
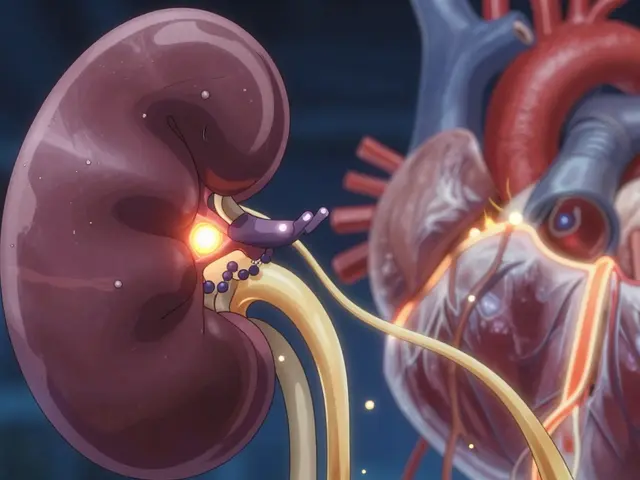
Every year, millions of people take generic drugs made in one country and used in another. But when something goes wrong - a rare side effect, a dangerous interaction, an unexpected reaction - how do we know fast enough to stop it? That’s where pharmacovigilance comes in. And right now, the world is trying to make it work the same way everywhere.
Why harmonization matters more than ever
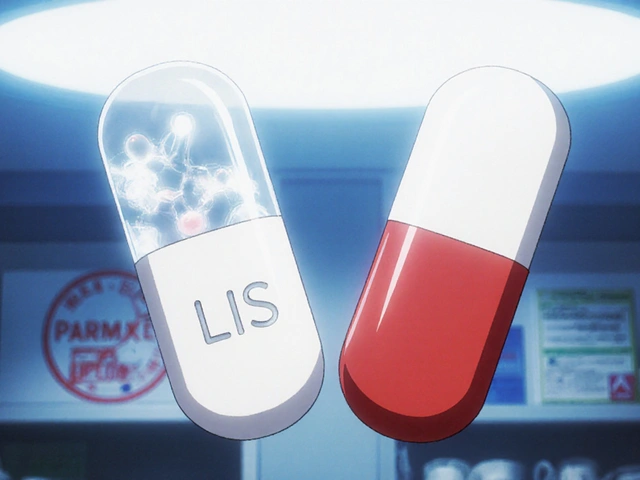
Imagine you’re a pharmacist in Brazil. A patient comes in with a strange rash after taking a generic blood pressure pill made in India. You report it. But that report doesn’t automatically reach regulators in the U.S. or Europe. Without a shared system, that same reaction might go unnoticed for months - or years - while others take the same drug and suffer the same fate. That’s the problem international pharmacovigilance tries to fix. The goal isn’t just to collect more data. It’s to make sure the right data gets to the right people at the right time, no matter where the drug was made or where it’s being used. The push for harmony started in 1990 with the International Council for Harmonisation (ICH). Back then, the U.S., EU, and Japan realized they were all doing the same work - but in different ways. Each had their own forms, deadlines, coding systems. Companies had to submit the same safety report three times, just with different formatting. It wasn’t just inefficient. It was dangerous. Today, the ICH’s E2 series guidelines are the backbone of global safety monitoring. E2B(R3) standardizes how individual case safety reports are sent electronically. E2E defines how risk management plans should be written. PSURs (Periodic Safety Update Reports) now follow a single template used from Canada to China. The result? Companies like Novartis cut duplicate case entry by 92%. Signal detection sped up by 38 days on average.How the big players do it differently
Even with harmonization, the world doesn’t move in lockstep. The U.S., EU, and Japan - the original ICH members - still lead the way. But their rules aren’t identical. In the U.S., the FDA only requires expedited reporting for serious adverse events that the sponsor believes are related to the drug. That’s a narrow filter. In the EU, the EMA demands expedited reporting for every serious event, regardless of whether the company thinks it’s linked. That means European teams process twice as many reports. One pharmacovigilance manager on Reddit said they spend 35-40% of their time just rewriting reports to fit different regional formats. Japan’s PMDA uses its J-STAR system to analyze 12 million patient records from real-world data. It’s one of the most advanced systems in the world. China’s NMPA, meanwhile, requires local reporting within 15 days - the same deadline as the FDA - but without full integration into global databases. That creates a parallel reporting stream that doubles the workload for global companies. Canada’s Health Canada aligns closely with ICH standards but keeps its own 30-day rule for serious events. It’s a middle ground - not as strict as the EU, not as selective as the FDA. But it still adds complexity. The real global database? VigiBase. Run by the WHO, it holds over 35 million individual case reports from 134 countries. It’s the only place you can see the full picture - from a rare reaction in rural Kenya to a new side effect in Germany. But here’s the catch: only 31% of low- and middle-income countries have fully adopted the ICH E2B(R3) standard. That means millions of reports are still stuck in paper files, faxes, or unstructured digital forms that VigiBase can’t easily read.Technology is changing the game - but unevenly
The biggest leap forward in recent years isn’t in policy. It’s in technology. The FDA and EMA started using machine learning to scan safety reports in 2022. Their systems now detect potential safety signals 30-40% faster than manual review. Japan’s AI models cut false positives by 25%. That’s huge. Fewer false alarms mean teams can focus on real threats. But this tech isn’t available everywhere. The EU mandates that pharmacovigilance systems integrate with electronic health records. In Brazil and South Africa, fewer than 15% of potential data sources are even digitized. A hospital in Nairobi might still use paper logs. A clinic in rural Indonesia might not have internet. That’s why the WHO’s Global Smart Pharmacovigilance Strategy - currently being revised after a 2024 meeting in New Delhi - is so critical. It aims to set common data standards across 150 countries by 2027. Without this, the gap between rich and poor nations will keep widening.
