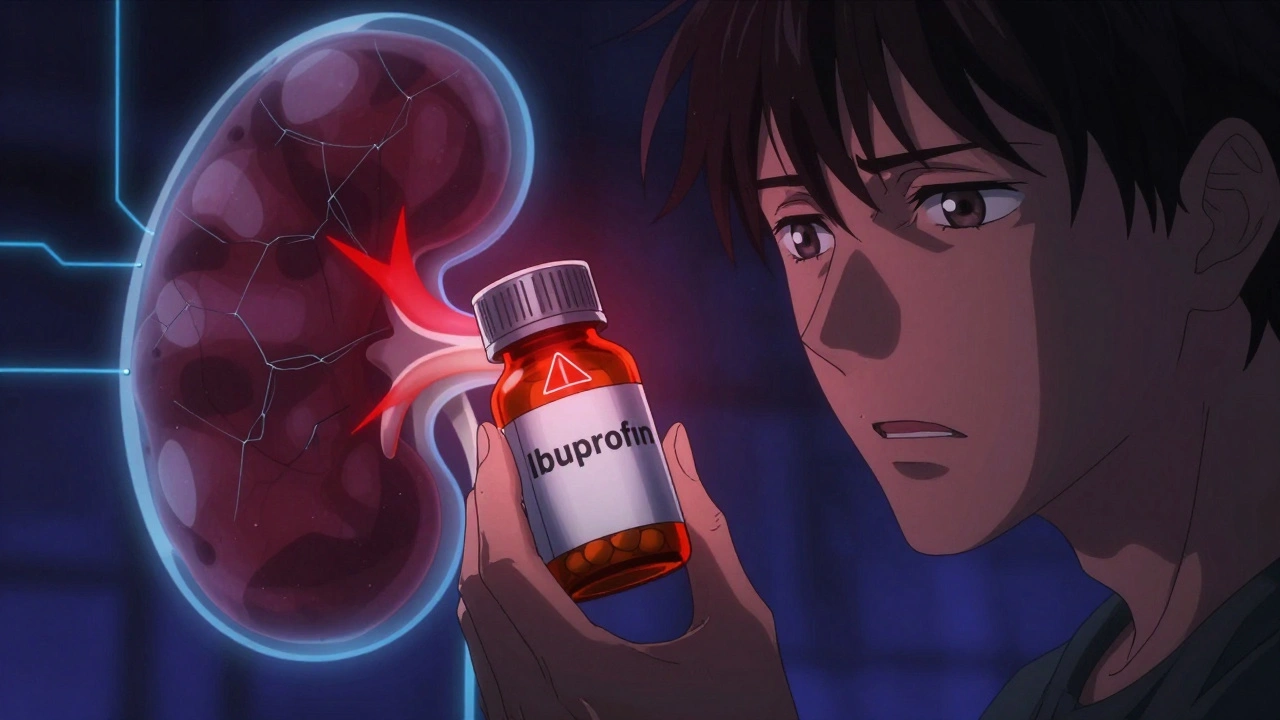
When your kidneys aren’t working well, even common medications can turn dangerous. It’s not just about taking less - it’s about knowing which drugs to avoid entirely, when to change the dose, and how to monitor for hidden risks. For someone with chronic kidney disease (CKD), a simple headache pill like ibuprofen can spike creatinine levels overnight. A diabetes drug that’s safe for most could land them in the hospital with lactic acidosis. This isn’t theoretical. In 2024, a patient in Halifax with stage 4 CKD ended up in emergency after taking two Advil for a cold. Their creatinine jumped from 3.2 to 5.7 in 48 hours. That’s acute kidney injury from a drug they thought was harmless.
Why Kidneys Change How Drugs Work
Your kidneys filter waste, but they also clear most medications from your blood. When kidney function drops - measured by eGFR (estimated glomerular filtration rate) - drugs build up. That’s why a standard dose of antibiotics, painkillers, or diabetes meds can become toxic. The problem isn’t always obvious. Many people don’t realize their kidney function has declined until they get sick from a medication they’ve taken for years.The key number is eGFR. If it’s below 60 mL/min/1.73 m², most drugs need review. Below 30? Many need to be stopped or changed. But here’s the catch: eGFR isn’t static. It can drop fast during illness, dehydration, or after surgery. A dose that was safe last month might be dangerous this week.
Drugs That Can Hurt Your Kidneys (Nephrotoxins)
Some medications are outright risky for people with CKD. These are called nephrotoxins - they directly damage kidney cells. The biggest culprits:- NSAIDs (ibuprofen, naproxen, celecoxib): These reduce blood flow to the kidneys. Even short-term use can trigger acute kidney injury, especially in older adults or those with diabetes. Avoid them completely if your eGFR is below 45.
