Generic drugs make up 90% of all prescriptions filled in the U.S., yet they’re also behind 95% of all drug shortages. These aren’t rare glitches-they’re systemic failures built into how the system works. When a life-saving antibiotic, chemotherapy drug, or anesthetic disappears from hospital shelves, it’s rarely because of a sudden spike in demand. It’s because of deep-rooted problems in manufacturing and supply chains that have been ignored for years.
Manufacturing Problems Are the Main Cause
The single biggest reason generic drugs run out? Manufacturing failures. According to the FDA, 62% of all drug shortages between 2010 and 2023 were caused by issues at production facilities. These aren’t minor hiccups. They’re major shutdowns.
Think about it: a single contaminated batch can shut down an entire plant for months. If a sterile injectable like saline or vancomycin is made in a facility that fails an FDA inspection, every drug coming out of that line gets pulled. There’s no backup. No quick fix. Just silence while hospitals scramble.
These aren’t new factories with cutting-edge tech. Most are aging facilities running on tight budgets. They’re built to produce one thing, at one price, with no room for error. A broken filter, a leaky pipe, or even a small mold issue can trigger a recall. And because these drugs have razor-thin margins, manufacturers can’t afford to upgrade equipment or hire extra staff to prevent problems. So they wait until something breaks-and then they’re caught flat-footed.
Global Supply Chains Are Fragile
Over 80% of the active pharmaceutical ingredients (APIs) used in generic drugs come from just two countries: China and India. That’s not diversity. That’s a single point of failure.
When a flood hits a manufacturing zone in India, or a lockdown happens in a Chinese city, the ripple effect hits U.S. hospitals within weeks. In 2020, the pandemic didn’t just delay shipments-it froze entire production lines. One plant in China that made the active ingredient for heparin, a blood thinner used in every ICU, shut down for six months. No one had a backup supplier. No one had stockpiled enough. And patients suffered.
Even worse, many of these overseas facilities aren’t inspected as often as they should be. The FDA has limited staff and resources. They can’t be everywhere. So some plants slip through the cracks, producing drugs that meet standards on paper-but not in practice. When those drugs finally arrive in the U.S., they’re recalled. And the shortage gets worse.
No Extra Capacity Means No Safety Net
Generic drug makers don’t build extra capacity. They don’t keep spare machines running. They don’t hire extra workers just in case. Why? Because there’s no profit in it.
Branded drugs make 30-40% profit margins. Generic drugs? Often less than 15%. And with pharmacy benefit managers (PBMs) controlling 85% of prescription spending, they drive prices down to the bone. Manufacturers compete not on quality or reliability-but on who can make the cheapest version of a drug.
So they cut corners. They run factories at 100% capacity. They don’t invest in redundancy. If one machine breaks, there’s no spare. If one supplier fails, there’s no alternative. One plant makes 10 different drugs. If that plant shuts down, 10 shortages happen at once.
This isn’t just risky. It’s reckless. And it’s intentional. The system rewards the lowest bid, not the most reliable supplier.

One Supplier, One Drug
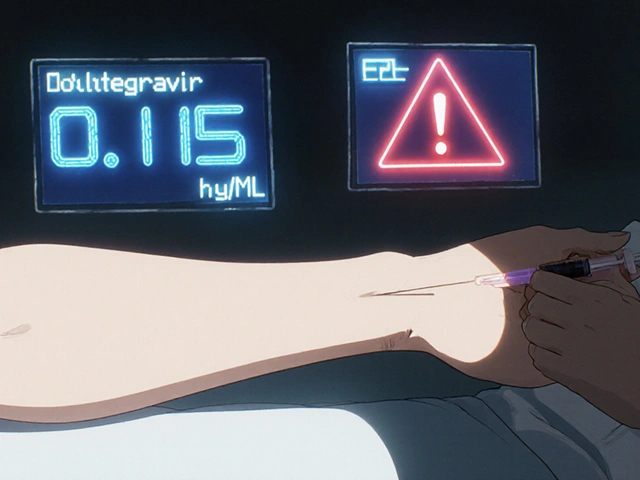
One in five drug shortages happens because a drug has only one manufacturer. That’s not competition. That’s monopoly by default.
Take dobutamine, a drug used to keep hearts beating during surgery. For years, only one company made it. When their facility had a quality issue in 2021, hospitals had no choice but to pause procedures. Patients waited. Some got worse. Others were moved to different hospitals-sometimes hundreds of miles away.
Why doesn’t another company step in? Because the price is too low. The FDA approved a second manufacturer for dobutamine in 2023-but they couldn’t make it profitable. So they didn’t launch. The market doesn’t reward new entrants. It punishes them.
Since 2010, over 3,000 generic drug products have been discontinued. Not because they weren’t needed. But because no one could make money selling them.
Market Forces Are Killing Supply
The problem isn’t just broken machines or foreign delays. It’s economics. The system is designed to fail.
Pharmacy benefit managers (PBMs) negotiate bulk discounts. They demand lower prices. They reward manufacturers who offer the cheapest deal-even if that deal means cutting staff, skipping inspections, or delaying maintenance. Hospitals don’t choose the drugs. PBMs do. And they don’t care if a drug is in shortage. They care if it’s the lowest price.
