
SSRI Dosing Calculator
Your Metabolizer Status
Dosing Recommendations
Select your metabolizer types and medication to see dose recommendations.
What This Means
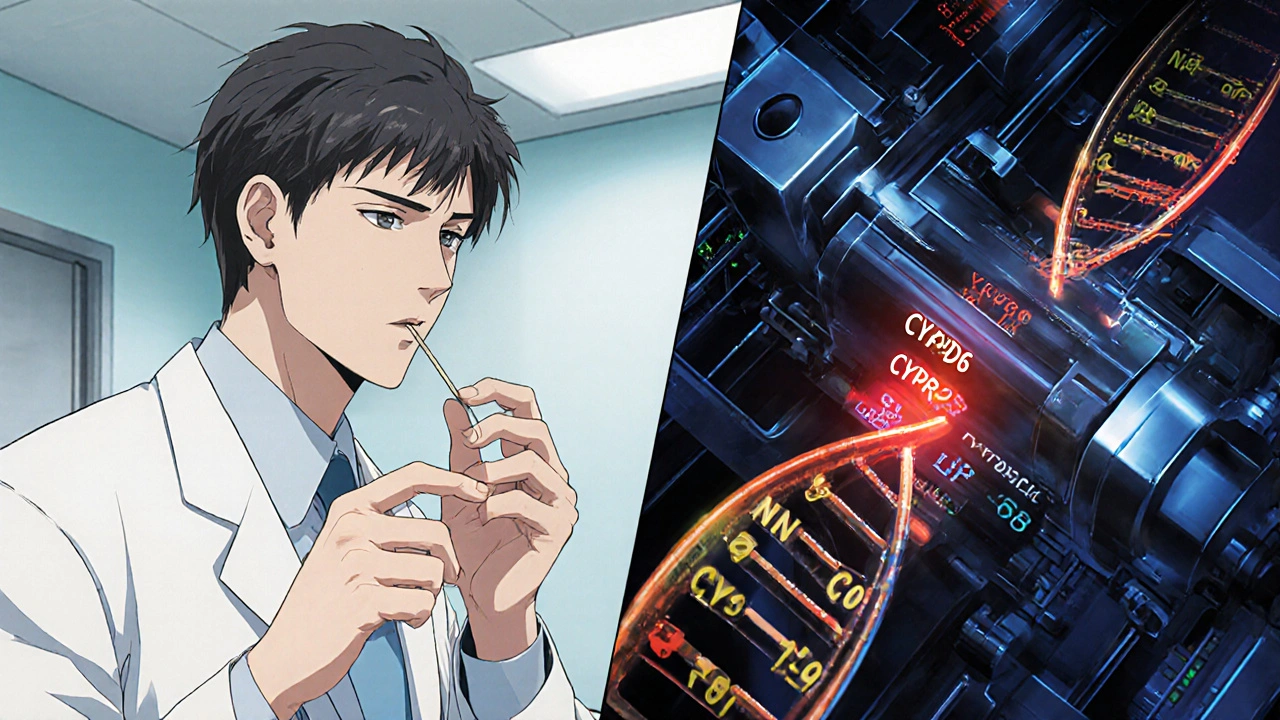
Your genetic makeup influences how your body processes antidepressants. The CYP2C19 and CYP2D6 enzymes determine whether you process SSRIs too slowly or too quickly, affecting both effectiveness and side effects.
Poor Metabolizer
Your body breaks down drugs slowly. May need lower doses to avoid side effects.
Ultrarapid Metabolizer
Your body breaks down drugs quickly. May need higher doses for effectiveness.
Normal Metabolizer
Standard dosing typically works well for most people.
When you start an SSRI like sertraline or escitalopram, you don’t know if it’ll work-or if it’ll make you feel worse before it helps. For many, the first weeks are a gamble: nausea, dizziness, insomnia, or worse. But what if your genes could tell you ahead of time whether your body will struggle with the drug? That’s where CYP2C19 and CYP2D6 come in. These two enzymes, coded by your genes, determine how fast or slow your body breaks down antidepressants. And that speed directly affects whether you get relief-or side effects.
What CYP2C19 and CYP2D6 Do to SSRIs
CYP2C19 and CYP2D6 are liver enzymes that act like molecular scissors, cutting antidepressants into pieces your body can get rid of. But not everyone has the same scissors. Your genes decide if you have sharp ones, dull ones, or even too many of them.
