
Quick Takeaways
- SGLT2 inhibitors increase glucose in the urine, creating a sweet environment for bacteria and fungi.
- About 3-5% of users develop genital yeast infections; 2-4% experience a urinary tract infection (UTI).
- Serious infections such as urosepsis or emphysematous pyelonephritis are rare (<0.2%) but can be life‑threatening.
- Good genital hygiene, adequate fluid intake, and early symptom reporting cut the risk dramatically.
- If you have a history of recurrent UTIs or structural urinary problems, discuss alternative drugs with your clinician.
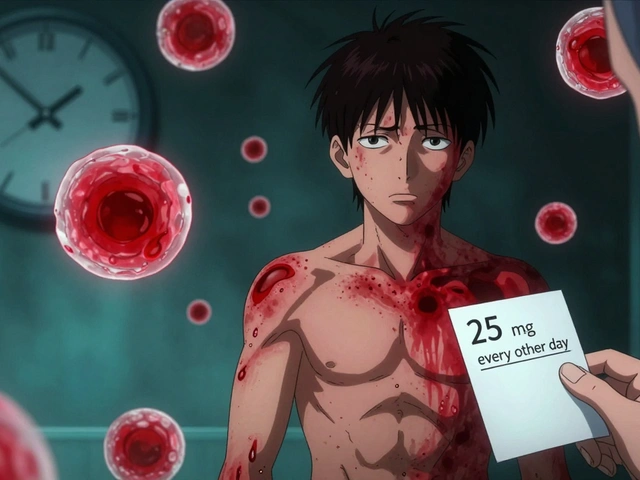
When doctors first rolled out SGLT2 inhibitors are a class of prescription medicines that block the sodium‑glucose cotransporter‑2 protein in the kidney’s proximal tubules. By stopping glucose from being re‑absorbed, they force 40‑110 grams of sugar out in the urine each day, which lowers blood sugar without causing much hypoglycaemia. The trade‑off? That sugary urine also feeds microbes, leading to a noticeable bump in urinary and genital infections.
How the drugs work - and why they invite microbes
Normal kidneys filter glucose and then shove it back into the bloodstream. SGLT2 inhibitors flip that switch off, so glucose spills into the bladder. Think of the bladder as a bathtub filled with sugary water - a perfect breeding ground for Escherichia coli, Candida and other opportunistic organisms.
Four agents dominate the market today:
- Canagliflozin (100 mg or 300 mg daily)
- Dapagliflozin (5 mg or 10 mg daily)
- Empagliflozin (10 mg or 25 mg daily)
- Ertugliflozin (5 mg or 15 mg daily)
All share the same glycosuric effect, though dapagliflozin tends to produce slightly less glucose excretion at the lower dose.
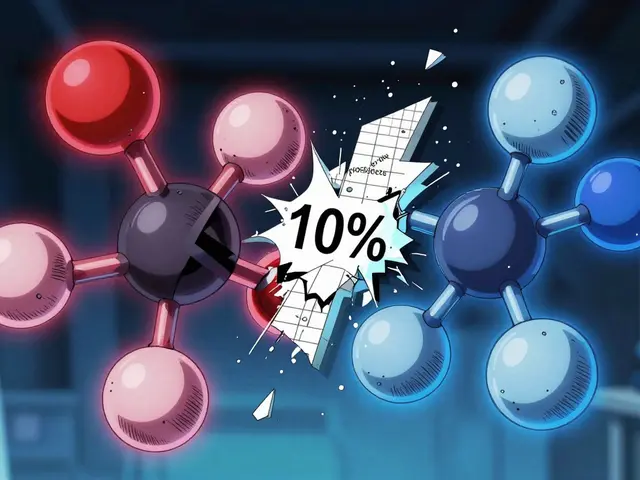
Numbers behind the infections
A 2022 meta‑analysis in *Pharmacology Research & Perspectives* found that users of SGLT2 inhibitors face a 1.78‑fold higher risk of any urinary tract infection compared with DPP‑4 inhibitors, and a 4.57‑fold higher risk of genital fungal infection. In plain terms, for every 100 patients on a comparator drug, an extra 2‑4 people will develop a UTI and about 3‑5 extra people will get a yeast infection.
Serious complications remain uncommon. The FDA’s FAERS review (Mar 2013‑Oct 2014) recorded 19 definite urosepsis cases, with a median onset of 45 days. Only two needed prolonged dialysis, and the overall absolute risk was under 0.1%.
For perspective, here’s a quick risk‑vs‑benefit snapshot:
| Drug class | UTI risk (RR) | Genital fungal infection risk (RR) |
|---|---|---|
| SGLT2 inhibitors | 1.78 | 4.57 |
| DPP‑4 inhibitors | 1.00 | 1.00 |
| Sulfonylureas | 1.72 | 3.82 |
| Thiazolidinediones | 1.71 | 3.78 |

Spotting the warning signs early
Most infections show up within the first three months. Common red flags include:
- Burning or itching around the genital area (often a Candida infection)
- Frequent, cloudy, or foul‑smelling urine
- Painful urination, urgency, or lower‑abdominal discomfort
- Fever above 100.4 °F, chills, or a feeling of being generally unwell
When any of these appear, don’t wait. A prompt clinic visit can prevent escalation to urosepsis or even emphysematous pyelonephritis - a rare gas‑forming kidney infection that has been reported in patients on dapagliflozin.
