
Nephrotoxic Medication Hydration Calculator
Your Kidney Health Assessment
Your Personalized Hydration Plan
Not Calculated
Why Hydration Matters When You’re on Nephrotoxic Medications
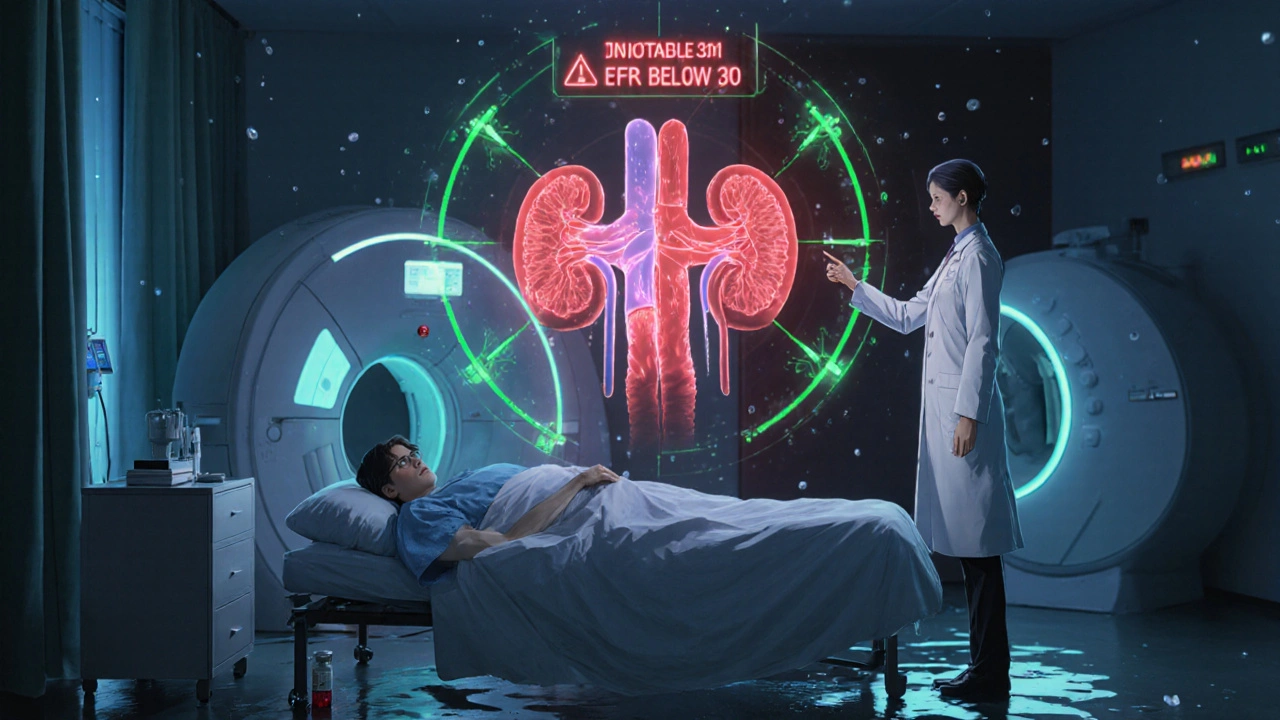
Some medicines you take for heart disease, cancer, or imaging tests can quietly damage your kidneys. These are called nephrotoxic medications. The most common culprit? Contrast dye used in CT scans, angiograms, and other imaging procedures. If you have reduced kidney function, diabetes, or heart failure, this dye can cause contrast-induced acute kidney injury - a sudden drop in kidney function that can lead to longer hospital stays, dialysis, or even permanent damage.
But here’s the good news: simple, well-timed hydration can cut that risk by more than half. It’s not about drinking more water randomly. It’s about using the right fluids, at the right time, in the right amount - based on your kidney health and medical history.
How Contrast Dye Harms the Kidneys (And How Hydration Stops It)
Contrast dye thickens the blood and reduces blood flow to the kidneys. It also triggers oxidative stress inside kidney cells. In healthy people, the kidneys handle this fine. But if your kidneys are already working hard - say, from chronic kidney disease or high blood pressure - they can’t cope. The result? Cell damage, inflammation, and reduced urine output.