- Sodium phosphate bowel prep: Used before colonoscopies. Can cause severe, lasting kidney damage. Polyethylene glycol (PEG) is the safe alternative.
- Aminoglycosides (gentamicin, tobramycin): Antibiotics that stick around in the body when kidneys fail. They can cause permanent hearing loss and kidney damage. Dosing must be adjusted by weight and eGFR, often given once daily instead of every 8 hours.
- Contrast dye: Used in CT scans. Can cause contrast-induced nephropathy. Hydration and sometimes a drug called N-acetylcysteine are used to reduce risk.
And don’t forget over-the-counter supplements. Some herbal products - like aristolochic acid-containing herbs or high-dose vitamin C - have been linked to kidney scarring. Many patients don’t tell their doctors they’re taking them. That’s a gap that can cost lives.
Diabetes Medications: The New Rules
Diabetes and kidney disease often go together. But not all diabetes drugs are created equal when kidneys are weak.- Metformin: Was once banned in CKD. Now, it’s safe down to eGFR 30. But stop it if eGFR drops below 30. The risk of lactic acidosis is real - and deadly. One patient on Reddit shared: “My doctor didn’t check my eGFR for a year. I got sick from metformin. I was in ICU for 5 days.”
- Sulfonylureas (glyburide, glipizide): These cause low blood sugar. In CKD, the body can’t clear them well. Low sugar can lead to falls, seizures, or coma. Avoid them.
- SGLT2 inhibitors (dapagliflozin, empagliflozin): These are game-changers. They work the same whether your eGFR is 60 or 15. They reduce kidney failure risk by nearly 40%. They’re now recommended even if you don’t have diabetes. No dose adjustment needed. That’s rare.
- GLP-1 agonists (semaglutide, liraglutide): Also safe in CKD. They help with weight and heart protection. No dose changes required.
What’s changing fast? SGLT2 inhibitors are now first-line for CKD patients with albuminuria (protein in urine), even without diabetes. The 2024 KDIGO guidelines say they should be started early - not as a last resort.
ACE Inhibitors and ARBs: More Is Better
For years, doctors held back on ACE inhibitors (like lisinopril) and ARBs (like losartan) in CKD because they raised creatinine. That was a mistake.Now we know: a small rise in creatinine (up to 30%) when starting these drugs is normal and even a sign they’re working. The real danger is under-dosing. KDIGO 2024 says: titrate to the highest tolerated dose. Don’t stop them because creatinine went up. Studies show patients who get full doses live longer, with slower kidney decline.
But watch potassium. These drugs can cause high potassium levels - especially with CKD. If potassium goes above 5.5, you need to adjust. That’s why monthly blood tests are critical.
What About Antibiotics and Pain Meds?
Antibiotics are tricky. Vancomycin, for example, must be dosed by weight and eGFR. Trough levels (blood concentration) should be kept between 10-15 mcg/mL in CKD, not the usual 15-20. Too high? Risk of hearing loss. Too low? Infection won’t clear.For pain, acetaminophen (Tylenol) is the safest option, up to 3,000 mg/day. Avoid aspirin in high doses. Opioids? Use with caution. Morphine and codeine can build up. Hydromorphone or fentanyl are better choices, but still need lower doses.
And never assume a drug is safe just because it’s “prescribed.” One study found 23.7% of CKD patients were getting medications at inappropriate doses - not because doctors were careless, but because EHR systems don’t flag renal risks well. Many don’t auto-calculate eGFR or suggest dose changes.

How to Stay Safe: A Practical Plan
You don’t need to be a doctor to protect your kidneys from medication harm. Here’s what works:- Know your eGFR. Ask for it at every visit. Write it down. If it drops below 60, review all meds.
- Use one pharmacy. A 2023 NIDDK study showed a 42% drop in medication-related kidney injury when patients used a single pharmacy. Pharmacists can catch interactions you miss.
- Ask: “Is this safe for my kidneys?” Every time a new drug is prescribed - even OTC or supplements.
- Get a medication review every 3 months. KDIGO recommends this for CKD stages 3-5. Bring all pills, vitamins, and herbs.
- Use a renal dosing app. Apps like Epocrates Renal Dosing are used by 63% of U.S. nephrologists. Free versions exist. Input your eGFR and get instant alerts.
- Carry a kidney medication card. List your eGFR, allergies, and drugs you can’t take. Show it in the ER.
One patient, ‘CKDSurvivor’ on DaVita, said: “My nephrologist used a KDIGO checklist. We caught metformin at eGFR 38. Saved me from lactic acidosis.” That’s not luck. That’s system.