What’s really holding things back?
The biggest obstacle isn’t technology. It’s money and training. A 2023 Deloitte report found that fully harmonizing global pharmacovigilance could save $2.3 billion a year and prevent 1,200-1,500 deaths annually. But closing the gap requires $1.8 billion in infrastructure investment - mostly in low- and middle-income countries. Training is another wall. A 2024 survey by the American College of Clinical Pharmacology found that 76% of top pharma companies now require their safety teams to understand basic machine learning. But in many countries, pharmacovigilance staff are still learning how to use Excel spreadsheets. MedDRA coding - the universal language for adverse event terms - causes 18-22% of rejected reports in the EU alone because people use different terms for the same symptom. And then there’s the human factor. One pharmaceutical executive told me, “We’ve automated 80% of our reporting. But we still have five people whose only job is to translate EU reports into FDA format.” That’s not innovation. That’s bureaucracy.What’s next? The road to true global alignment
The good news? Progress is real. In January 2024, the FDA, EMA, and PMDA formed a Joint Pharmacovigilance Task Force. They’ve already aligned 78% of their risk management plan requirements for new biologic drugs. That’s a huge step. The ICH announced in March 2024 it’s creating new standards for validating AI tools in pharmacovigilance - with implementation expected by mid-2026. That means companies won’t have to build different AI models for each region. One model, one validation process, global use. Adoption is climbing too. 95% of U.S. and EU companies fully follow ICH E2 guidelines. Only 42% in emerging markets do. But that’s up from 25% in 2018. The future isn’t about forcing everyone to copy the EU or the FDA. It’s about building a shared system where:- Every adverse event report - whether from Tokyo or Tanzania - uses the same format (E2B(R3))
- AI tools are trained on global data and validated under one standard
- Real-world data from hospitals, pharmacies, and clinics flows into VigiBase automatically
- Training and funding follow the need, not the GDP

What this means for patients and companies
For patients, this is about safety. Faster detection of dangerous drugs means fewer avoidable deaths. It means a generic drug made in India can be trusted as safely in Canada as it is in Germany. For companies, it’s about cost and speed. Harmonization cuts reporting time, reduces duplication, and speeds up market access. The FDA estimates it shortens time-to-market by 15-20%. That’s billions in savings. But the real win? Trust. When regulators, manufacturers, and patients know the system works the same way everywhere, confidence grows. And that’s what makes global generics sustainable.What you need to know right now
If you’re in the pharma industry:- Make sure your safety team uses ICH E2B(R3) for all global submissions
- Start training staff in basic data science - it’s no longer optional
- Map your reporting workflows. Where are you wasting time on regional formatting?
- Push for a single global safety database. Don’t let legacy systems hold you back
- Report any unusual reaction to your doctor - even if you think it’s minor
- Ask if your generic drug is tracked in global safety databases
- Know that the system is getting better - but only if you help it
What is pharmacovigilance harmonization?
Pharmacovigilance harmonization means creating consistent global standards for monitoring drug safety. It ensures that adverse event reports, risk management plans, and safety data follow the same format and rules across countries - so regulators and companies can share information faster and catch dangers earlier.
Why do different countries have different reporting rules?
Each country has its own regulatory history, resources, and risk tolerance. The EU takes a precautionary approach - reporting everything serious. The FDA focuses on events linked to the drug. Japan uses massive real-world data. These differences exist because there’s no single global law - only guidelines. Harmonization is about reducing, not eliminating, these gaps.
How does VigiBase help global safety?
VigiBase is the WHO’s global database with over 35 million individual case reports from 134 countries. It’s the only system that lets regulators see patterns across borders - like a sudden spike in liver damage from a generic drug sold in Brazil, India, and South Africa. Without it, many dangerous reactions would stay hidden.
Are AI tools being used in pharmacovigilance?
Yes. The FDA and EMA use AI to detect safety signals 30-40% faster than manual review. Japan’s PMDA uses AI to cut false alarms by 25%. But these tools only work if data is clean and standardized - which is still a challenge in many countries.
