What is Hyperkalemia in CKD?
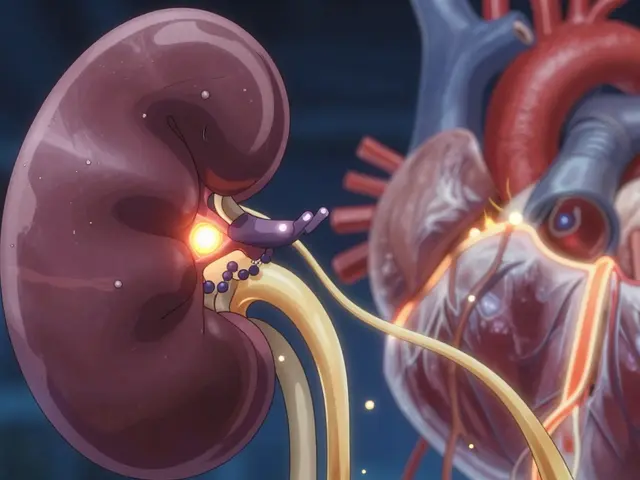
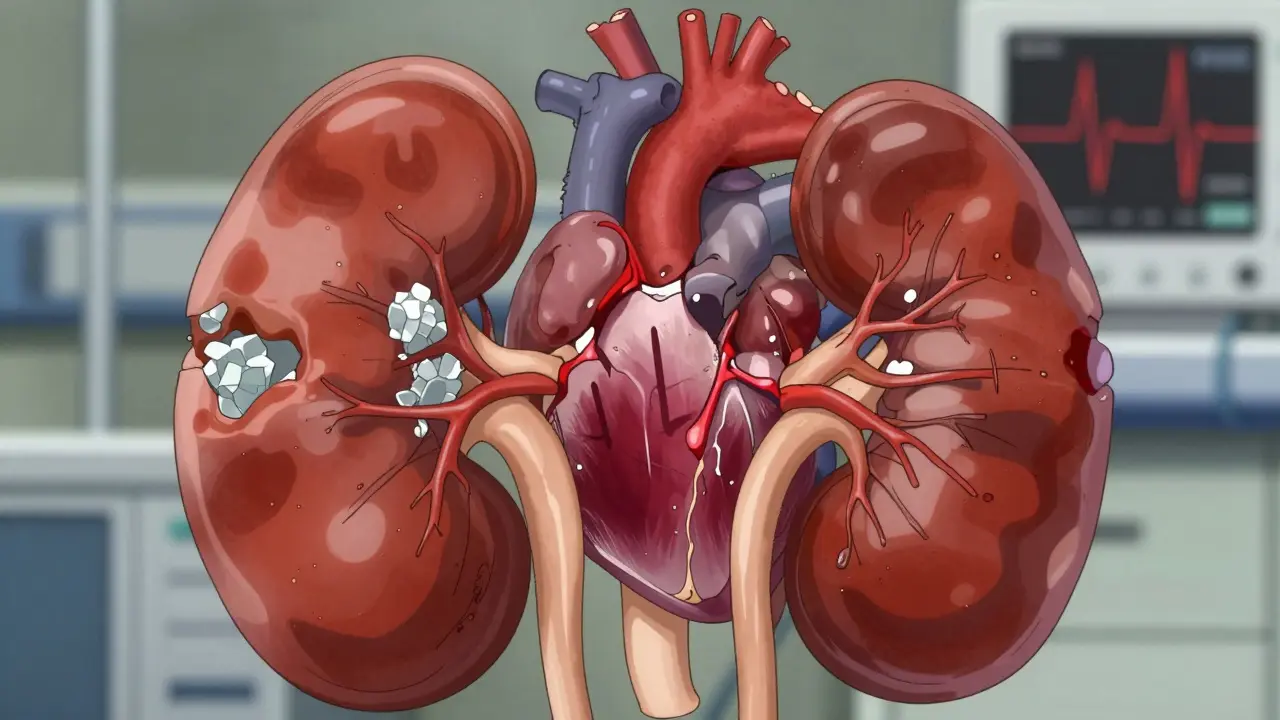
Hyperkalemia is a condition where serum potassium levels rise above normal. In Chronic Kidney Disease (CKD), the kidneys lose their ability to filter excess potassium from the blood. This affects about 40-50% of patients with advanced CKD, according to the 2022 Renal Association Clinical Practice Guidelines. Normal potassium levels are 3.5-5.0 mmol/L, but levels above 5.0 mmol/L can cause dangerous heart rhythms or even cardiac arrest.
