When the FDA shows up at your generic drug manufacturing facility, it’s not a surprise visit-it’s a routine check. But that doesn’t mean you can wing it. The agency doesn’t just look at paperwork. They watch how your team handles materials, how your equipment runs, and whether your quality control unit actually has the authority to stop a batch when something’s off. If you’ve never been inspected before, here’s what really happens-and how to get ready.
Why the FDA Inspects Generic Drug Facilities
The FDA doesn’t inspect generic drug plants because they don’t trust manufacturers. They inspect because the law says they must. Every facility making drugs for the U.S. market must follow Current Good Manufacturing Practices (CGMP), outlined in 21 CFR Part 211. These rules aren’t suggestions. They’re the minimum standard for ensuring every pill, injection, or capsule is safe, effective, and consistent.
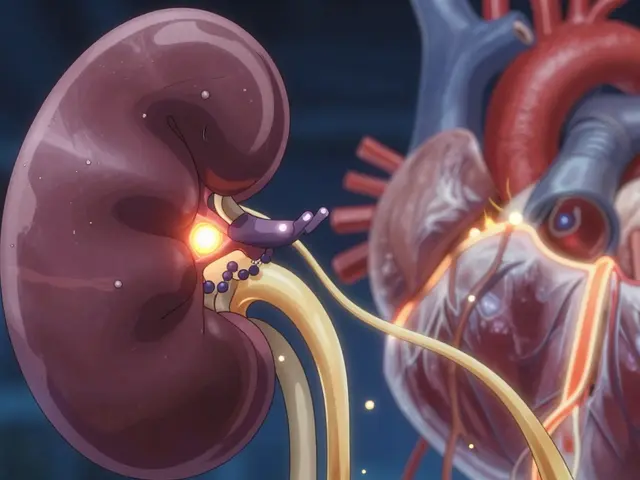
Generic drugs make up over 90% of prescriptions filled in the U.S. That’s billions of doses every year. If one batch is contaminated or under-dosed, the impact isn’t just financial-it’s personal. That’s why the FDA uses a risk-based model to pick which facilities get inspected and when. Sites with past issues, high-risk products, or sudden spikes in patient complaints get priority. But even the cleanest plants aren’t off the hook. Routine inspections happen every two years on average, and some get hit more often.
The Six Systems the FDA Checks
FDA investigators don’t wander around randomly. They follow a structured approach called the 6-System Inspection Model. Every inspection covers the Quality System, and then picks two or more of these five others:
- Quality System - This is always checked. They look at your quality unit’s independence, SOPs, deviation investigations, and CAPA processes. Are you fixing problems-or just documenting them?
- Facilities & Equipment - Are your cleanrooms properly maintained? Is equipment calibrated? Are cleaning procedures validated? They’ll check logs, maintenance records, and even the condition of your HVAC filters.
- Materials - Where do your raw ingredients come from? Do you test every batch? Do you have qualified suppliers? They’ll pull your vendor approval records and look for gaps in supplier audits.
- Production - Can you prove your process is consistent? They’ll review batch records, process validation data, and equipment logs. Did you follow the approved procedure exactly? If not, why?
- Packaging & Labeling - Mislabeling is a top cause of recalls. They’ll check if your labels match the approved template, if barcode scanning works, and if anti-tampering features are in place.