What’s Changing in 2025-2026
The field is moving fast. In August 2025, the DoD/VA updated guidelines to require PEG bowel prep for all CKD patients getting colonoscopies - sodium phosphate is now banned in their system. The FDA is preparing a 2026 update to its renal dosing guidance, using real-world data from EHRs. And KDIGO is rolling out a standardized medication safety checklist in Q2 2026 - the first of its kind.Pharmacogenomics is also emerging. Trials are testing if genetic differences in liver enzymes (CYP450) affect how CKD patients metabolize drugs. That could one day mean personalized dosing based on DNA - not just eGFR.
Final Thought: It’s Not About Fear - It’s About Awareness
Kidney disease doesn’t mean you can’t take meds. It means you need smarter meds. The goal isn’t to avoid all drugs - it’s to use the right ones, at the right dose, at the right time. SGLT2 inhibitors are now protecting kidneys. ACE inhibitors are saving lives. But ibuprofen? Still a trap.If you or someone you care about has CKD, don’t wait for a crisis. Start today: check your eGFR, list every pill you take, and ask your pharmacist: “Which of these could hurt my kidneys?” That one question could keep you out of the hospital - and protect your kidneys for years to come.
Can I still take ibuprofen if I have kidney disease?
No. Ibuprofen and other NSAIDs reduce blood flow to the kidneys and can cause sudden kidney injury, especially if your eGFR is below 60. Even short-term use can spike creatinine levels. Use acetaminophen (Tylenol) instead, up to 3,000 mg per day. Always check with your doctor before taking any pain reliever.
Is metformin safe for people with kidney disease?
Metformin is safe if your eGFR is 30 or above. But if your eGFR drops below 30, you must stop it - the risk of lactic acidosis becomes too high. Between eGFR 30-45, use caution and lower the dose. Always get your eGFR checked before refilling metformin. Many patients are unaware of this risk, leading to preventable hospitalizations.
Do I need to change my blood pressure meds if my kidneys are weak?
No - you may need to increase them. ACE inhibitors and ARBs are now recommended at maximum tolerated doses for kidney protection, even if your eGFR is below 30. A small rise in creatinine after starting these drugs is normal and expected. Don’t stop them unless potassium goes above 5.5 or you have signs of low blood pressure. Under-dosing these drugs is more dangerous than the creatinine rise.
What diabetes drugs are best for kidney disease?
SGLT2 inhibitors (like dapagliflozin) and GLP-1 agonists (like semaglutide) are now first-line. They protect the kidneys, reduce heart risks, and don’t need dose changes even with very low eGFR. Avoid sulfonylureas - they cause dangerous low blood sugar in kidney disease. Metformin is still an option if eGFR is above 30.
How often should I get my medications reviewed if I have CKD?
At least every 3 months if you have stage 3-5 CKD. More often if your eGFR is dropping quickly, you’re hospitalized, or you start a new drug. Many patients only see their doctor once a year - that’s not enough. A 2023 study found that quarterly reviews catch 80% of unsafe prescriptions before they cause harm.
Can over-the-counter supplements harm my kidneys?
Yes. Many herbal supplements - like those containing aristolochic acid, high-dose vitamin C, or creatine - can damage kidneys. Some are sold as “natural kidney support,” but they’re often harmful. A 2023 survey found 68% of CKD patients didn’t tell their doctor about supplements they were taking. Always disclose everything - even if you think it’s “just a vitamin.”
What should I do before a CT scan with contrast dye?
Tell the radiology team you have kidney disease. Ask if the scan is absolutely necessary. If it is, make sure you’re well-hydrated before and after. In some cases, your doctor may give you N-acetylcysteine to reduce risk. Avoid contrast dye if your eGFR is below 30 unless it’s life-saving. Always request a low-osmolar or iso-osmolar contrast agent - they’re safer.
Are there apps that help with kidney-safe dosing?
Yes. Epocrates Renal Dosing is used by 63% of U.S. nephrologists. It lets you input your eGFR and instantly shows safe doses for hundreds of drugs. Other free options include Medscape’s Renal Dosing Tool and the KDIGO app. These aren’t replacements for your doctor, but they’re powerful tools to help you ask better questions.
Why do some doctors still under-dose ACE inhibitors in CKD patients?
Outdated thinking. Many doctors were taught to avoid ACE inhibitors if creatinine rose, fearing kidney damage. But research shows that rise is a sign the drug is working - not harming. KDIGO 2024 calls under-dosing “suboptimal care.” Clinical trials proving benefit used maximum doses. If your doctor lowers your dose because creatinine went up, ask if they’ve read the latest guidelines.
What’s the biggest mistake CKD patients make with medications?
