When you fill a prescription for a brand-name drug like Protonix or Yasmin, you might not realize the pill in your hand could be an authorized generic - identical to the brand, but priced like a generic. For insurers, this isn’t just a cost-saving trick; it’s a strategic tool to control spending without risking patient outcomes. But how does formulary placement actually work for these drugs? And why do some patients get hit with surprise denials or confusion at the pharmacy counter?
What Exactly Is an Authorized Generic?
An authorized generic is a brand-name drug sold under a different label - no brand name, no fancy packaging, but the exact same active ingredients, dosage, and manufacturing process. It’s made by the original brand company, using the same factory and formula, just without the brand logo. Think of it like a car manufacturer selling the same model under a different dealership name.
Unlike regular generics, which must prove they’re bioequivalent through an Abbreviated New Drug Application (ANDA), authorized generics skip that step entirely. They’re approved under the original New Drug Application (NDA), meaning they’re legally and chemically identical to the brand. The FDA lists over 147 authorized generics as of 2023, including popular drugs for acid reflux, birth control, and thyroid conditions.
This matters because it eliminates guesswork. If your doctor prescribes Synthroid and you’re allergic to a dye used in the brand version, you won’t get a different generic with a different filler - you’ll get the same pill, just cheaper. That’s why many patients with narrow therapeutic index drugs (like warfarin or levothyroxine) prefer them.
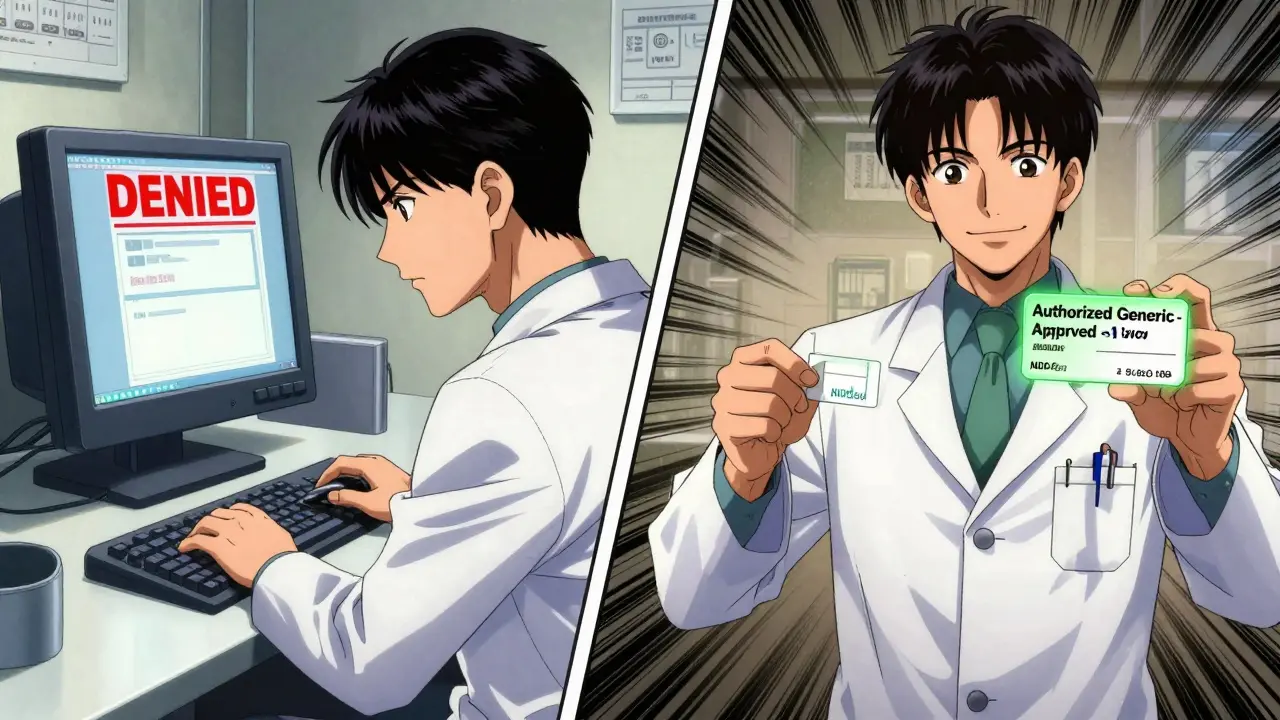
How Insurers Treat Authorized Generics in Formularies
Most insurance plans group drugs into tiers. Tier 1 is cheapest (usually regular generics), Tier 2 is mid-range (sometimes brand-name drugs with higher copays), and Tier 3 or 4 is the most expensive. The big question: Where do authorized generics go?