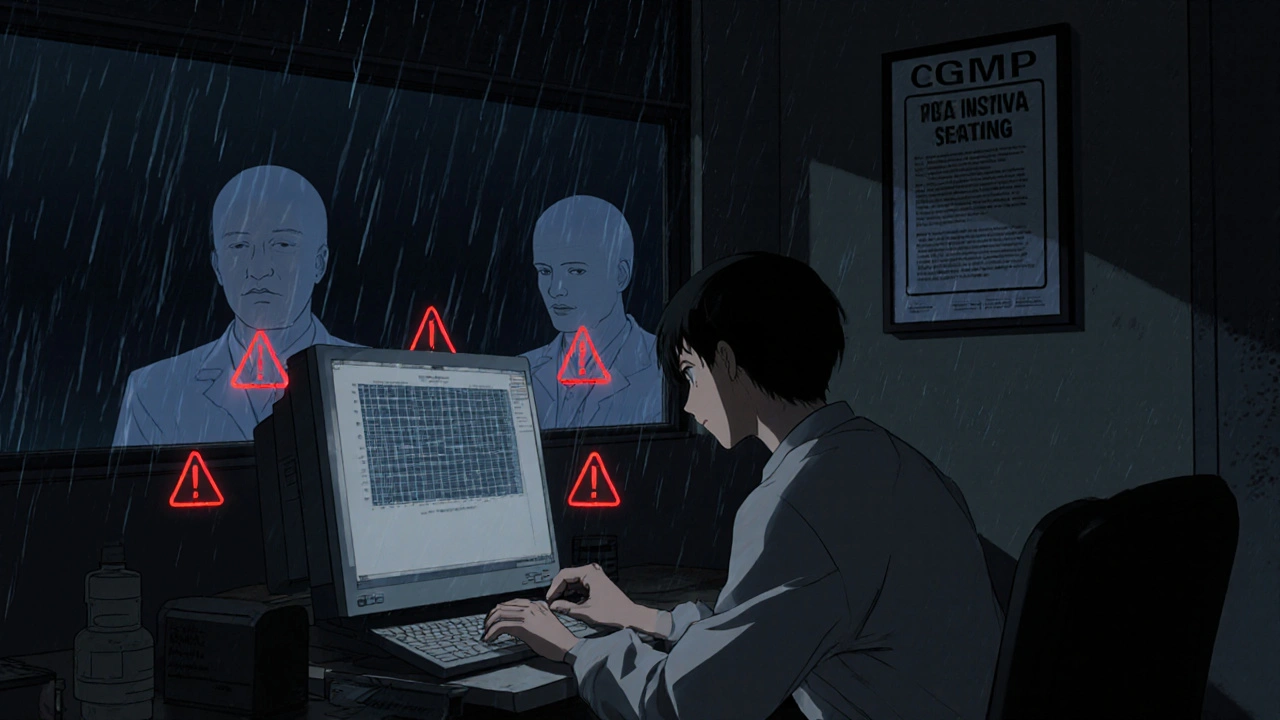
- Laboratory Control - Your lab isn’t just a room with machines. They’ll verify your analytical methods are validated, your reference standards are traceable, and your data is intact. No backdating. No deleting. No cherry-picking results.
One key thing: the Quality System is the backbone. If your quality unit can’t say no to production, the inspection will fail-no matter how good your equipment looks.
What Happens During a Pre-Approval Inspection (PAI)
If you’re submitting a new generic drug application, expect a Pre-Approval Inspection. This isn’t just a tour. It’s a deep dive into whether your facility can actually make the drug you described in your application.
The FDA team will check three things:
- Is your facility ready for commercial production?
- Do your records match what you submitted?
- Is your application complete and accurate?
They’ll compare your facility layout to your drawings. They’ll check if the analytical methods you filed are the same ones used in your lab. They’ll look at your stability samples-where are they stored? Are the temperatures logged? Are the samples still in their original containers?
One common mistake: companies submit detailed applications but don’t train staff to follow them. Investigators will ask a line operator, "What’s your SOP for cleaning this mixer?" If the answer doesn’t match the document, that’s a red flag.
What You’ll Get: FDA Form 483 and the Establishment Inspection Report
At the end of the inspection, the FDA team will hand you a Form FDA 483. This isn’t a final verdict-it’s a list of observations. Each item references a specific regulation, like 21 CFR 211.22(a) for lack of quality unit authority or 21 CFR 211.160(b) for unvalidated test methods.
Observations are listed in order of severity. A single missing calibration log might be a minor observation. But if your quality unit can’t stop production, that’s a major one.
You have 15 business days to respond. Don’t just say "we’ll fix it." Explain exactly what you did, when, and how you prevented it from happening again. Attach evidence: revised SOPs, training records, validation reports.
The FDA then writes the Establishment Inspection Report (EIR), which becomes part of your facility’s permanent record. This report determines whether your inspection is marked as "acceptable" or "unacceptable." If it’s unacceptable, you could get a warning letter-or worse, an import alert blocking your drugs from entering the U.S.