Assuming a drug is safe because it’s prescribed or sold over the counter. Many patients don’t realize that kidney disease changes how every drug behaves. They take ibuprofen for a headache, a supplement for energy, or an antibiotic from a previous prescription - and don’t tell their doctor. That’s how preventable kidney injuries happen. Always ask: “Is this safe for my kidneys?” - every single time.




Comments (14)
Karen Mccullouch
I can't believe people still take ibuprofen like it's candy. My mom had stage 4 CKD and took Advil for her arthritis-ended up in the ER with a creatinine of 7.2. They had to start her on dialysis for a week. 🤦♀️ Why do people think OTC means 'safe for everyone'??
Michael Gardner
SGLT2 inhibitors are first-line now? LOL. That’s what Big Pharma wants you to believe. The real reason? They’re expensive. And guess who pays? You. And the FDA? They’re just rubber stamps for drug companies. Wake up.
Willie Onst
Honestly? This post is a lifeline. I’ve been managing CKD for 8 years and no one ever told me about the EHR systems not flagging renal risks. I took metformin for years without knowing my eGFR dropped below 30. I’m alive because I asked my pharmacist one day: 'Is this safe?' That one question saved me. 🙏
Ronan Lansbury
KDIGO guidelines? More like KDIGO-Pharma-Collusion-Initiative. Did you know the same people who write these guidelines have stock in SGLT2 manufacturers? The 'eGFR below 30' rule? It’s not medical-it’s financial. And don’t get me started on 'PEG is safer.' That’s just a rebranded poison.
Jennifer Taylor
I JUST FOUND OUT MY MOM TOOK IBUPROFEN FOR 3 YEARS WITH EGF 28!!! SHE’S IN THE HOSPITAL NOW AND THE DOCTOR SAID 'IT’S A MIRACLE SHE’S STILL ALIVE' I’M CRYING RIGHT NOW WHY DOESN’T ANYONE TELL YOU THIS??!?!?!?!!
Shelby Ume
I’ve been a renal dietitian for 15 years, and I still see patients on NSAIDs. It’s heartbreaking. The most effective tool isn’t a new drug-it’s education. I give every patient a laminated card with the top 5 nephrotoxins. Simple. Free. Life-saving. If you’re reading this: print it. Share it. Don’t wait for a crisis.
Jade Hovet
OMG this is so important!! I just got my eGFR back and it’s 41 😱 I’ve been taking Aleve for my back pain for YEARS… I’m switching to Tylenol TODAY!! Also, I downloaded Epocrates Renal Dosing!! 🙌🙏 I’m telling all my CKD friends!! You’re a lifesaver!!
nithin Kuntumadugu
Lmao u think u know everything? U forgot about the chinese herbs my grandma took for 'kidney cleansing'-turned out they had aristolochic acid. Kidney gone in 6 months. And ur 'safest' drugs? SGLT2 inhibitors cause ketoacidosis. 200+ deaths reported. But hey, keep taking your 'game changer' pills.
John Fred
The real win here is SGLT2 inhibitors. They’re not just renal-protective-they’re cardioprotective, weight-reducing, and reduce hospitalizations for heart failure. In CKD patients with albuminuria, the number needed to treat to prevent one major adverse renal event is under 10. That’s a home run. And yes, you can use them even with eGFR 15. No dose adjustment needed. This is precision medicine.
Harriet Wollaston
I just got diagnosed with stage 3 CKD last month and I was terrified. But reading this made me feel like I’m not alone. I’m going to ask my doctor about SGLT2 inhibitors and get that medication review. I’m also printing out that kidney card. Thank you for writing this with so much heart. You’re helping people like me feel hopeful.
Lauren Scrima
Oh wow. So the 'safe' painkiller is Tylenol? Up to 3,000 mg? That’s… 6 extra-strength pills. Per day. And you’re telling me that’s not liver damage waiting to happen? 😅
sharon soila
Every single person with kidney disease deserves to know this. Knowledge is power. And power is protection. I’ve shared this with my church group, my book club, my neighbor who’s on dialysis. It’s not just medical advice-it’s a moral responsibility. Please, don’t wait. Check your eGFR. Ask the questions. Live well.
nina nakamura
This is the same garbage every year. SGLT2 inhibitors are overhyped. NSAIDs are vilified. But no one talks about the real killer: poor hydration and protein overconsumption. You’re blaming drugs because it’s easier than fixing diet and lifestyle. Your 'practical plan'? Useless without addressing the root cause.
Hamza Laassili
I work in a VA hospital and I see this EVERY DAY. People come in with creatinine at 6.5 because they took ibuprofen for a headache. The EHR? Doesn’t flag it. The nurse? Doesn’t ask. The doctor? Too busy. I had to manually override a prescription last week. Someone’s gonna die because of this system. Fix the tech, not just the meds.