Hydration works by keeping blood flowing through the kidneys and diluting the dye so it doesn’t stick around long enough to cause harm. Think of it like flushing a clogged drain: more water = faster cleanup. Studies show that patients who get proper hydration before and after contrast exposure are far less likely to develop kidney injury.
The Three Main Hydration Protocols - And Which One Works Best
Not all hydration is created equal. There are three proven methods, each with different effectiveness, cost, and complexity.
- Standard IV Saline (0.9% sodium chloride): The most common approach. Given at 3-4 mL per kg of body weight per hour, starting 4 hours before and continuing 4 hours after the procedure. Reduces kidney injury risk by about 26% compared to no hydration.
- Sodium Bicarbonate IV: Uses a slightly alkaline solution to neutralize acid buildup in kidney cells. Administered as 154 mmol/L solution at 3 mL/kg/hr for 1 hour before, then 1 mL/kg/hr for 6 hours after. Reduces risk by 26% - same as saline, but may offer extra protection in high-risk patients.
- RenalGuard System: A closed-loop machine that tracks your urine output in real time and automatically adjusts IV fluid to keep you peeing 150-200 mL per hour. This is the most effective method, cutting kidney injury risk by 68%. But it’s expensive and needs special equipment and trained staff.
For patients with eGFR below 60 mL/min/1.73m² - meaning moderate to severe kidney impairment - RenalGuard or hemodynamic-guided hydration (which uses blood pressure and heart metrics to tailor fluid) is strongly recommended. For those with normal kidney function (eGFR above 60), standard saline is often enough.
Oral Hydration: A Simple, Safe Alternative
You don’t always need an IV. For many patients - especially those who are stable, mobile, and have no heart failure - drinking water works just as well.
Studies show that drinking 500 mL of water two hours before the procedure, then 250 mL every hour during and after, matches the kidney protection of IV fluids. In one trial, CI-AKI rates were 4.7% with oral hydration versus 5.1% with IV - no meaningful difference.
Oral hydration is cheaper, less invasive, and lets you stay comfortable. But it only works if you can drink consistently and aren’t nauseated, vomiting, or on fluid restrictions due to heart failure.

Who Can Skip Hydration Altogether?
Not everyone needs it. If your eGFR is above 29 mL/min/1.73m² - meaning your kidney function is mild to normal - research shows you likely don’t benefit from prophylactic hydration. One 2018 study found no difference in kidney injury rates between patients who got fluids and those who didn’t.
This matters because unnecessary hydration can cause problems. Too much fluid in someone with heart failure can lead to pulmonary edema - fluid in the lungs - which can be life-threatening. Doctors now use a risk-based approach: check your eGFR, look at your heart health, then decide.
When Advanced Hydration Makes Sense (And When It Doesn’t)
Advanced systems like RenalGuard aren’t for everyone. They’re best for:
- Patients with CKD stage 3 or worse (eGFR < 60)
- Those with heart failure or diabetes
- People getting large volumes of contrast dye
- High-risk procedures like cardiac catheterization
But they cost about $1,200 more per procedure. For a healthy 70-year-old getting a routine CT scan with low-dose dye? Probably overkill. Hospitals are starting to use AI tools to predict who’s at risk - and only offer advanced hydration to those who truly need it.
What Your Doctor Should Check Before You Get Hydrated
Before any hydration plan starts, your care team needs to know:
- Your most recent eGFR (estimated glomerular filtration rate) - ideally from the last 30 days
- Your heart function (ejection fraction if you’ve had an echo)
- Whether you’re on metformin, diuretics, or ACE inhibitors - all affect kidney fluid balance
- Your current fluid restrictions - many heart patients must limit daily intake
- Whether you’ve had kidney injury from contrast before
If your eGFR is below 30, your doctor may suggest skipping contrast entirely and using an MRI instead. No dye = no risk.