According to a 2022 Health Affairs study of 1,247 Medicare Part D plans, 87% of insurers place authorized generics in the same tier as traditional generics - usually Tier 1 or Tier 2. That means a $50 brand-name copay drops to $10 or even $0. Only 12% treat them like brand drugs. That’s a huge win for cost control.
Why? Because insurers know there’s zero therapeutic risk. No need for prior authorization. No step therapy. No appeals. If a patient is stable on a brand, switching to its authorized generic doesn’t require a new prescription or monitoring. It’s a seamless swap.
But here’s the catch: Not all plans make this clear. Some formularies don’t even list “authorized generic” as a separate option. They just say “generic.” That’s where confusion starts.
Why Authorized Generics Are Cheaper - But Not Always Available
Authorized generics typically cost 15-25% less than the brand-name version. That’s the same discount you’d expect from a regular generic. But unlike traditional generics, which can take months to enter the market after a patent expires, authorized generics can launch the same day. That’s because the brand company controls the supply - they’re not waiting for another manufacturer to file an ANDA.
That speed gives manufacturers a strategic advantage. Instead of letting a competitor undercut them with a cheaper generic, they release their own version - and keep the market share. In fact, a 2021 Health Affairs study found that in 22% of cases, the introduction of an authorized generic delayed the entry of true generic competitors.
That’s why only about 15-20% of brand-name drugs have an authorized generic version. They’re not common for every medication. You’ll see them most often in high-revenue drugs - cardiovascular, endocrine, and psychiatric meds. Oncology drugs? Rarely. Why? Because manufacturers of cancer drugs often rely on complex pricing models and patient assistance programs. An authorized generic could disrupt that.
Real Patient Experiences: Savings and Surprises
On Reddit’s r/Pharmacy community, users share stories of life-changing savings. One person wrote: “My insurance denied Synthroid because it was branded. But when I asked for the authorized generic, they approved it with a $10 copay. I’ve been on it for six months - no difference in how I feel.”
That’s the ideal scenario. But not everyone gets it right. A 2022 GoodRx survey of 1,500 patients found that 34% didn’t know their pharmacy switched them to an authorized generic. Some saw a different-looking pill and thought it was a mistake. Others got denied coverage because the pharmacy system didn’t recognize the NDC code.
Pharmacies aren’t always set up to handle them. Walgreens reported a 12% error rate in processing authorized generic claims before they updated their systems. Why? Because these drugs aren’t listed in the FDA’s Orange Book - the usual reference for generics. They’re hidden in a separate FDA list. If your pharmacy’s software doesn’t pull from that list, it won’t know the drug is covered.
That’s why some patients get caught in the middle. A prescription for “Lisinopril” might get filled with a regular generic. But if the doctor meant “Lisinopril HCTZ authorized generic,” and the pharmacy didn’t flag it, the claim gets rejected. The patient thinks the drug isn’t covered. The doctor thinks it’s a formulary issue. The insurer thinks the pharmacy messed up.
How PBMs Are Changing the Game
Pharmacy Benefit Managers (PBMs) like OptumRx, Express Scripts, and CVS Caremark are starting to treat authorized generics as a core cost-saving tool. In January 2023, OptumRx rolled out an “Authorized Generic First” policy for 47 high-cost medications. That means if an authorized generic exists, it’s the default option - unless the doctor writes “dispense as written” or the patient objects.
Express Scripts added special flags to their formulary system in late 2022 to identify authorized generics separately from traditional generics. That lets them track usage, measure savings, and push them to the top of the formulary.
And it’s working. A Health Affairs study found that Medicare Part D plans with clear authorized generic policies saved 7.3% per member per month on prescription costs. That’s not small change - it adds up to hundreds of millions across a national plan.
