
When you're on TRICARE, getting your prescription filled shouldn't feel like a maze. For most military families, generics are the go-to choice-cheaper, just as effective, and widely covered. But knowing exactly what’s covered, where to fill it, and how much you’ll pay can make all the difference. With changes taking effect in January 2026, it’s time to get clear on how TRICARE handles generic medications.
How TRICARE Defines and Covers Generics
TRICARE doesn’t just cover any generic drug. It only covers generics that are on its official formulary-a list updated every month by the Defense Health Agency. These aren’t just any copycat pills. They’re FDA-approved versions of brand-name drugs with the same active ingredients, strength, and dosage. The key difference? Price. Generic drugs typically cost 80-85% less than their brand-name counterparts. That’s why TRICARE pushes them hard: 92% of all prescriptions filled through the program in 2025 were for generics. But here’s the catch: not every generic is automatically covered. Some generics-even if FDA-approved-aren’t on the formulary. That means your doctor might prescribe a generic, but TRICARE won’t pay for it unless you get prior authorization. About 12% of generic drugs require this extra step. If your drug isn’t on the formulary, your provider has to prove it’s medically necessary. Approval rates are around 78%, but that still means you might wait days or even weeks.Where to Get Your Generics and What It Costs
TRICARE gives you three ways to fill prescriptions: military pharmacies, TRICARE Home Delivery, and retail network pharmacies. Each has different costs-and one is completely free. Military pharmacies are the best deal. If you’re eligible and your local base has a pharmacy, you pay $0 for every covered generic, no matter what. No copay. No deductible. Just walk in, show your ID, and walk out with your meds. This option is only available to active duty service members, retirees, and their families. It’s the one place where TRICARE’s coverage truly shines. TRICARE Home Delivery is ideal for chronic conditions like high blood pressure, diabetes, or cholesterol. You can order up to a 90-day supply through Express Scripts. As of January 1, 2026, the copay for generic formulary drugs is $14. That’s up from $13 in 2025. Still, it’s far cheaper than most civilian plans. For example, a 90-day supply of lisinopril might cost $14 through TRICARE, while a civilian plan charges $30 for just 30 days. Network retail pharmacies (like CVS, Walgreens, or Walmart) charge $16 for a 30-day supply of a generic formulary drug. This rate hasn’t changed since 2025. But if you use a non-network pharmacy, the cost jumps. TRICARE Prime beneficiaries pay 50% of the total cost after their deductible. Everyone else pays either $48 or 20% of the total-whichever is higher. That’s a big jump, so stick to network pharmacies if you can.What’s Not Covered (And Why)
TRICARE excludes certain drugs, even if they’re generic. The biggest change in 2025 was the removal of weight loss medications from coverage for TRICARE For Life beneficiaries, effective August 31, 2025. This affects about 1.2 million retirees and their spouses. Even though the FDA approved these drugs, TRICARE decided they weren’t medically necessary under its guidelines. Critics say this creates a gap, especially for older adults managing obesity-related conditions. The Defense Health Agency says it’s a cost-control measure, but many beneficiaries are frustrated. Another limitation: generic biologics. These are complex, newer versions of biologic drugs (like insulin or rheumatoid arthritis treatments). TRICARE treats them differently. They require 22% more prior authorizations than regular small-molecule generics. That’s because interchangeability rules are stricter. Even if a generic biologic is FDA-approved, TRICARE may still treat it like a brand-name drug until more data proves it’s equivalent.How to Check If Your Drug Is Covered
You can’t guess. You have to check. The TRICARE Formulary Search tool (on esrx.com/tform) is your best friend. Type in the exact drug name and strength. The tool tells you:- Is it on the formulary?
- What tier is it? (Tier 1 = generic)
- What’s the copay?
- Does it need prior authorization?