Dietary Management for Different CKD Stages
For people with early-stage CKD (stages 1-3a), a 'prudent but not restrictive' approach is recommended. But as kidney function declines, stricter limits apply. Those with stage 3b-5 CKD (not on dialysis) need to keep potassium intake to 2,000-3,000 mg daily - roughly half of what healthy adults consume. Practical swaps make this easier: instead of oranges (181 mg per fruit), try apples (145 mg), and replace potatoes (421 mg per 100g) with cauliflower (29 mg per 100g). A 2023 study found that patients who followed these dietary changes reduced their emergency hyperkalemia episodes by 40%.
Common high-potassium foods include bananas (422 mg per medium), oranges (181 mg), tomatoes (237 mg per cup), and spinach (839 mg per cup cooked). Work with a Renal Dietitian to create a personalized meal plan. They can help identify hidden sources of potassium in processed foods and suggest safe alternatives. For example, swapping white rice for brown rice can lower potassium intake while maintaining nutrition.

Emergency Treatment for Critical Potassium Levels
If potassium reaches 5.5 mmol/L or higher with ECG changes like peaked T-waves, immediate action is critical. Doctors typically start with Calcium Gluconate IV to stabilize the heart within minutes. This is followed by insulin and glucose to lower potassium within 30 minutes. For patients with metabolic acidosis, sodium bicarbonate can help. These steps buy time while addressing the underlying cause.
According to the 2022 Renal Association Guidelines, calcium gluconate (10 mL of 10% solution IV over 2-5 minutes) is given when ECG changes occur. Insulin (10 units regular insulin with 50 mL 50% dextrose) lowers potassium by 0.5-1.5 mmol/L within 30 minutes but carries a 10-15% risk of hypoglycemia. Sodium bicarbonate (50-100 mmol IV) acts within 5-10 minutes for patients with low bicarbonate levels. These interventions are life-saving but temporary - they don't remove potassium from the body.
Chronic Management with Potassium Binders
Long-term control often requires potassium binders. Older options like Sodium Polystyrene Sulfonate (SPS) have risks like colonic damage, but newer drugs like Patiromer and Sodium Zirconium Cyclosilicate (SZC) are safer. Patiromer works over 4-8 hours and is sodium-neutral, making it better for heart failure patients. SZC acts faster (within 1 hour) but adds sodium, which might worsen swelling. In clinical trials, patiromer helped 78% of patients stay on heart-protective RAAS inhibitors, while SZC maintained 83% of mineralocorticoid receptor antagonist use.
RAAS inhibitors like ACE inhibitors or ARBs are crucial for protecting kidneys and heart, but they increase hyperkalemia risk. The trade-off is worth it: discontinuing these medications raises the risk of heart attacks and kidney failure. Newer binders have changed this equation. A 2023 study by Fiaccadori et al. showed that patiromer and SZC allow doctors to maintain optimal RAAS inhibitor doses in most patients, reducing the need for dangerous potassium level spikes.

Monitoring and Long-Term Care
Regular blood tests are key. Check potassium every 1-2 weeks after starting RAAS inhibitors, then every 3-6 months if stable. Symptoms like muscle cramps or irregular heartbeat mean test immediately. A 2022 survey of 247 nephrologists showed that structured monitoring every three months increased medication adherence by 29% and reduced hospital visits for hyperkalemia by half.