CYP2C19 handles citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft). If you’re a poor metabolizer of CYP2C19, your body can’t break these drugs down fast enough. That means the drug builds up in your blood-sometimes two to three times higher than normal. In one study, poor metabolizers had 3.5 times more escitalopram in their system than normal metabolizers. That’s not just a small difference-it’s enough to trigger dizziness, vomiting, or even heart rhythm changes at standard doses.
CYP2D6 does the same for fluoxetine (Prozac), paroxetine (Paxil), and venlafaxine (Effexor). If you’re a poor metabolizer here, you’re at 2.7 times higher risk of side effects like severe nausea or insomnia. On the flip side, if you’re an ultrarapid metabolizer, your body clears the drug too fast. You might take the full dose and feel nothing. That’s why some people say SSRIs “don’t work” for them-they’re not broken. Their genes are just too efficient.
How Testing Works-and What It Can’t Do
Testing for these genes is simple: a cheek swab or blood sample goes to a lab. Results come back in 1-3 weeks. The test looks at specific gene variants-over 100 for CYP2D6, about 35 for CYP2C19-to assign you one of four metabolizer types: poor, intermediate, normal, or ultrarapid.
But here’s the catch: knowing your metabolizer status doesn’t guarantee you’ll respond better to an SSRI. Studies show clear differences in drug levels, but not always in how people feel. A 2024 study of over 5,800 people found no strong link between CYP2C19 genes and whether someone improved on escitalopram-even though their blood levels were wildly different.
So testing isn’t a crystal ball. It’s a warning system. It tells you: “Your body might not handle this dose safely.” It doesn’t say: “This drug will make you happy.” That still depends on your brain chemistry, stress levels, sleep, and other factors.
Real Cases: When Genes Changed Treatment
One 45-year-old woman started venlafaxine at 75 mg a day. Within days, she couldn’t sleep, felt nauseous, and got dizzy walking to the bathroom. Her doctor assumed it was “normal” side effects. But after pharmacogenetic testing, she was flagged as a CYP2D6 poor metabolizer. Her dose was cut in half-to 37.5 mg-and within a week, her symptoms vanished. She stayed on that lower dose and finally felt better.
Another patient, a CYP2C19 ultrarapid metabolizer, tried escitalopram at 20 mg daily for six weeks with no improvement. His doctor didn’t increase the dose, fearing side effects. But after his test came back, they doubled the dose to 40 mg. Within three weeks, his depression lifted. He didn’t need to try three other meds. He just needed the right dose.
These aren’t rare. In a 2023 study, CYP2D6 poor metabolizers were 3.2 times more likely to report “severe” side effects with paroxetine. CYP2C19 poor metabolizers had 2.8 times more side effects with citalopram. That’s not luck. That’s biology.
Why It’s Not Routine Yet
If the science is this clear, why aren’t all doctors ordering these tests?
First, insurance. As of mid-2024, only 62% of U.S. insurers cover pharmacogenetic testing for antidepressants. Many still see it as “experimental.”
Second, complexity. If you’re a poor metabolizer for CYP2D6 but a rapid one for CYP2C19, which drug do you pick? There’s no simple answer. That’s why the Clinical Pharmacogenetics Implementation Consortium (CPIC) released detailed guidelines in April 2023. But most doctors haven’t had the training to use them.
Third, evidence gaps. CPIC gives CYP2D6 and tricyclic antidepressants (like amitriptyline) a high-level “A” recommendation-strong proof. But for SSRIs, it’s only “B”-meaning the data is good, but not yet definitive. That makes some clinicians hesitant.
Who Benefits Most?
You’re more likely to gain from testing if:
- You’ve tried two or more SSRIs and had bad side effects
- You’ve had antidepressants fail despite taking them correctly
- You’re sensitive to medications in general
- You’re taking more than one drug that’s processed by CYP2D6 or CYP2C19
It’s less helpful if you’ve never tried an SSRI and are just starting out. But if you’ve been stuck in a cycle of side effects and failed treatments, this test can break the pattern.

What Comes Next
The future isn’t just CYP2C19 and CYP2D6. New guidelines now include genes like SLC6A4 (the serotonin transporter) and HTR2A (a serotonin receptor). These help explain why some people respond emotionally to SSRIs-even when their metabolism is normal.
A major NIH-funded trial called GUIDED-2, launched in January 2024, is tracking 5,000 people with treatment-resistant depression across 75 clinics. It’s the largest real-world test of pharmacogenomics for depression ever done. Results are due in 2027.
Meanwhile, polygenic scores-combining dozens of genetic markers with lifestyle data-are being tested in academic centers. By 2026, you might get a single report that says: “Your genes + your sleep patterns + your stress levels suggest sertraline at 100 mg is your best option.”