But it’s not just about Medicare. Large employers are catching on. According to the Kaiser Family Foundation’s 2023 Employer Health Benefits Survey, 68% of big companies plan to differentiate coverage between authorized generics and traditional generics in 2024. Some may even offer lower copays for authorized generics - treating them as the preferred option.
What Patients and Providers Need to Know
If you’re on a brand-name drug and your insurance says it’s not covered, ask: “Is there an authorized generic version?” You might be surprised. The FDA keeps a public list of all authorized generics. Your pharmacist can look it up. Your doctor can prescribe it by name.
Don’t assume “generic” means the same thing. A regular generic might have different fillers or coatings. An authorized generic won’t. That’s critical for people with allergies, sensitivities, or those on drugs where tiny differences matter.
For prescribers, write the generic name - not the brand - unless there’s a medical reason not to. If you write “Synthroid,” you might get the brand. If you write “levothyroxine,” you might get a regular generic. But if you write “levothyroxine (authorized generic),” you increase the chance of getting the exact match.
And if your claim gets denied? Call your insurer. Ask them to check if the NDC code for the authorized generic is in their system. Many denials are just system errors - not policy issues.
The Future: More Coverage, More Scrutiny
The Inflation Reduction Act of 2022 is pushing Medicare Part D to favor lower-cost options. CMS expects authorized generic usage to grow 15-20% by 2025. That means more plans will adopt “first choice” policies.
But there’s a shadow. The FTC has flagged authorized generics as a potential anti-competitive tool. If a brand company uses its authorized generic to block cheaper competitors, that could trigger enforcement. That’s why some manufacturers are careful - they launch the authorized generic only after traditional generics are already in the market.
Meanwhile, the FDA’s GDUFA III rules, updated in 2023, are making it easier to track and report authorized generics. That means better transparency - fewer hidden drugs, fewer denied claims.
For now, authorized generics are one of the most underused tools in pharmacy benefits. They offer the best of both worlds: brand reliability at generic prices. But only if you know they exist - and know how to ask for them.
Are authorized generics the same as regular generics?
No. Regular generics are made by different companies and must prove they’re bioequivalent to the brand through FDA testing. Authorized generics are made by the brand company itself, using the exact same formula, ingredients, and manufacturing process. They’re identical to the brand drug - just sold without the brand name.
Why is my insurance denying my authorized generic?
It’s usually a system error. Authorized generics aren’t listed in the FDA Orange Book, so some pharmacy databases don’t recognize them. The NDC code might be missing or mislabeled. Ask your pharmacist to verify the NDC code against the FDA’s authorized generic list. If it’s correct, call your insurer and request a manual override.
Can I request an authorized generic instead of the brand?
Yes. You can ask your doctor to prescribe the generic name and specify “authorized generic” if available. You can also ask your pharmacist if an authorized generic version exists for your brand-name drug. Many pharmacies can check the FDA’s list or use PBM tools like Prime Therapeutics’ AG Tracker to find it.
Do authorized generics cost less than regular generics?
Usually, no - they cost about the same. But they’re significantly cheaper than the brand-name version. The key advantage isn’t always price difference between generics, but that they’re identical to the brand. So if you’re sensitive to inactive ingredients, an authorized generic gives you brand consistency at generic cost.
Why aren’t all brand drugs available as authorized generics?
Manufacturers choose when to launch them. They’re often used for high-revenue drugs where the company wants to retain market share after patent expiration. For drugs with low profit margins, or where generic competition is already strong, there’s little incentive to launch an authorized generic. Only about 15-20% of brand drugs have one.
What to Do Next
If you’re paying a high copay for a brand-name drug, check if an authorized generic exists. Visit the FDA’s website and search their authorized generic list. Talk to your pharmacist. Ask your doctor to switch the prescription. Even a $10 copay difference adds up over time.
For employers and insurers, the data is clear: Clear policies on authorized generics reduce costs without compromising care. Update your formularies. Train your staff. Flag these drugs in your system. You’re not just saving money - you’re reducing patient confusion and improving adherence.
Authorized generics aren’t magic. But they’re one of the quietest, most effective ways to bring down drug costs - if you know how to use them.