What to Do If Your Generic Isn’t Covered
If your drug isn’t on the formulary, don’t panic. Your provider can submit a prior authorization request. This usually takes 48 hours. Sometimes, they’ll ask for extra medical records. If it’s denied, you can appeal. About 23% of requests need additional documentation, so make sure your doctor includes clinical notes explaining why the generic isn’t working or why the brand is necessary. You can also ask your provider to switch to a different generic on the formulary. Often, there are multiple versions of the same drug. One might be covered, another isn’t. For example, if your lisinopril isn’t covered, your doctor might switch you to a different manufacturer’s version that is.How TRICARE Compares to Other Plans
Compared to Medicare Part D, TRICARE’s generic copays are higher. Medicare averages $7-$10 for a 30-day supply. TRICARE charges $14-$16. But TRICARE has a secret weapon: free military pharmacies. Medicare doesn’t offer that. VA benefits are even better-zero copays for all medications-but only veterans who are service-connected or low-income qualify. TRICARE covers a much broader group: active duty, retirees, and families. Commercial insurers often have wider formularies, covering 98% of prescribed drugs upfront. TRICARE covers about 90%. But TRICARE wins on consistency. There’s no surprise out-of-pocket spike. No annual deductible for military pharmacies. No complex tier structures that change every year.Real Stories From TRICARE Users
A Marine Corps retiree in Florida says: “My generic cholesterol med costs $14 for 90 days through Home Delivery. My neighbor on a private plan pays $30 for 30 days. I’m saving $100 a month.” On Reddit, a Navy spouse wrote: “Got my blood pressure meds filled at the base pharmacy-$0. I didn’t even know I could do that until last year. Now I won’t go anywhere else.” But not everyone is happy. One Air Force veteran on Military OneSource said: “My doctor prescribed a generic for my thyroid. It wasn’t on the formulary. I had to wait three days for approval. I missed a week of meds.”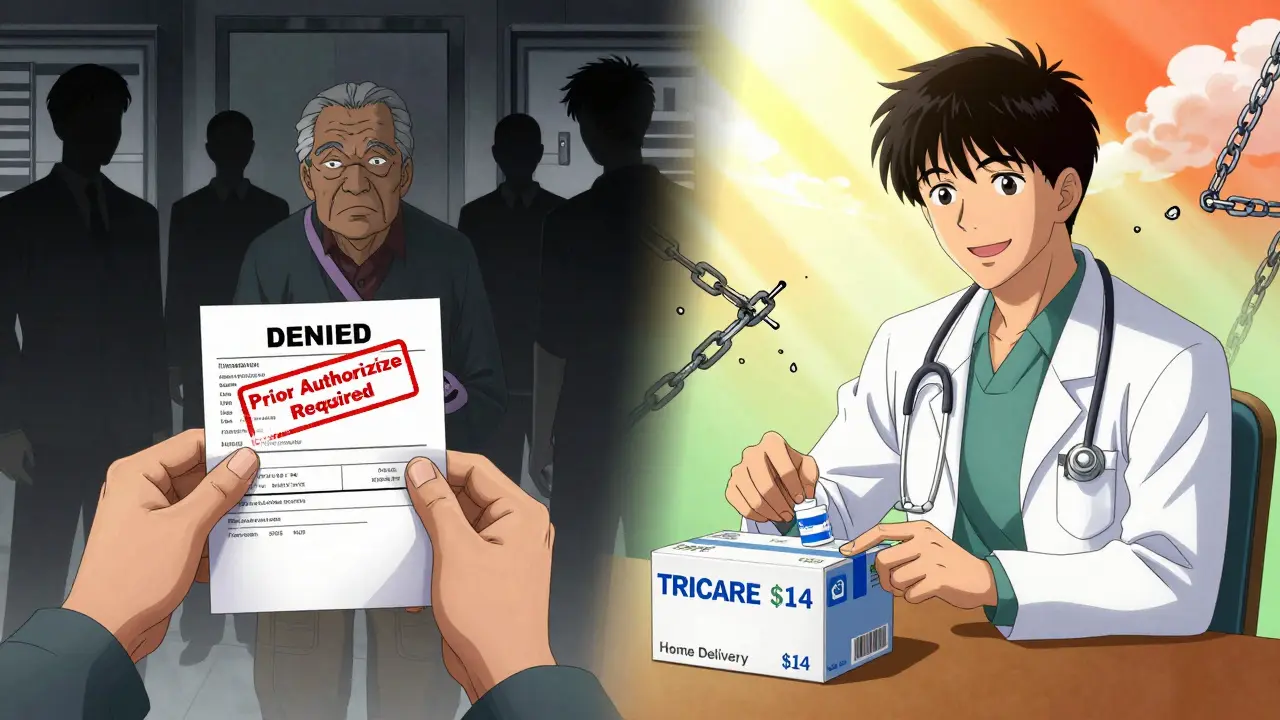
What’s Changing in 2026
The biggest update is the $1 increase for Home Delivery generics-from $13 to $14. That’s the first change since 2023. Retail copays stay at $16. No other changes are planned for 2026. Looking ahead, TRICARE plans to roll out real-time benefit tools by Q3 2026. That means your doctor will see your copay and coverage status before they even write the prescription. No more surprises at the pharmacy. Also coming: step therapy expansion. For 15 more drug classes (like asthma and depression meds), you’ll have to try a cheaper, formulary drug first before moving to a more expensive one. This isn’t new, but it’s spreading.Pro Tips for Managing Your TRICARE Generics
- Always use military pharmacies when possible-$0 copay beats $16 every time.
- Switch to Home Delivery for chronic meds. Save money, save trips.