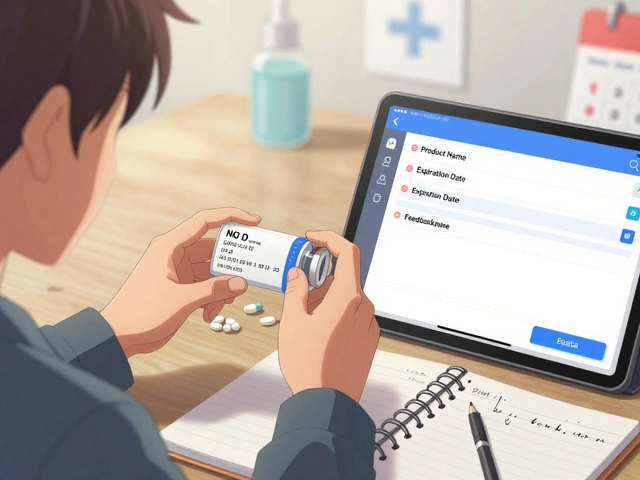
Modern tools help too. A 2023 pilot study found that smartphone apps tracking food potassium content improved dietary adherence by 32%. These apps scan barcodes and calculate potassium in real-time - a game-changer for people struggling with dietary restrictions. For advanced CKD patients, consistent monitoring and medication adjustments can prevent hyperkalemia from becoming a life-threatening issue.
Frequently Asked Questions
What foods should I avoid with hyperkalemia in CKD?
Common high-potassium foods to limit include bananas, oranges, potatoes, tomatoes, spinach, and avocados. For example, one medium banana contains 422 mg of potassium, which could be nearly half your daily limit in advanced CKD. Instead, choose lower-potassium options like apples (145 mg per fruit), berries (100 mg per half-cup), or cauliflower (29 mg per 100g). A renal dietitian can help you create a safe meal plan based on your specific kidney function.
Can I take potassium binders with my other medications?
Yes, but timing matters. Patiromer can reduce absorption of medications like levothyroxine by 23% if taken within 3 hours. Always take potassium binders at least 4 hours apart from other medications. Sodium zirconium cyclosilicate (SZC) has fewer drug interactions but still requires careful timing. Your pharmacist can help coordinate your medication schedule to avoid interactions while managing hyperkalemia effectively.
What happens if I ignore high potassium levels?
Ignoring hyperkalemia can lead to serious complications. As potassium rises above 6.0 mmol/L, ECG changes like widened QRS complexes can occur, increasing the risk of cardiac arrest. Studies show that each 0.5 mmol/L increase in potassium above 5.0 mmol/L raises the risk of death by 18%. Emergency treatment is critical at these levels - delaying care can be life-threatening. Always seek medical help if you experience symptoms like muscle weakness, irregular heartbeat, or chest pain.
How do newer potassium binders compare to older ones?
Older binders like sodium polystyrene sulfonate (SPS) carry significant risks, including colonic necrosis (0.5-1.0% incidence) and sodium overload (11 mmol Na per gram). Newer options like patiromer and sodium zirconium cyclosilicate (SZC) are much safer. Patiromer causes constipation in 14.2% of patients but is sodium-neutral, while SZC acts faster (within 1 hour) but may cause edema in 12.3% of heart failure patients. Both have replaced SPS as first-line treatments due to better safety profiles and effectiveness in maintaining RAAS inhibitor therapy.
Is it safe to continue RAAS inhibitors with hyperkalemia?
Yes, and it's often safer than stopping them. Discontinuing RAAS inhibitors increases cardiovascular event risk by 28% and kidney disease progression by 34%. With modern potassium binders, 78-83% of patients can maintain full RAAS inhibitor doses. A 2022 study showed that using patiromer or SZC allows doctors to keep patients on heart-protective medications while controlling potassium. Always work with your nephrologist to balance these benefits - the risks of stopping RAAS inhibitors often outweigh the risks of hyperkalemia with proper management.