Why do emerging markets struggle with pharmacovigilance?
Most lack funding, trained staff, digital infrastructure, and access to real-world data. Only 31% of low- and middle-income countries use the full ICH E2B(R3) standard. Many still rely on paper reports. Without investment, global safety efforts will always have blind spots.
What’s the biggest barrier to full harmonization?
Money. The world needs $1.8 billion to bring basic pharmacovigilance systems up to standard in low- and middle-income countries. Without that, even the best guidelines won’t help. Training and cultural resistance matter too - but funding is the first step.


Comments (11)
Katy Bell
Finally, someone wrote about this without sounding like a corporate brochure. I work in pharma compliance, and honestly? The EU’s ‘report everything’ approach is exhausting - but I get why they do it. One missed signal could mean another patient dies because someone assumed it was ‘just a rash.’
Olanrewaju Jeph
In Nigeria, we still fax adverse event reports to the national drug agency. Sometimes the fax machine breaks, and we wait weeks just to resend. Harmonization isn’t just about standards - it’s about dignity. Our patients deserve to be seen in the same system as yours.
Jennifer Skolney
YES. 😊 I’ve seen teams waste MONTHS rewriting reports just to satisfy regional formats. It’s insane. We need ONE system - not 12 versions of the same form. AI can help, but only if we stop making people do manual copy-paste jail. 💪
Dalton Adams
Let’s be real - most of these ‘global standards’ are just the EU’s rules with a different label. The FDA’s ‘only report what you think is related’ approach is dangerously lazy. If a patient has a stroke after taking a generic, and the company says ‘probably not related,’ do they just ignore it? That’s not science - that’s liability avoidance. 🤦♂️
Javier Rain
This is the kind of stuff that actually saves lives - not just saves money. I’ve worked with teams in Brazil and Kenya, and the passion they have for patient safety? It’s unmatched. We just need to stop treating them like afterthoughts. Give them the tools, not the paperwork.
Kane Ren
Biggest win? When AI stops flagging ‘headache’ as a signal because someone in India reported it 400 times. That’s not a safety issue - that’s a language barrier. We need better context, not more filters.
Suresh Ramaiyan
I grew up in a small town in Tamil Nadu. My mom took a generic BP pill - same one sold in the U.S. - and had a reaction no doctor could explain. We didn’t know where to report it. No one asked. That’s the real cost of fragmentation: silence. We’re not just talking about data formats here - we’re talking about people who vanish into the system. If we can track a package from Delhi to Detroit in 3 days, why can’t we track a dangerous drug reaction in 3 hours?
The WHO’s VigiBase is the closest thing we have to a global heartbeat. But right now, it’s like trying to hear a whisper in a hurricane. We need every clinic, every pharmacy, every hospital - even the ones without internet - to be part of the signal. Not the noise.
It’s not about making everyone copy the EU or the FDA. It’s about building a language everyone can speak. MedDRA isn’t perfect, but it’s a start. Training people to use it shouldn’t be a luxury. It should be mandatory - like handwashing in hospitals.
And yes, AI helps. But algorithms don’t care about context. A ‘rash’ in Nairobi might mean dengue. A ‘rash’ in Chicago might mean a new drug interaction. Without local knowledge feeding into global systems, we’re just training machines to miss the truth.
Money? Yes, we need it. But we also need humility. The best pharmacovigilance isn’t happening in Zurich or Boston. It’s happening in a clinic in Lagos where a nurse writes down symptoms on a napkin because the tablet is out of battery. That’s the data we’re missing. That’s the story we’re ignoring.
Harmonization isn’t a policy goal. It’s a moral one. If a drug kills someone in Indonesia, and we don’t know until a year later because their report was stuck on paper - we failed. Not the patient. Not the company. Us. All of us who had the power to change it.
Let’s stop calling it ‘efficiency.’ Let’s call it justice.
JD Mette
Interesting read. I wonder how many of these reports in VigiBase are duplicates because of inconsistent coding. I’ve seen cases where ‘dizziness’ and ‘lightheadedness’ are treated as separate events even though they’re clinically the same.
Karla Morales
Let’s not romanticize this. The ‘global system’ is a fantasy. The WHO can’t even enforce basic reporting in 70% of member states. This is all performative altruism. Companies pay lip service to harmonization while lobbying to keep their own loopholes. And don’t get me started on AI - it’s just black-box bias wrapped in a lab coat. 🤖
Laurie Sala
Ugh. Another ‘progress is happening’ article. When will we stop pretending that $1.8 billion will magically fix everything? The real problem is that pharma companies don’t want transparency - they want liability shields. They’d rather pay fines than fix the system. And regulators? They’re too scared to hold them accountable.
Charmaine Barcelon
Patients should just stop taking generics. Seriously. If you can’t trust the drug, why risk it? The system is broken. End of story.