What to Do Today
If you’re considering testing:
- Ask your doctor if they use CPIC guidelines. If not, ask for a referral to a psychiatrist or pharmacist trained in pharmacogenomics.
- Check with your insurer. Some require pre-authorization.
- Use free tools like the CPIC dosing calculator to understand your results before your appointment.
- Don’t change your dose based on a test alone. Always work with a provider who understands the context.
There’s no magic pill. But there’s now a way to stop guessing. If your body keeps reacting badly to antidepressants, your genes might be trying to tell you something. Listen.
Is pharmacogenomic testing for SSRIs covered by insurance?
As of mid-2024, only about 62% of major U.S. insurers cover CYP2C19 and CYP2D6 testing for antidepressants. Coverage varies by plan and state. Some require prior authorization or proof that you’ve tried at least two antidepressants without success. Medicare and Medicaid coverage is limited and inconsistent. Always check with your insurer before ordering the test.
Can I get tested without a doctor’s order?
Some direct-to-consumer companies offer pharmacogenetic tests, but they’re not always clinically validated. Many don’t test the full range of CYP2D6 variants, especially structural changes like gene duplications. Results from these tests can be misleading. For accurate, clinically actionable results, you need a test ordered by a licensed provider and processed by a CLIA-certified lab.
Does testing work for all SSRIs?
No. CYP2C19 affects citalopram, escitalopram, and sertraline. CYP2D6 affects fluoxetine, paroxetine, and venlafaxine. But fluvoxamine and bupropion are processed differently and aren’t strongly tied to these genes. Not all antidepressants have clear genetic links. Testing is most useful for the SSRIs and SNRIs that rely heavily on CYP2C19 and CYP2D6.
How long does it take to get results?
Most labs take 1 to 3 weeks to return results after receiving your sample. Some specialized clinics offer faster turnaround-under 10 days-but they’re less common. Plan your treatment timeline around this delay. Don’t delay starting medication if you’re in crisis. Use the test to guide future adjustments, not your initial choice.
Can I be a poor metabolizer for one gene and ultrarapid for another?
Yes. This is common. Someone might be a CYP2D6 poor metabolizer but a CYP2C19 ultrarapid metabolizer. That means they process some antidepressants too slowly and others too quickly. This complicates drug selection and requires careful balancing. That’s why CPIC and other guidelines now recommend looking at multiple genes together, not in isolation.
Is pharmacogenomic testing the future of depression treatment?
It’s one piece of the future-not the whole picture. Genetics explains about 30-50% of why people respond differently to SSRIs. The rest comes from environment, trauma, sleep, diet, and other genes. But for people stuck in trial-and-error cycles, this test cuts through the guesswork. It won’t cure depression, but it can reduce the suffering caused by the wrong drug or dose. By 2026, it will likely be standard for complex cases.




Comments (15)
Emily Gibson
I wish my doctor had ordered this test when I was on 40mg of sertraline and couldn't sleep for weeks. Turned out I'm a CYP2C19 poor metabolizer. They cut my dose in half and I finally felt like myself again. It's not magic, but it's way better than guessing.
Mirian Ramirez
Okay so I just got my results back and I'm a CYP2D6 poor metabolizer and a CYP2C19 ultrarapid?? Like what even is my body?? I tried fluoxetine, it did nothing, then I tried escitalopram and got nauseous for two weeks, then paroxetine and I felt like I was gonna pass out?? I'm so confused but also kinda relieved?? Like maybe it's not me being broken?? Maybe my liver just hates antidepressants?? I'm gonna print this out and take it to my psych next week, I think they'll finally listen??
Kika Armata
How quaint. You’re all acting like this is some revolutionary breakthrough. The pharmacogenomic field has been saturated with overhyped, underpowered studies since 2015. The CPIC guidelines are barely consensus-level recommendations, and the NIH’s GUIDED-2 trial won’t even publish until 2027. Meanwhile, you’re treating a cheek swab like it’s a divine revelation. Your serotonin transporter polymorphisms don’t care about your trauma history, your sleep hygiene, or your socioeconomic stressors. This isn’t precision medicine-it’s genetic determinism dressed up in white coats. And don’t get me started on the direct-to-consumer companies selling these tests for $299. They’re not even testing the full CYP2D6 gene variants. You’re paying for placebo science.
Herbert Lui
There’s something deeply poetic about this, isn’t there? We’ve spent centuries trying to fix depression with chemicals, then blaming the person when it doesn’t work. And now we learn-it’s not that your soul is broken. It’s that your liver enzymes are just… different. Like your body speaks a language the doctor doesn’t know. I think of that woman on venlafaxine-37.5 mg and suddenly, the world stopped screaming. That’s not pharmacology. That’s translation. We’re learning to listen to the quiet, molecular voices inside us. And maybe-just maybe-that’s the first real step toward healing. Not more pills. More understanding.