- Check the formulary before each refill. Drugs get added and removed.
- If a generic isn’t covered, ask your doctor for a substitute on the formulary.
- Call the TRICARE Pharmacy Helpline at 1-877-363-1303 if you’re confused. They handled 1.2 million calls in 2025.
- Don’t use non-network pharmacies unless it’s an emergency. The cost is steep.
TRICARE’s generic drug program isn’t perfect. But it’s one of the most cost-effective systems in the country. For military families, it means fewer financial surprises and more access to essential meds. The key is knowing the rules-and using the tools that make them easy to follow.
Are all generic drugs covered by TRICARE?
No. Only generics on the TRICARE Formulary are covered. About 12% of generic drugs require prior authorization, even if they’re FDA-approved. Always check the TRICARE Formulary Search tool before filling a prescription.
What’s the copay for generic drugs at military pharmacies?
$0. All covered generic and brand-name drugs are free at military pharmacies for eligible beneficiaries, including active duty members, retirees, and their families.
Can I use a non-network pharmacy for TRICARE generics?
Yes, but it’s expensive. TRICARE Prime beneficiaries pay 50% of the total cost after their deductible. Other beneficiaries pay either $48 or 20% of the total cost-whichever is greater. Stick to network pharmacies to avoid high out-of-pocket costs.
Why was my generic drug denied by TRICARE?
Your drug may not be on the TRICARE Formulary, or it may require prior authorization. Some generics, especially for weight loss or biologics, are excluded or restricted. Check the formulary tool or call the TRICARE Pharmacy Helpline at 1-877-363-1303 for details.
Does TRICARE cover weight loss generics in 2026?
No. As of August 31, 2025, TRICARE For Life beneficiaries no longer have coverage for weight loss medications, even if they’re generic. This exclusion remains in place for 2026. Active duty members and other beneficiaries may still be eligible under different rules.


Comments (2)
Harry Henderson
TRICARE’s generic drug game is straight fire. $0 at military pharmacies? That’s not a benefit, that’s a goddamn gift. If you’re still paying $16 at CVS, you’re leaving money on the table. Stop being lazy. Walk. Drive. Do whatever it takes. Your wallet will thank you. And if your doctor tries to push a non-formulary generic? Tell them to file the PA or switch it. No excuses.
suhail ahmed
Man, this post reads like a love letter to bureaucracy wrapped in a pharmacy receipt. But hey-I’m from India, and we’ve got our own chaos with generic meds. Here, you get the same pill in five different brands, each with a different color and price, and none of them are on any ‘formulary’ because there isn’t one. TRICARE’s system? At least it’s predictable. $14 for 90 days? That’s a luxury we’d kill for. Keep pushing the formulary tool. It’s your lifeline.