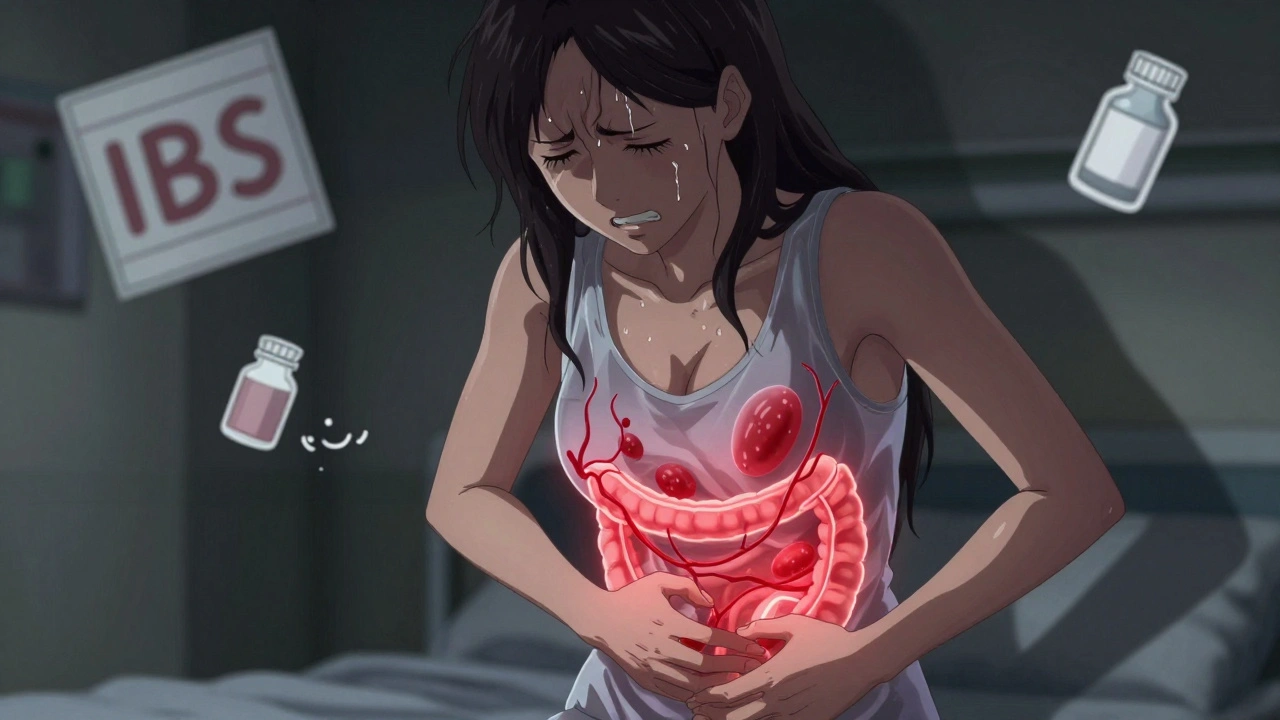
Severe stomach pain that comes and goes with your period isn’t just bad luck-it could be endometriosis. Many women assume their cramps are normal, or blame it on food poisoning or stress. But if your pain is so bad you can’t stand up, throw up, or go to work, and it keeps coming back every month, you’re not imagining it. Endometriosis doesn’t just affect the uterus. It can grow on the bowel, bladder, and even the lining of your stomach, causing pain that feels like it’s coming from your gut.
