
Medication Interaction Checker
Check for Medication Interactions
Enter medications to see potential interactions and how a collaborative healthcare team would identify them.
Added Medications
Potential Interactions
According to studies cited in the article:
30%+ of side effects can be reduced with collaborative care teams
67% fewer adverse events when pharmacists are part of the care team
Why Medication Side Effects Are a Team Problem
Take a patient on five different medications for diabetes, high blood pressure, and arthritis. They start feeling dizzy, nauseous, and exhausted. They go to their doctor, who adjusts one drug. A week later, the dizziness gets worse. They visit a specialist, who adds another pill for the nausea. The cycle continues. This isn’t rare-it’s the norm in fragmented care. The real issue isn’t the drugs themselves. It’s that no one is looking at the full picture.
Side effects don’t happen in isolation. They’re the result of drug interactions, dosing mismatches, patient misunderstandings, and missed follow-ups. A 2022 JAMA Internal Medicine study found that medication errors cause 67% fewer adverse events when pharmacists are part of the care team. That’s not luck. It’s structure.
Doctors diagnose. Specialists treat. But pharmacists? They know every pill, every interaction, every hidden risk. When they sit at the table with the rest of the team, side effects stop being accidents. They become preventable.
What Each Member Actually Does in a Collaborative Team
It’s not just about having more people in the room. It’s about knowing who does what-and doing it together.
Doctors lead diagnosis and set treatment goals. But they don’t have time to memorize 1,200+ drug interactions. That’s where pharmacists come in. They review every prescription, flag risky combinations, and catch duplications. In hospital rounds, pharmacists now participate in 78% of patient care discussions, according to PMC11075915. They don’t just say, “This drug might cause drowsiness.” They say, “This drug combined with the patient’s sleep aid increases sedation risk by 40%. Let’s switch to a non-sedating alternative.”
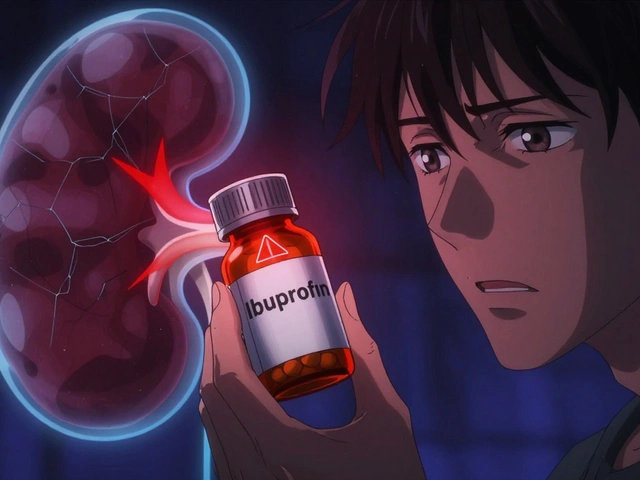
Specialists-like cardiologists or endocrinologists-focus on their organ system. But they often don’t see the full medication list. A cardiologist might prescribe a blood thinner. An endocrinologist might add a new diabetes drug. Neither knows the patient is also taking an over-the-counter NSAID for back pain. That combo? It can cause internal bleeding. A pharmacist spots it before the patient even leaves the clinic.
Nurses monitor symptoms. Patients report how they feel. But without a pharmacist translating those reports into medication changes, nothing shifts. In a 2023 study, patients under collaborative care reported 89% satisfaction because someone finally asked: “Are you still taking that pill you were told to stop?”
How Collaboration Lowers Side Effects by 30% or More
Numbers don’t lie. When pharmacists join the team, side effects drop. Not a little. A lot.
In a landmark NEJM study, African-American men with uncontrolled hypertension saw their blood pressure drop to normal levels in 94% of cases-compared to just 29% under standard care. That’s not because of a new drug. It’s because pharmacists adjusted doses weekly, checked for interactions with diet supplements, and made sure patients understood how to take their pills.