Real-World Results: What Happens When Hospitals Do This Right
The Mayo Clinic reduced contrast-induced kidney injury from 12.3% to 5.7% in just one year by standardizing hydration protocols across radiology, cardiology, and nursing teams. They created checklists, trained staff, and made hydration part of the pre-procedure checklist - like verifying allergies or fasting.
Hospitals that don’t use protocols see 2-3 times more kidney injury cases. That means more patients needing dialysis, longer stays, and higher costs - about $7,500 extra per case.
What You Can Do Today
Don’t wait for your doctor to bring it up. Ask these questions before any imaging test:
- “Will I need contrast dye?”
- “What’s my eGFR, and am I at risk for kidney injury?”
- “Should I get IV fluids, oral fluids, or neither?”
- “Do I need to stop any of my meds before or after?”
- “Will you check my creatinine 48 hours after?”
If you’re told you need hydration, follow the plan. Don’t skip the post-procedure fluids just because you feel fine. Kidney damage often shows up 2-3 days later.
What’s Coming Next
By 2030, AI-driven systems will likely predict your kidney’s response to contrast in real time - adjusting fluids automatically based on your body’s signals. Some hospitals are already testing biomarkers that detect early kidney cell stress within minutes of dye exposure.
For now, the best defense is simple: know your kidney numbers, ask the right questions, and follow the hydration plan - whether it’s water in a bottle or IV in your arm.
Can drinking water prevent kidney damage from contrast dye?
Yes, drinking water can help - especially if you’re healthy and your kidneys are working well. Studies show that drinking 500 mL two hours before and 250 mL per hour during and after the procedure works just as well as IV fluids for most people with normal kidney function. But if you have heart failure, kidney disease, or are very ill, IV hydration under medical supervision is safer and more controlled.
Is IV hydration always better than oral hydration?
No. For patients with normal kidney function (eGFR above 60), oral hydration is noninferior to IV. In fact, it’s often preferred because it’s less invasive and avoids risks like fluid overload. IV is reserved for high-risk patients - those with CKD, diabetes, heart failure, or those getting large amounts of contrast dye. The goal isn’t to use the most aggressive method - it’s to use the right method for your body.
Should I stop my blood pressure meds before getting contrast?
Sometimes. Medications like ACE inhibitors, ARBs, and diuretics can increase the risk of kidney injury when combined with contrast dye. Many doctors will ask you to hold them 24-48 hours before the procedure - especially if you have kidney disease. But never stop your meds without talking to your doctor. For some patients, especially those with heart failure, stopping these drugs can be dangerous.
Can I get kidney damage from contrast dye even if I’m hydrated?
Yes, but it’s much less likely. Hydration reduces risk by 26-68%, depending on the method. However, if you have very advanced kidney disease (eGFR below 30), your kidneys may still be vulnerable even with hydration. In these cases, doctors often avoid contrast entirely and use MRI or ultrasound instead. Hydration helps - but it’s not a magic shield.
How long after the procedure should I get my kidney function checked?
Your creatinine should be checked 48 to 72 hours after the procedure. That’s when kidney injury, if it’s going to happen, becomes visible in blood tests. Some hospitals do it sooner, but 48-72 hours is the standard window. If you’re discharged before then, make sure you have a plan to get the test done - whether at a lab, urgent care, or your primary care clinic.
Are there any side effects from hydration fluids?
Yes - but they’re rare if done properly. Too much IV fluid can cause fluid overload, especially in people with heart failure or low heart function. This can lead to swelling, shortness of breath, or even pulmonary edema. Sodium bicarbonate can cause alkalosis if given too fast. Oral hydration is safer but can cause nausea if drunk too quickly. That’s why hydration plans are tailored - not one-size-fits-all.
Does N-acetylcysteine (NAC) help protect kidneys from contrast dye?
Not really. Multiple studies, including a 2020 meta-analysis of over 21,000 patients, found that NAC offers no additional benefit when adequate hydration is already used. It’s not recommended in current guidelines. Some clinics still give it out of habit, but evidence doesn’t support it. Focus on hydration instead.