Practical steps to lower your risk
- Hydrate well. Aim for at least 2 L of water daily; the more you pee, the less time glucose sits in the bladder.
- Keep the area dry. Change underwear daily, use breathable fabrics, and consider a mild, fragrance‑free cleanser.
- Watch your diet. While the drug forces sugar out, limiting excess simple carbs can reduce overall urinary glucose load.
- Consider prophylaxis. Some clinicians advise a daily cranberry capsule; a 2023 FDA safety note cited a 29% reduction in UTIs for SGLT2 users.
- Report symptoms ASAP. Early treatment with a short course of oral antibiotics (for bacterial UTI) or topical azoles (for yeast) works in >90% of cases.
When to think about a different diabetes pill
If you’ve had any of the following, discuss alternatives with your endocrinologist:
- Two or more UTIs in the past year
- Structural urinary issues (e.g., kidney stones, bladder outflow obstruction)
- Immunosuppression or chronic steroid use
- Previous episode of Fournier’s gangrene or emphysematous pyelonephritis
Other drug classes-DPP‑4 inhibitors, GLP‑1 receptor agonists, or even low‑dose sulfonylureas-don’t raise urinary glucose, so they avoid the infection pathway. The trade‑off is often a smaller impact on heart‑failure outcomes or weight loss.
Guidelines from the American Diabetes Association (2023) advise “assessing a history of recurrent UTIs before starting SGLT2 inhibitors and opting for an alternative if risk is high.”
Balancing the benefits
Despite the infection chatter, SGLT2 inhibitors shine in two big areas:
- Cardiovascular protection. Empagliflozin cut major adverse cardiovascular events by 14% in the EMPA‑REG OUTCOME trial (2015). Canagliflozin showed a similar 14% reduction in the CANVAS Program (2017).
- Kidney health. Dapagliflozin continued to slow eGFR decline in the DAPA‑CKD extension (2023), even for patients with stage 3 CKD.
For patients with heart‑failure or chronic kidney disease, the cardiorenal upside often outweighs the modest infection risk-especially when mitigated with the steps above.
What’s on the horizon?
Researchers are tackling the infection problem from two angles:
- Dual SGLT1/2 inhibitors. Early trials suggest they produce less glycosuria, potentially lowering infection rates while keeping heart benefits.
- Risk‑prediction tools. A 2024 *Diabetes Care* study validated a 5‑point score (age > 65, female sex, HbA1c > 8.5%, prior UTI, eGFR < 60) that flags patients with >15% absolute risk of a complicated UTI.
Even with these advances, analysts at GlobalData expect SGLT2 prescriptions to keep rising ~7% a year through 2028, driven by expanding heart‑failure and CKD indications.
Bottom line for patients
Start the drug with a clear plan: stay hydrated, keep the genital area clean, and know the symptoms that demand a doctor’s call. If infection shows up, treat it fast-most issues resolve without dropping the medication. But if infections keep coming back, it’s perfectly reasonable to switch to another class.
Why do SGLT2 inhibitors cause more yeast infections than other diabetes drugs?
The drugs force glucose into the urine, creating a sugary environment that feeds Candida species. Other diabetes medications don’t raise urinary glucose, so the yeast doesn’t get a food source.
How quickly can an infection develop after starting an SGLT2 inhibitor?
Most patients notice symptoms within the first 1‑3 months, but the median time to a serious urosepsis case in FDA data was 45 days.
Can I prevent infections by drinking more water?
Yes. Higher fluid intake dilutes urinary glucose and promotes frequent voiding, which reduces the time bacteria have to grow.
Should I stop the medication if I get a yeast infection?
Usually no. Treat the infection with an antifungal cream or oral medication and continue the SGLT2 inhibitor, unless infections become recurrent or severe.
Are there alternative drugs that don’t raise infection risk?
DPP‑4 inhibitors, GLP‑1 receptor agonists, and some sulfonylureas have a much lower rate of urinary or genital infections. Discuss these options if you have a history of recurrent UTIs.



Comments (13)
Wilson Roberto
Thinking about SGLT2 inhibitors can feel like weighing a scale of benefits versus side‑effects. The glucose that ends up in the urine does create a sweet breeding ground for microbes, but the heart‑protective data are compelling. Staying hydrated and practicing good genital hygiene can blunt the infection risk without sacrificing the cardio‑renal gains. If you notice the first hint of itching or burning, a quick antifungal or antibiotic course usually settles the issue. Remember, the goal is to keep the drug working for you, not to abandon it at the first sign of a nuisance.