For diabetes, collaborative teams achieved 1.2% greater HbA1c reduction than solo doctor care. That might sound small, but it’s the difference between avoiding nerve damage and facing amputation risk.
Anticoagulation therapy? One pharmacist-led program cut bleeding events by 31%. Why? Because they tracked INR levels daily, adjusted warfarin doses based on diet changes, and called patients directly when labs looked off. No waiting for the next appointment. No guessing.
These aren’t outliers. A 2021 review in the Journal of Interprofessional Care showed collaborative care reduces hospital readmissions by 23.1% and ER visits by 15.7%. Why? Because side effects were caught early-before they became emergencies.
The Tech That Makes It Work
You can’t collaborate if no one can see what the others are doing.
Real-time access to the same electronic health record is non-negotiable. Systems using HL7 FHIR standards let pharmacists, doctors, and specialists see the same lab results, prescriptions, and allergy alerts at the same time. No more faxed sheets. No more phone tag.
When a patient gets a new prescription from a specialist, the pharmacist gets an alert. If it clashes with an existing drug, they flag it immediately. If the patient hasn’t picked it up, they call. If the dose is too high for kidney function, they suggest a change.
Tools like automated drug interaction checkers and medication reconciliation software cut down manual work. But the magic happens when a pharmacist sees a patient’s full list-12 medications, 4 supplements, 3 OTCs-and says, “You’re taking three drugs that all cause dizziness. Let’s trim this down.”
Community pharmacies now use these same tools. CVS and Walgreens have embedded pharmacists in over 1,200 primary care clinics as of early 2024. They don’t just fill scripts. They manage therapy.
Where It Fails-and Why
It’s not perfect. And it doesn’t work everywhere.
Some doctors still see pharmacists as “pill counters,” not clinicians. A 2021 ASHP survey found 37% of pharmacists reported resistance from physicians who didn’t want to share decision-making. One doctor told a pharmacist, “I don’t need you telling me how to prescribe.” That mindset kills collaboration before it starts.
Reimbursement is another wall. Only 28 states pay Medicaid for pharmacist-led medication reviews. Medicare only started covering some services in 2022. Without payment, clinics can’t afford to hire pharmacists full-time.
Documentation is a nightmare. One Reddit user, ‘MedCheck2023,’ said their team reduced hospital readmissions by 27%-but spent 2.5 hours a day just filling out forms. If the system doesn’t reward efficiency, people burn out.
And scope-of-practice laws vary wildly. In some states, pharmacists can prescribe. In others, they can’t adjust a single dose without a doctor’s signature. That creates chaos in multi-state health systems.
What Success Looks Like in Real Life
Meet Maria, 72. She has atrial fibrillation, osteoarthritis, and depression. She’s on seven medications. She’s confused. She skips doses. She feels tired all the time.
Her primary care doctor referred her to a collaborative clinic. The pharmacist pulled her record, found she was taking two NSAIDs (one prescription, one OTC) that increased her bleeding risk. She was also on a sleep aid that made her dizzy when combined with her blood pressure drug.
The team met. The pharmacist suggested switching one NSAID to acetaminophen, lowering the blood pressure dose, and replacing the sleep aid with a non-drug routine. The doctor agreed. The nurse taught Maria how to use a pill organizer. Two weeks later, her dizziness was gone. Her energy came back. Her INR stabilized.
That’s not a miracle. It’s a process.
Another example: a diabetic patient with foot ulcers. The podiatrist treated the wound. The endocrinologist adjusted insulin. But the pharmacist noticed the patient was taking a statin that was causing muscle pain-so they stopped taking it. Without the statin, their pain improved. But then their cholesterol spiked. The team swapped it for a different statin with fewer side effects. All in one visit.
How to Get Started-Even in a Small Clinic
You don’t need a giant hospital to make this work.
Start small. Invite a local pharmacist to join your weekly huddle. Even 15 minutes a week. Share one high-risk patient. Review their meds. See what gaps appear.