Meanwhile, manufacturers are caught in a trap. If they raise prices to cover costs, they lose contracts. If they keep prices low, they can’t invest in quality. So they leave. Or they stop making the drug altogether. And the shortage grows.
The result? A shrinking pool of manufacturers. Fewer factories. Fewer workers. Fewer options. And more patients at risk.
Canada Does It Better
Canada has the same generic drug market. Same global supply chains. Same low prices. But they have far fewer shortages.
Why? Because they don’t rely on the market alone. Canada has a national drug stockpile. When a shortage hits, they pull from it. They coordinate between regulators, hospitals, and manufacturers. They talk to each other. They plan ahead.
The U.S. doesn’t. Our strategic national stockpile is for bioterrorism or natural disasters-not everyday drug shortages. There’s no national plan. No coordination. No backup.
Canadian pharmacists spend less time managing shortages. U.S. pharmacists spend 50-75% more time just trying to find alternatives. That’s not efficiency. That’s chaos.
What’s Being Done?
There are signs of change. In 2023, Congress introduced the RAPID Reserve Act. It proposes creating a strategic reserve for critical generic drugs. It wants to incentivize domestic manufacturing. It wants to reduce reliance on single-source suppliers.
The FTC is also investigating PBMs. Their 2023 report called their practices ‘lacking transparency’ and ‘harmful to patients.’ That’s a start. But it’s not enough.
Some hospitals are building their own stockpiles. Some states are passing laws to require manufacturers to report shortages earlier. But without fixing the economics, none of it will last.
What Needs to Change
This isn’t about blame. It’s about design. The system was built for cheap, not reliable. And now it’s breaking.
We need:
- Minimum stockpiles of critical generics-like antibiotics, anesthetics, and chemotherapy drugs.
- Financial incentives for manufacturers to keep producing low-margin drugs, even if they’re not profitable.
- More domestic production of APIs-not just finished pills, but the raw ingredients.
- Transparency-manufacturers must report problems before they become crises.
- Regulation of PBMs-they shouldn’t be the ones deciding which drugs are available.
Right now, we’re treating drug shortages like accidents. They’re not. They’re predictable. And they’re preventable.
When a patient can’t get their cancer drug because the factory in India shut down, it’s not bad luck. It’s policy failure. And it’s happening every single day.
Why are generic drugs more likely to be in shortage than brand-name drugs?
Generic drugs have much lower profit margins-often under 15%-compared to 30-40% for brand-name drugs. This makes manufacturers less likely to invest in quality control, equipment upgrades, or backup production lines. With intense price pressure from pharmacy benefit managers (PBMs), companies cut costs until they can’t afford to keep making the drug. As a result, 95% of all drug shortages involve generics, even though they make up 90% of prescriptions.
How do manufacturing inspections contribute to drug shortages?
When the FDA finds violations-like contamination, poor sanitation, or faulty equipment-at a drug manufacturing facility, they can halt production until fixes are made. These shutdowns can last months. Because many generic drugs are made in just one or two plants worldwide, a single inspection failure can cause a nationwide shortage. The FDA can’t inspect every facility often enough, and overseas plants are especially hard to monitor closely.
Why can’t we just make more generic drugs in the U.S.?
We could-but it’s not profitable. Building a FDA-compliant manufacturing facility costs over $100 million. For a drug that sells for pennies per pill, the return on investment is too low. Manufacturers prefer to produce in countries with lower labor and regulatory costs. Without government subsidies or guaranteed minimum prices, no company will risk the upfront cost.
Do pharmacy benefit managers (PBMs) cause drug shortages?
PBMs don’t cause shortages directly, but they create the conditions that make them inevitable. By negotiating the lowest possible prices and favoring drugs with the deepest discounts, they push manufacturers to cut corners. When profit margins shrink below 10%, companies stop investing in quality, stop expanding capacity, and eventually stop making the drug altogether. PBMs control 85% of U.S. prescription spending, so their pricing decisions shape the entire market.
Are there any drugs that are always in shortage?
Yes. Certain generic sterile injectables-like sodium bicarbonate, epinephrine, and propofol-have been in and out of shortage for over a decade. These drugs are cheap, complex to manufacture, and have low margins. Few companies want to make them. When one manufacturer shuts down or gets inspected, there’s often no backup. These drugs are used in emergency rooms, ICUs, and operating rooms, so shortages put lives at immediate risk.
What can hospitals do when a drug is in shortage?
Hospitals can try to find alternative drugs, ration existing supplies, or delay non-urgent treatments. But alternatives aren’t always safe or effective. For example, switching from one chemotherapy drug to another can reduce treatment success rates. Pharmacists spend 50-75% more time managing shortages than they did 10 years ago, often working with limited information. Without a national tracking system or stockpile, hospitals are left to improvise under pressure.



Comments (12)
Spencer Garcia
Been working in hospital pharmacy for 15 years. This isn’t news-it’s a daily grind. We’re juggling 3-5 shortages at any given time. Last month, we ran out of midazolam for 11 days. No backup. No warning. Just a call from the OR saying they can’t sedate patients. We patched it with off-label stuff. Not ideal. But that’s the system now.