How to Prepare-Without Panicking
You don’t need to stage a fake inspection. You need to run your facility like one’s already happening.
- Keep everything documented - If it’s not written down, it didn’t happen. That includes deviations, investigations, training, and equipment maintenance.
- Train your team - Everyone, from the janitor to the plant manager, should know who to call when an FDA investigator shows up. No one should guess what to say.
- Do mock inspections - Bring in a third party to simulate an audit. Watch how your staff reacts. Do they know where the batch records are? Can they explain their process in under a minute?
- Fix small issues early - A broken thermometer in a cold room? Fix it. A missing signature on a log? Correct it. The FDA sees patterns. One small gap can look like a culture problem.
- Don’t wait for the notice - The FDA can show up unannounced. Treat every day like inspection day.
Facilities with mature quality systems-those that go beyond compliance and build a real quality culture-get better outcomes. Investigators notice when teams are confident, calm, and know their processes inside out.
The New PreCheck Program: Get Feedback Before You Build
In 2024, the FDA launched the PreCheck program to help manufacturers avoid costly mistakes. If you’re designing a new facility or upgrading equipment, you can submit a Type V Drug Master File (DMF) early. This includes your facility layout, quality system design, and validation plans.
The FDA reviews it and gives you feedback before you spend millions on construction. It’s not a guarantee of approval-but it’s the closest thing you’ll get. Companies using PreCheck report fewer major findings during their actual inspections.
This program is part of a bigger push to bring generic drug manufacturing back to the U.S. The FDA isn’t just cracking down-they’re trying to help you get it right.
What Happens After a Warning Letter
If you get a warning letter, it’s not the end. But it’s serious. The FDA will review your response, consult internal experts, and decide whether to close the case or take further action.
In June 2025, the FDA finalized guidance for Post-Warning Letter Meetings (PWLMs). This gives you a chance to sit down with agency officials, explain your corrective actions, and ask questions. It’s not a negotiation. But it’s a path forward.
Follow-up inspections are common. The FDA will come back to see if you fixed what you promised. If you didn’t, you risk import bans or criminal charges.
High Compliance Rates-But Don’t Get Complacent
The FDA reports that over 90% of inspections find facilities to have acceptable CGMP compliance. That’s good news. But it doesn’t mean you’re safe.
Those 10% that fail? They’re often the ones who thought they were "close enough." They skipped training. They didn’t validate a method. They assumed the auditor wouldn’t notice.
The FDA isn’t looking for perfection. They’re looking for control. Can you prove you know what you’re doing? Can you show you’re consistently doing it right? If yes, you’ll pass.
If you’re building a new facility, upgrading an old one, or preparing for your first inspection-don’t wait. Start now. Document everything. Train your team. Fix the small stuff. And remember: the goal isn’t to pass an inspection. It’s to make medicine people can trust.
What happens if I don’t respond to an FDA 483 within 15 days?
If you don’t respond, the FDA will assume you’re not addressing the findings. This increases the chance of a warning letter, import alerts, or even product seizures. The FDA expects a timely, detailed, and evidence-based response-even if you disagree with an observation. Silence is treated as non-compliance.
Can the FDA inspect without warning?
Yes. Routine inspections can be unannounced, especially for facilities with higher risk profiles or past compliance issues. The FDA does not need to notify you in advance. This is standard practice under CGMP regulations to ensure you’re operating in a state of control at all times.
What’s the difference between a 483 and a warning letter?
An FDA 483 lists observations from the inspection-it’s an initial list of concerns. A warning letter is a formal regulatory action issued if the FDA believes your responses are inadequate or if the findings indicate serious violations. Warning letters are public, can trigger legal consequences, and often lead to import bans.
Do I need to validate every analytical method?
Yes. Every test used to release a batch or verify stability must be validated. The FDA checks for parameters like accuracy, precision, specificity, and robustness. If you’re using a method from a pharmacopeia like USP, you still need to prove it works in your lab under your conditions.
What’s the biggest mistake companies make during FDA inspections?