Nick Zararis
Just wanted to say: if you’re thinking about testing, DO IT. Seriously. I’m a CYP2D6 intermediate metabolizer with a CYP2C19 normal, and I was on 60mg of sertraline for 8 months and felt nothing. My psychiatrist, who actually knows CPIC guidelines, cut me to 25mg and added a tiny bit of bupropion. Within 10 days, I could get out of bed. Don’t let anyone tell you it’s ‘experimental.’ If you’ve tried three SSRIs and felt like garbage, this is your lifeline. Also, check your insurance-some plans cover it now, even Blue Cross.
Sara Mörtsell
Everyone’s acting like this is a miracle but the data is still B level? And you’re going to change your dose based on a gene test? That’s not science-that’s superstition. I’ve seen people go off their meds because they read a Reddit post. You don’t need a gene test to know if you’re suicidal. You need a therapist. And a bed. And food. And someone who won’t judge you. Stop outsourcing your mental health to a lab report.
Rhonda Gentz
I’ve been on three different SSRIs. Two made me feel like I was drowning. One made me feel nothing. I never thought it was my genes-I thought I was just broken. Then I got tested. CYP2C19 poor metabolizer. My doctor dropped my escitalopram from 20mg to 10mg. I cried the first day I didn’t feel like I was going to vomit. It’s not a cure. But it’s the first time in five years I didn’t feel like I was fighting my own body. I wish I’d known sooner.
Alexa Ara
Hey, if you’re reading this and you’ve been stuck in the SSRI loop-you’re not alone. I was there. I thought I was weak. Turns out my liver just processes meds differently. This test didn’t fix my depression, but it stopped the torture of guessing. And that? That’s huge. You deserve to feel better without suffering through three bad drugs first. Talk to your doctor. Ask for the test. You’ve got nothing to lose but the nausea.
Olan Kinsella
You think this is about genes? Nah. This is about control. The pharmaceutical industry doesn’t want you to know your body can handle less. They want you on 50mg, 100mg, forever. And the labs? They’re making bank off these tests. I got mine done. The results said I’m a poor metabolizer. So I cut my dose in half. And guess what? I didn’t die. I didn’t even feel worse. I just… felt. Like I was human again. Who’s really in charge here? The genes? Or the profit margins?
Kat Sal
OMG I just got my results and I’m a CYP2D6 ultrarapid AND a CYP2C19 poor?? Like… what?? I’ve been on 40mg of escitalopram for a year and felt nothing. My doc said ‘maybe it’s not working.’ But now I know-I just needed 80mg. And I didn’t get sick?? I’m so hyped. I’m gonna tell everyone I know. This is the future!!
Rebecca Breslin
Of course this works. I’ve been saying this for years. My cousin got tested, got her dose adjusted, and now she’s hiking in the Rockies. Meanwhile, my therapist still says ‘just try another one.’ She doesn’t even know what CYP2D6 is. This isn’t just science-it’s justice. People deserve to be treated based on their biology, not their insurance plan. Stop being lazy, doctors.
Kierstead January
Let me guess-you’re white, middle-class, and have good insurance. That’s why you can afford this test. What about the people on Medicaid who can’t even get a therapist? You’re turning depression into a genetic lottery. Meanwhile, people in rural areas are still being told to ‘exercise more’ and ‘drink less coffee.’ This isn’t progress. It’s privilege dressed up as science.
Imogen Levermore
Wait… so you’re telling me your genes are deciding if you’re depressed or not? 😳 What about the NSA? What about the vaccines? Did you know CYP2D6 was used in the 1990s to track Soviet spies? I’m not saying this is fake… but why is the government not talking about this? And why do all the labs use the same company? 🤔 #MindControl #CYP2D6IsALie 🤖💊
Chris Dockter
Stop pretending this is science. The study showed no link between gene status and improvement. Zero. Nada. The only thing that changed was blood levels. So what? You’re still depressed. You’re still suffering. This is just another way for pharma to sell more tests and more pills. Don’t fall for it.
Gordon Oluoch
People are treating this like a cure. It’s not. It’s a tool. A limited, imperfect, expensive tool. And yet you’re all acting like you’ve been handed the keys to heaven. Meanwhile, the real issues-trauma, poverty, isolation-are still ignored. You want to fix depression? Fix the world. Not your liver.