Why endometriosis mimics digestive problems
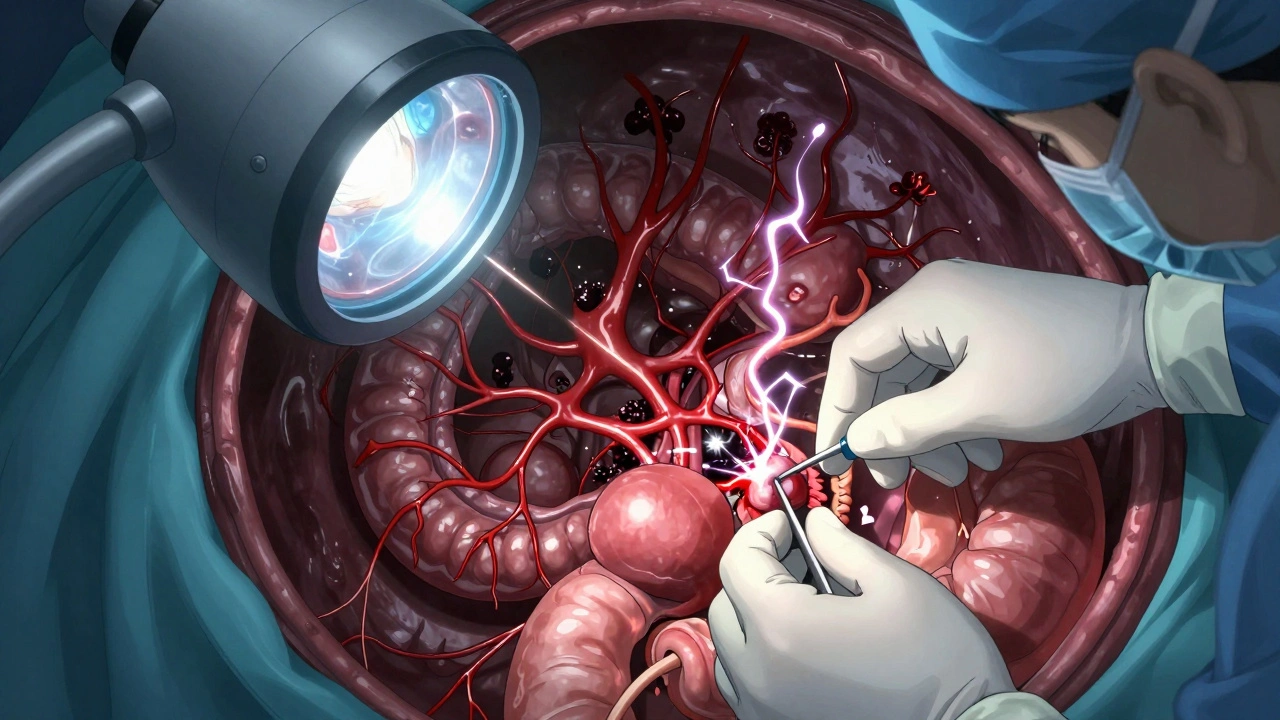
Endometriosis happens when tissue similar to the lining of the uterus grows outside the womb. These implants bleed and swell during your cycle, just like the uterine lining. But when they land on the intestines, colon, or stomach, your body treats them like invaders. That triggers inflammation, scar tissue, and nerve irritation-all of which cause sharp, cramping, or burning pain in the abdomen.
That’s why so many people with endometriosis go to the doctor thinking they have IBS, Crohn’s, or a stomach bug. They get tested for food allergies, take antacids, or get prescribed laxatives. Nothing helps. The real problem? The tissue growing on their bowel isn’t being seen. A 2023 study in Human Reproduction found that nearly 40% of women with severe abdominal pain and endometriosis were misdiagnosed with gastrointestinal disorders first.
Signs your stomach pain might be endometriosis
Not all stomach pain is endometriosis. But if you notice these patterns, it’s worth asking your doctor:
- Pain that spikes right before or during your period and fades after
- Bloating so bad you look 6 months pregnant, especially around your cycle
- Diarrhea, constipation, or painful bowel movements that match your menstrual timing
- Nausea or vomiting during your period that doesn’t happen at other times
- Pain during or after sex that feels deep in your pelvis or lower belly
These aren’t random symptoms. They’re signals. Endometriosis implants on the bowel can cause the muscle walls to stiffen, making it hard to pass stool. When they grow near nerves in the lower abdomen, they send pain signals that your brain interprets as coming from your stomach. It’s not a coincidence-it’s anatomy.
Where the pain actually comes from
Think of your pelvis as a crowded room. The uterus sits in the middle. Around it are the bladder, rectum, sigmoid colon, and parts of the small intestine. Endometriosis doesn’t care about boundaries. It can attach to any surface it finds. When it grows on the rectosigmoid colon (the last part of the large intestine), it can cause pain during bowel movements. When it wraps around the stomach’s outer lining, it can trigger nausea and early fullness after eating.
Some women report a feeling like something is “pulling” inside their lower belly. Others say it feels like a knife stabbing them when they move or breathe deeply. That’s not gas. That’s endometrial tissue pulling on nerves or sticking organs together with scar tissue. In advanced cases, the bowel can become partially blocked, leading to vomiting and severe constipation.
