drugs.
That’s why mislabeling is so common. Someone gets a rash after taking amoxicillin as a kid. Years later, they’re told they’re allergic. They avoid penicillin, even though the rash was probably just a virus. Now, they’re stuck with a different antibiotic that’s less effective and more likely to cause side effects.
What Happens After a Reaction
Once you’ve had a confirmed drug allergy, you need to avoid that drug and similar ones. But you also need to make sure your medical records reflect it correctly. Tell every doctor, pharmacist, and ER nurse. Wear a medical alert bracelet if you’ve had a severe reaction.
Keep a list of all drugs you’ve reacted to, including the symptoms and timing. Bring it to every appointment. If you’re unsure whether a new medicine is safe, ask your pharmacist or allergist. Don’t assume a drug is okay just because it’s in the same class.
If you’ve had a serious reaction, see an allergist. They can help you understand what you’re truly allergic to-and what you’re not. Many people who think they’re allergic to multiple drugs turn out to be allergic to just one. Getting tested can open up safer, cheaper treatment options.
Why This Matters More Than You Think
Every year in the U.S., over 1.3 million people go to the emergency room because of drug reactions. Many of those are avoidable. Mislabeling allergies leads to worse outcomes: longer hospital stays, higher costs, and more dangerous infections.
Penicillin is the most commonly mislabeled allergy. But it’s also one of the safest, most effective antibiotics-if you’re not allergic. If you’ve been told you’re allergic but never got tested, you might be denying yourself the best treatment for your next infection.
And if you’ve had a severe reaction, you’re not just protecting yourself-you’re protecting your family. A child with a drug allergy might need a different vaccine or treatment. A pregnant person might need a safer painkiller. Accurate information saves lives across generations.
Drug allergies are rare-but their impact is huge. The key isn’t avoiding all medicines. It’s knowing which ones are truly dangerous for you. And that starts with recognizing the signs-and acting fast when they show up.


Comments (15)
Lisa Davies
This is so important!! 🙌 I had a friend who got labeled penicillin-allergic after a toddler rash-turned out it was roseola. She’s been on super expensive antibiotics for years. So glad someone’s putting this out there.
Doctors need to stop treating allergies like a checkbox and start treating them like a puzzle.
Michelle M
It’s wild how we treat drug allergies like they’re permanent tattoos when they’re often just misread signals from our bodies. We fear what we don’t understand. But knowledge? Knowledge is the real medicine.
Testing isn’t just about avoiding danger-it’s about unlocking better care. We owe it to ourselves to ask: ‘Am I allergic… or just unlucky with a virus?’
Raj Kumar
i had a rash after amoxicillin when i was 7. mom freaked out. now im 32 and i just got tested. turns out im not allergic. my doc was like 'youve been avoiding the best antibiotic for 25 years lol'. mind blown.
John Brown
This hits different if you’ve ever been in the ER with someone having anaphylaxis. One minute they’re laughing, next they’re gasping. No time for doubt. If you see swelling + trouble breathing? Call 911. No ‘maybe’s. No ‘I’ll wait.’
Christina Bischof
i used to think allergies were just itchy skin until my cousin got sjs from an antibiotic. skin peeled off her arms like sunburn. she was in the icu for weeks. never take a rash lightly after a new med
Nupur Vimal
everyone thinks theyre allergic to penicillin because they got a rash as a kid but nobody ever tells you that viruses cause rashes too and its not an allergy its just bad timing and you idiots keep paying for worse drugs
Sai Nguyen
India has the same problem. Doctors prescribe antibiotics like candy. Parents panic at a rash. Kid gets labeled allergic. Later, they get TB and can’t use first-line drugs because ‘penicillin allergy’ on file. This isn’t health-it’s superstition.
Benjamin Glover
It’s embarrassing how many Americans confuse side effects with allergies. Nausea isn’t an immune response. Dizziness isn’t anaphylaxis. You’re not ‘allergic to caffeine’ because you jitter. This isn’t science-it’s self-diagnosis culture.
John Samuel
As someone who works in ER triage, I’ve seen too many patients with ‘penicillin allergy’ on their charts who’ve never been tested. We end up giving vancomycin or clindamycin-more expensive, more toxic, more likely to cause C. diff.
One simple skin test can save a life, a hospital bed, and thousands of dollars. Why isn’t this standard?
Cassie Henriques
DRESS syndrome is underdiagnosed because it mimics viral illness-fever, lymphadenopathy, eosinophilia. But if you’re on an anticonvulsant or allopurinol and develop a rash + transaminitis after 2+ weeks? That’s a red flag.
Biopsy + eosinophil count + drug rechallenge (in controlled setting) = gold standard. Too many docs miss this.
Jocelyn Lachapelle
i got a rash after ibuprofen once and thought i was allergic so i stopped taking it for 10 years until i got a migraine and my dr said try it again. no reaction. i feel so dumb but also so relieved
Melissa Taylor
I’m so glad someone mentioned the medical alert bracelet. My mom wore one after her anaphylaxis to sulfa drugs. When she collapsed at the grocery store, the paramedics saw it and knew exactly what to do. It saved her life. Don’t underestimate the power of a little metal tag.
Jake Sinatra
The data is clear: over 90% of self-reported penicillin allergies are false. Yet hospitals still treat them as absolute contraindications. This isn’t caution-it’s institutional inertia. We need mandatory allergy re-evaluation protocols for adults over 40.
Mike Nordby
I work in pharmacology. We have no reliable in vitro test for 80% of drug allergies. Diagnosis remains clinical. That’s why history matters more than labs. Documenting onset, progression, resolution, and recurrence is the only way to build accurate profiles. Stop relying on secondhand reports.
RONALD Randolph
This article is a joke. You’re telling people to just ‘get tested’ like it’s a routine blood draw? In the U.S., allergists are booked 6 months out. And insurance denies it unless you’ve had a near-death experience. This isn’t helpful-it’s tone-deaf.