Use free tools. The National Interprofessional Practice and Education Center offers a free online toolkit used by 63% of new teams. It includes templates for collaborative practice agreements, communication scripts, and documentation checklists.
Train your staff. Use SBAR (Situation, Background, Assessment, Recommendation) to structure conversations. Instead of saying, “This patient’s meds look weird,” say: “Situation: Patient had a fall last week. Background: On warfarin, lisinopril, and ibuprofen. Assessment: Ibuprofen increases bleeding risk. Recommendation: Switch to acetaminophen and monitor INR.”
Track results. Count how many side effects you avoid. How many ER visits you prevent. How many patients say they finally understand their meds.
The Future Is Already Here
By 2026, 92% of academic medical centers plan to expand pharmacist roles. CMS is preparing to reimburse pharmacists directly for comprehensive medication management-potentially helping 28 million Medicare beneficiaries.
Side effect management isn’t just about drugs. It’s about communication. Trust. Shared responsibility.
The old model-doctor prescribes, patient takes, side effect happens, repeat-doesn’t work anymore. Patients are complex. Medications are powerful. And the only way to keep them safe is to have the right people talking, together, every single day.
Can pharmacists really adjust medications without a doctor’s approval?
In 48 states, pharmacists can adjust medications under a formal Collaborative Practice Agreement (CPA) signed by a physician. These agreements outline exactly what changes a pharmacist can make-like adjusting warfarin doses, managing diabetes meds, or switching pain relievers. In some states, they can even prescribe. But without a CPA, they can only recommend changes. The key is having the agreement in place before any adjustments happen.
Do I need to hire a full-time pharmacist to see results?
No. Many clinics start with a part-time pharmacist or a shared model. A pharmacist working 20 hours a week can still reduce medication errors by 40% and cut ER visits by 12%. The goal isn’t full-time presence-it’s consistent, structured involvement. Even one weekly medication review session can catch dangerous interactions before they cause harm.
What’s the biggest mistake clinics make when starting collaboration?
Trying to do everything at once. The most common error is launching a full-scale program without a clear scope. Instead, start with one high-risk condition-like anticoagulation or diabetes. Define the roles clearly. Pick one communication tool. Track one outcome, like hospital readmissions. Once that works, expand. Rushing leads to confusion, resistance, and burnout.
How do I get doctors on board if they’re skeptical?
Show them data from their own patients. Track one month of medication-related issues before bringing in a pharmacist. Then track the next month after. The drop in side effects, ER visits, and calls about confusion speaks louder than any lecture. Also, invite them to co-sign the collaborative agreement. Ownership builds trust.
Are these models covered by insurance?
Medicare Part B now covers comprehensive medication management when provided by pharmacists in team-based settings. Medicaid coverage varies by state-only 28 states reimburse as of early 2024. Private insurers are slowly following. Many value-based care contracts now include pharmacist services as a required component to meet quality metrics like medication adherence and hospitalization rates.



Comments (3)
Patrick Merrell
This is exactly why we need to stop treating pharmacists like glorified cashiers. They’re the only ones who actually read the damn script and check for interactions. If your doctor doesn’t listen, find one who does-or better yet, demand your pharmacist be at the table. This isn’t optional anymore.
rasna saha
I work in a small clinic and we started doing weekly med reviews with our part-time pharmacist. Last month, we caught a dangerous combo in a 78-year-old patient that had been going on for 6 months. She was on three drugs that all made her dizzy. We swapped one out and her falls stopped. No drama. Just good teamwork. This works-even if you’re tiny.
James Nicoll
So let me get this straight. We’ve known for a decade that pharmacists prevent disasters, but we still treat them like they’re handing out lollipops at the counter? Meanwhile, doctors are out here prescribing like they’re playing Jenga with a patient’s organs. The system’s not broken-it’s just been designed to fail. And we’re all paying for it in ER bills and grief.