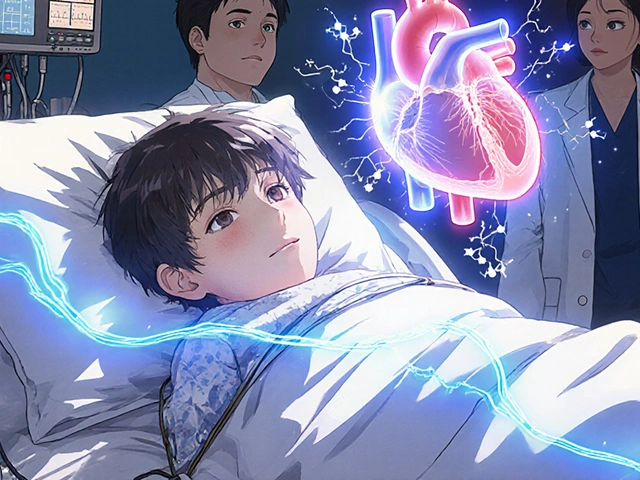
Why diagnosis takes years
The average time to diagnose endometriosis is 7 to 10 years. Why? Because doctors still think of it as a “period pain” issue, not a systemic disease. Ultrasounds often miss it. Blood tests don’t detect it. The only way to confirm it is through laparoscopic surgery-where a camera is inserted to see the lesions.
Many women are told to take birth control, “just live with it,” or see a gastroenterologist. But if your pain follows your cycle, no GI treatment will fix it. You need a specialist who knows endometriosis can hide in plain sight-inside your abdomen, not just your uterus.
What to do if you suspect endometriosis
If you’ve had severe stomach pain for months or years, especially if it lines up with your period, here’s what to do:
- Track your symptoms for at least two cycles. Note the day, intensity, and what you were doing when the pain hit.
- Bring your symptom log to a gynecologist who specializes in endometriosis-not just any OB-GYN.
- Ask for a pelvic ultrasound, but know it won’t show everything. Deep infiltrating endometriosis often needs an MRI.
- Request a referral to a surgeon trained in excision surgery. This is the gold standard for removing endometriosis tissue completely.
- Don’t accept pain as normal. If your doctor says, “It’s just cramps,” get a second opinion.
There’s no cure for endometriosis, but it can be managed. Excision surgery removes the tissue, and many women see their stomach pain drop by 70% or more afterward. Hormone treatments can help slow growth, but they don’t remove existing lesions.

What doesn’t work-and what does
Many people try diet changes, probiotics, or elimination diets hoping to fix endometriosis pain. These can help with bloating or IBS-like symptoms, but they won’t touch the root cause. If the tissue is growing on your bowel, no amount of gluten-free eating will make it disappear.
What does help? Surgery to remove the lesions. Physical therapy for pelvic floor tension. And support groups-because no one should feel alone while suffering in silence.
One patient from Halifax, 32, had been told she had IBS for five years. Her pain was so bad she skipped family dinners. After a pelvic MRI and laparoscopy, surgeons found endometriosis on her sigmoid colon and bladder. After excision surgery, her stomach pain vanished. She didn’t need to change her diet. She just needed the right diagnosis.
When to seek help right away
Severe stomach pain with endometriosis is usually cyclical. But if you experience:
- Sudden, sharp pain that doesn’t match your cycle
- Fever, chills, or vomiting with abdominal pain
- Inability to pass stool or gas for more than 48 hours
- Blood in stool or vomit
-go to the emergency room. These could be signs of bowel obstruction or rupture, which are rare but serious complications.
Living with it-without letting it control you
Endometriosis doesn’t have to define your life. But it does require you to become your own advocate. Keep records. Find a specialist. Ask for imaging. Push for answers. You’re not overreacting. Your pain is real, and it’s treatable.
There are support networks in Halifax and across Canada. Organizations like Endometriosis Canada offer free resources, doctor directories, and peer mentoring. You don’t have to figure this out alone.
Can endometriosis cause stomach pain without period cramps?
Yes. While most people link endometriosis pain to their period, some have pain that’s constant or triggered by eating, bowel movements, or sex. This usually happens when lesions are on the bowel, bladder, or nerves near the stomach. The pain may not feel like cramps-it can be burning, stabbing, or pressure.
Is endometriosis the same as IBS?