Narasimha Murthy
Glycosuria induced by SGLT2 blockade inevitably alters the urinary microenvironment, fostering opportunistic organisms. While the author emphasizes a "modest" infection risk, the raw numbers (3‑5 % for genital candidiasis, 2‑4 % for UTIs) translate into thousands of patients annually when scaled to prescription volumes. Moreover, the cited studies often exclude individuals with baseline urinary tract abnormalities, artificially lowering observed incidence. The argument that hydration mitigates risk overlooks the fact that renal concentrating ability diminishes with age, a demographic that comprises a substantial portion of the SGLT2 user base. The recommendation to treat infections without discontinuing therapy assumes perfect access to antifungal agents, which is not universal in many health‑care settings. Additionally, the author glosses over the psychological burden of recurrent genital irritation, a factor that can erode medication adherence. The safety data also fail to account for the rare but catastrophic Fournier’s gangrene, a condition that, while infrequent, carries a mortality exceeding 30 % when it occurs. The discussion of dual SGLT1/2 inhibitors remains speculative; early-phase trials have not yet demonstrated a meaningful reduction in infection rates compared with established agents. Risk‑prediction tools, such as the 5‑point score referenced, require prospective validation before they can be integrated into routine practice. Furthermore, the emphasis on cardiovascular benefits may distract clinicians from a holistic assessment that includes quality‑of‑life outcomes. In practice, many endocrinologists prescribe SGLT2 inhibitors without thorough screening for prior UTIs, thereby exposing vulnerable patients to preventable complications. The presumption that “most issues resolve without dropping the medication” is an oversimplification that ignores scenarios where recurrent infections necessitate a permanent switch. Finally, the article does not address the cost implications of managing these infections, which can offset the economic advantages of reduced cardiovascular events. In summary, the narrative that infection risk is merely a minor inconvenience does not hold up under rigorous scrutiny, and clinicians should maintain a higher index of suspicion when initiating therapy.
Samantha Vondrum
Colleagues, let us approach this topic with both scientific rigor and compassionate guidance. 🩺 The mechanistic link between increased urinary glucose and Candida overgrowth is well‑documented, and acknowledging it allows us to empower patients with practical preventative measures. Consistent water intake, routine genital cleansing, and prompt reporting of early symptoms are cornerstone strategies that complement pharmacotherapy. It is equally important to frame the conversation around shared decision‑making, especially when patients have a history of recurrent UTIs. By offering alternatives such as DPP‑4 inhibitors or GLP‑1 agonists in a respectful manner, we uphold the principle of individualized care. I encourage all providers to incorporate these nuanced discussions into routine visits, thereby fostering adherence and minimizing adverse events. 🌟
Kelvin Egbuzie
Oh sure, just drink an ocean of water and the bugs will magically disappear – as if pharma didn’t design these pills to turn our bladders into sugar farms. ;) The "cardio‑renal" hype conveniently hides the fact that manufacturers have a vested interest in downplaying the infection data. If you really think a simple lifestyle tweak can outrun a drug‑induced metabolic shift, you’re dreaming. And don’t get me started on the “rare” Fournier’s gangrene – rare for the study sponsors, terrifying for the patient.
Katherine Collins
i dun think thse meds are worth the risk lol 😜 keep an eye on it but dont stress too much.
Taylor Nation
Totally get the concern, but let’s keep the conversation pragmatic. Staying on the drug while using a quick course of antifungal often solves the problem without sacrificing the heart‑benefit. If infections become a pattern – two or more UTIs in a year – that’s the moment to flag a medication review with your endocrinologist. It’s all about balancing risk and reward, and the data still show a net positive impact for most patients.
Nathan S. Han
Hear me out: the drama of a yeast infection can feel overwhelming, yet the clinical evidence paints a far more measured picture. When you look at absolute numbers, the infection rate is modest compared to the profound reduction in cardiovascular mortality demonstrated across multiple trials. Think of the drug as a double‑edged sword – one edge cuts away heart attacks, the other occasionally pricks the skin in a predictable way. The key is diligent monitoring, patient education, and swift intervention at the first sign of discomfort. In the grand narrative of diabetes management, SGLT2 inhibitors often emerge as starring protagonists rather than villains.
Ed Mahoney
Yep, just an infection.
Brian Klepacki
Behold, the saga of a molecule that promises to rescue the heart while courting the yeast! One cannot help but admire the audacity of a drug that, in its quest for renal preservation, throws a sugary banquet for opportunistic fungi. Yet the clinical theater is not without its critics; the audience watches as researchers unveil dual‑inhibitors hoping to silence the microbial chorus. Whether this will rewrite the script or merely add a footnote remains to be seen, but the drama is undeniably captivating.
Shermaine Davis
i think its a good med but watch out for the itch. use creams fast. dont quit unless many times.
Selina M
hey all, just a heads up – stay hydrated, keep clean, and if you feel weird go to your doc fast. no need to freak out but do act quick.
tatiana anadrade paguay
It’s encouraging to see the emphasis on patient education. Providing clear guidance on hydration, hygiene, and symptom monitoring helps patients feel in control while preserving the therapeutic benefits of SGLT2 inhibitors.
Nicholai Battistino
Well articulated. Concise point‑by‑point summary is appreciated.