Comments (16)
vanessa parapar
I've seen so many patients get wrecked by contrast dye because no one bothered to hydrate them properly. Seriously, if your eGFR is under 60 and you're getting a CT with contrast, you're basically gambling with your kidneys. Water isn't optional-it's medical-grade prevention. Stop treating hydration like a suggestion.
Ben Wood
I'm sorry, but I have to say-this entire article is dangerously oversimplified. IV hydration isn't a panacea. The RenalGuard system? It's not just expensive-it's over-engineered for most cases. And the claim that oral hydration is 'non-inferior'? That's based on a 2017 meta-analysis that excluded patients with NYHA Class III/IV heart failure. You're leaving out the critical exceptions.
Sakthi s
Simple truth: drink water. Stay hydrated. Ask your doctor. No magic needed.
Rachel Nimmons
I wonder how many of these 'hydration protocols' are just profit-driven. Who benefits from IV lines and RenalGuard machines? Hospitals. Pharma. Radiology departments. What if the real solution is just… not using contrast unless absolutely necessary? Did anyone ever ask that question?
Abhi Yadav
We are all just temporary vessels of water and electricity anyway. The body knows what it needs. If your kidneys are screaming for help, maybe you're not listening to the universe. 🌊💧
Julia Jakob
Okay but like… why are we still using contrast dye at all? It’s 2025. We have MRI, ultrasound, AI-enhanced imaging, and yet we’re still shoving toxic chemicals into people’s veins because it’s ‘faster’? This feels like sticking a bandaid on a bullet wound and calling it progress. Also, NAC? Please. That’s just placebo with a fancy name.
Robert Altmannshofer
Honestly? This is one of those rare medical topics where the solution is both dumb-simple and wildly underused. People think hydration means chugging a gallon of water the night before. Nah. It’s about rhythm. Timing. Consistency. Like brushing your teeth-you don’t do it once a year and call it good. And honestly? The fact that some hospitals still don’t have a hydration checklist? That’s criminal. We know how to prevent this. We just don’t always do it.
Kathleen Koopman
I just had a CT last week and drank 500ml before and kept sipping water. Felt great afterward! 🥤💙 No IV, no fuss. My nephrologist said I did it right. So glad I read this before my appointment!
Nancy M
In my experience working across multiple healthcare systems in the U.S., the disparity in hydration protocols is staggering. In urban academic centers, RenalGuard is standard. In rural clinics? They hand you a plastic cup of water and say 'drink up.' This isn't just medical-it's socioeconomic. Access to care shouldn't be determined by zip code.
gladys morante
I'm not saying this isn't important, but I've been on dialysis for three years now. No one ever told me about this until after I had three bad reactions. Why is this information so hidden? Why do patients have to dig for it? It feels like we're being set up to fail.
Precious Angel
Let me tell you what they don't want you to know. The entire contrast dye industry is a multi-billion dollar scam. They don't care about your kidneys. They care about the revenue from scans, the IV bags, the RenalGuard machines, the follow-up labs. They profit from your fear of missing a diagnosis. And hydration? It's the one thing they can't bill for. That's why it's buried in the fine print. They want you to think you need the expensive stuff. You don't. You need truth. And truth is, you probably don't need the dye at all.
Melania Dellavega
There's something beautiful about how something so simple-drinking water-can be so profoundly healing. We live in a world that glorifies high-tech fixes, but sometimes the most powerful medicine is the oldest one: hydration, patience, and listening to your body. I wish more doctors saw it that way.
Bethany Hosier
I must respectfully submit that the empirical data presented herein, while statistically significant, fails to account for the confounding variables associated with systemic healthcare inequities, particularly in the context of racialized biomarker interpretation and institutional bias in eGFR calculation algorithms. The implicit assumption that eGFR is a neutral metric is scientifically untenable.
Krys Freeman
Why are we spending money on this? In my country, we just tell people to drink water. End of story. This is overkill.
Shawna B
So drink water before the scan? Got it.
Jerry Ray
Wait-so if I have an eGFR of 65 and I'm healthy, I don't need hydration? But if I have an eGFR of 59 and I'm healthy, I do? That's a 1-point difference. That's not medicine. That's a spreadsheet.