The biggest mistake is assuming compliance is about paperwork. The FDA looks for evidence of a real quality culture. If your quality unit is silent when production pushes to ship a questionable batch, or if employees can’t explain why they follow a procedure, you’ll fail-even with perfect documents. It’s about behavior, not just records.
Is the FDA focusing more on data integrity now?
Absolutely. Investigators are trained to spot signs of data manipulation: backdated entries, deleted files, unexplained changes in chromatograms, or inconsistent timestamps. Electronic records must be secure, auditable, and backed up. If your system allows users to delete data without a trace, you’re at high risk for a major finding.
Can I use the same SOPs for multiple products?
Only if the processes are truly identical. The FDA requires product-specific validation and documentation. Using a generic SOP for different drugs without proving each one meets its unique requirements is a common violation. Each product’s formulation, equipment, and controls must be individually validated and documented.


Comments (15)
Aarti Ray
Coming from India where we make a lot of generic meds, I can say the FDA rules are tough but fair. We train our staff like they’re surgeons-because in a way, they are. One typo in a batch log and the whole shipment gets held. No drama, just discipline.
Skye Hamilton
So the FDA’s just gonna show up unannounced like some kinda federal ghost? 😒 Like we’re all criminals until proven innocent? Who gave them the right to invade our factories like this?
Maria Romina Aguilar
...I mean, technically, under 21 CFR 211.22(a), the quality unit must have authority... but what if they don’t? What if the plant manager is also the head of QA? Is that really a violation? Or just... a corporate structure?
Brandon Trevino
Let’s be clear: 90% compliance rate is a lie. The FDA doesn’t inspect the real offenders-they inspect the ones who still have paper records. The ones using LIMS systems? They’re invisible. This whole system is a charade.
Denise Wiley
OMG I just had a panic attack reading this. I work in a small lab and we’ve got one person doing QA, production, AND cleaning logs. I didn’t even know we were supposed to validate every method. I thought USP was enough. I’m so sorry everyone.
Austin Simko
They’re using inspections to control the drug supply chain. You think this is about safety? It’s about keeping foreign generics out. The FDA’s a tool of Big Pharma.
Nicola Mari
It is beyond appalling that any facility would dare assume that ‘close enough’ is acceptable when human lives are at stake. The arrogance of modern industry is staggering. No training? No validation? Shameful. Utterly shameful.
Sam txf
You people are acting like the FDA is some kind of benevolent angel. They’re bureaucrats with clipboards. They don’t care if your drug saves lives-they care if your logbook has a signature in the right box. This isn’t medicine. It’s paperwork theater.
Michael Segbawu
Why do we let foreigners make our meds? We used to make everything here. Now we’re begging the FDA to check on Chinese plants. This ain’t freedom. This is surrender.
Alexander Rolsen
...I’ve seen it. The lab techs? They’re terrified. They know if they say the wrong thing, they’ll get fired. The QA guy? He’s got a notebook full of fake CAPAs. The FDA doesn’t know. But I do. And I’m not sleeping tonight.
Leah Doyle
Thank you for writing this. I’m a new QA intern and I was so scared to ask questions. Now I feel like I actually understand what’s at stake. 🙏
Alexis Mendoza
What if the real problem isn’t the inspection? What if it’s that we’ve turned medicine into a checklist? We’re not building trust-we’re building compliance. And trust can’t be documented.
Michelle N Allen
Okay so I read all this and I’m just wondering-do we really need to validate every single method? Like, isn’t that just a waste of time? I mean, if it’s in USP and it’s worked for 20 years, why do we need to reprove it? It’s not like anyone’s going to notice unless they’re looking for something to fail. And honestly, who has the time?
Olivia Gracelynn Starsmith
One thing I’ve learned over 18 years in pharma: the best inspections aren’t the ones where you pass. They’re the ones where you walk away and realize you’ve actually improved your system. The FDA doesn’t want to shut you down. They want you to stop cutting corners. And if you’ve been doing that? Good. You’re already ahead of most.
Madison Malone
I used to think inspections were scary. Now I see them as a gift. Every time they come, they show us what we’re missing. We fixed a broken thermometer last month because of an inspection tip. That’s not a penalty-that’s a lifesaver.