Abby Polhill
APIs from India and China aren’t just ‘global supply chains’-they’re strategic vulnerabilities. We outsourced our pharmaceutical sovereignty like it was a call center. Now we’re paying the price in ICU delays and canceled surgeries. The FDA’s inspection backlog? It’s not bureaucratic inefficiency-it’s policy abandonment.
Usha Sundar
My uncle’s chemo got delayed because the vancomycin ran out. He’s fine now. But it shouldn’t have happened. Not in 2024.
Bret Freeman
This entire system is a Ponzi scheme built on the backs of sick people. PBMs are the real villains. They don’t care if you live or die-they care if the rebate check clears. They’re not intermediaries. They’re parasites. And Congress? They take their money. So we get shortages. It’s not an accident. It’s a business model.
They’ll pass another ‘RAPID Reserve Act’ and call it progress. Meanwhile, the same factories keep failing inspections. Same PBMs keep squeezing margins. Same hospitals keep scrambling. We’re not fixing the system. We’re decorating the coffin.
Aurora Daisy
Canada’s ‘better’? Sure, if you like rationing and 6-month wait times for everything. Their system works because they don’t let people have choices. We’d rather have shortages than surrender our freedom to a state-run drug bureaucracy. You want stability? Move to North Korea. At least they have a stockpile.
Steven Mayer
The FDA’s inspection protocols are outdated. They still rely on paper audits and scheduled visits. Meanwhile, manufacturers use AI-driven predictive maintenance and real-time contamination sensors. The disconnect is systemic. We’re regulating 1980s infrastructure with 1990s tools. No wonder things keep breaking.
And don’t get me started on the lack of real-time inventory tracking. Hospitals still fax shortage alerts. We’re running a 21st-century healthcare system on 1970s infrastructure.
Georgia Brach
Let’s be clear: this isn’t about ‘profit margins.’ It’s about moral hazard. Manufacturers know the government will bail them out with emergency waivers or temporary import permits. So they don’t invest. They wait. They gamble. And patients pay the cost. This isn’t capitalism-it’s cronyism disguised as free markets.
And the ‘Canadian model’? They don’t have shortages because they don’t have innovation. No one’s developing new generics there because there’s no upside. We’re the ones pushing the science. They’re just free-riding. Don’t mistake stagnation for stability.
Dan Gaytan
There’s hope. I’ve seen small manufacturers in Ohio and Pennsylvania start up with state grants to make critical injectables. One guy in Indiana is building a sterile compounding lab that could supply 20 hospitals. It’s slow. It’s messy. But it’s real. We don’t need a federal mandate-we need local champions. And we need to stop treating drug manufacturing like a commodity.
Support local. Demand transparency. Talk to your reps. Change doesn’t come from D.C. It comes from the guy who refuses to give up.
Pankaj Chaudhary IPS
As someone who’s worked in public health across three continents, I can say this: India and China produce generics because they have the scale, not because they’re inferior. The issue isn’t geography-it’s governance. We need bilateral quality accords, not protectionism. Invest in training Indian inspectors. Fund joint FDA-CDSCO audits. Build mutual accountability. That’s how you fix supply chains-not by pulling out.
And yes, profit margins are thin. But that’s why we need public-private partnerships. Not subsidies. Not bailouts. Incentives tied to reliability metrics. If you maintain 98% uptime on critical drugs, you get priority in future tenders. Simple. Transparent. Sustainable.
bharath vinay
Who really owns the FDA? Big Pharma. They own the regulators. They own the Congress. The shortages? They’re not accidents. They’re engineered. Why? So they can push you toward their expensive branded drugs. You think vancomycin is hard to get? Wait till your insurance denies your $12,000 cancer pill and says ‘try the generic.’ Then you’ll see how fast they fix it.
It’s all a show. The RAPID Reserve Act? A distraction. They’ll spend $500 million on stockpiles while letting the factories rot. The real solution? Break up the PBMs. Nationalize the APIs. And shut down every factory that’s been cited twice.
Joe Jeter
Everyone’s blaming PBMs and China. But let’s be honest-nobody wants to pay more for a drug. You want reliability? Then pay for it. Stop screaming about $0.10 pills. If you’re willing to pay $20 instead of $5 for a lifesaving antibiotic, manufacturers will invest. But you’re not. You want it cheap, safe, and available. That’s not a market. That’s a fantasy.
We’ve conditioned ourselves to expect miracles at discount prices. Now we’re surprised when the miracle stops working. Wake up.
Payson Mattes
Did you know the same company that makes your generic blood pressure pill also makes the nerve agent antidote for the military? And that plant in Hyderabad? It’s owned by a Chinese state-owned enterprise that also controls 70% of the rare earth minerals used in fighter jets. You think this is about drugs? No. This is about control. The next time you get a shortage, ask yourself: who benefits? It’s not the hospitals. It’s not the patients. It’s the ones pulling the strings from behind the scenes.
They’re not just making pills. They’re making power. And they’re using your medicine as leverage.