No. IBS is a functional disorder of the gut with no visible tissue damage. Endometriosis involves actual growth of tissue outside the uterus that causes inflammation and scarring. The symptoms can overlap-bloating, diarrhea, constipation-but endometriosis pain follows your menstrual cycle and often includes pelvic pain, painful sex, or infertility. IBS doesn’t cause those.
Can birth control fix endometriosis stomach pain?
Birth control can reduce the bleeding and swelling of endometriosis lesions, which may ease pain for some. But it doesn’t remove the tissue. Many women find their stomach pain returns or worsens after stopping the pill. Birth control masks symptoms-it doesn’t treat the cause.
Why do ultrasounds often miss endometriosis?
Standard pelvic ultrasounds are great for looking at the uterus and ovaries, but they can’t see deep lesions on the bowel, bladder, or abdominal lining. These are often hidden behind gas or other organs. Only specialized transvaginal ultrasounds by trained technicians, or an MRI, can detect deeper endometriosis. Laparoscopy remains the only definitive diagnostic tool.
Does endometriosis get worse with age?
It can. Without treatment, endometriosis lesions can grow, spread, and form more scar tissue over time. That’s why early diagnosis matters. After menopause, symptoms often improve due to lower estrogen levels, but not always-especially if you’re on hormone therapy. The damage done to organs can be permanent if left untreated for years.


Comments (15)
Jessica Baydowicz
I used to think my monthly stomach explosions were just bad tacos-turns out, I had endometriosis gnawing on my colon. No joke. Took me seven years, three ER visits, and a doctor who actually listened. Now I’m pain-free after surgery. You’re not crazy. Your pain is real.
Martyn Stuart
Thank you for this. As someone who’s been through it, I can’t stress enough: don’t settle for ‘it’s just IBS.’ I was prescribed loperamide for two years while my bowel was literally being glued shut by endometrial tissue. The moment I found a specialist who did excision surgery? My life changed. You don’t need to suffer silently-advocate, document, insist.
val kendra
same. i went to 5 docs before one said ‘maybe its endo’ and i cried because no one had ever believed me. now i have a scar and a new lease on life. dont let them gaslight you.
Ben Choy
Just had my third laparoscopy last month. Still healing, but the pain’s down 80%. I used to cancel plans every month like clockwork. Now I’m hiking again. It’s not a miracle-it’s medicine. Find a surgeon who knows what they’re doing. Google ‘excision specialist’ and don’t stop until you find one.
Karl Barrett
The epistemological crisis here is systemic: medical paradigms still prioritize reproductive health as a subset of gynecology rather than an integrated bio-psycho-social condition. Endometriosis is not a ‘women’s issue’-it’s a neuroinflammatory disorder with visceral manifestations that are systematically underdiagnosed due to gendered bias in clinical reasoning. The 7-year diagnostic delay isn’t an anomaly-it’s a feature of patriarchal medicine.
Jake Deeds
Ugh. I’m so tired of women being told their pain is ‘all in their head.’ My sister waited 9 years. She had to miss her daughter’s first steps because she was curled up on the bathroom floor. And the doctor? Said she ‘needed to relax more.’ Like that’s the solution. If this were a man with colon cancer, they’d be scanning him within hours. Double standard. And it’s disgusting.
George Graham
I’m a guy, and I didn’t even know this could happen outside the uterus. My partner had been suffering for years, and I thought she was just ‘having a bad cycle.’ I’m so sorry I didn’t push harder. This post helped me understand what she’s been through. Thank you for the clarity. I’m helping her find a specialist this week.
John Filby
My cousin had this and no one believed her until she showed them her symptom tracker. She had a whole spreadsheet: pain level, food, bowel movement, mood. When she brought it in, the doctor’s face changed. I’m telling everyone now. Track everything. It’s your superpower.
Elizabeth Crutchfield
i had endo on my bladder and no one believed me. they said i was just drinking too much coffee. i cried in the parking lot after the appointment. 3 years later i had surgery and now i can pee without screaming. please believe women.
Yasmine Hajar
Okay but can we talk about how the medical system is literally designed to ignore women’s pain? I’ve been told I’m ‘too emotional,’ ‘too dramatic,’ ‘just stressed.’ I had to record my pain on video and send it to my doctor before they’d even consider an MRI. And guess what? It was endometriosis on my bowel. I’m not mad-I’m motivated. Now I run a support group. You’re not alone. We’re here.
Emmanuel Peter
Wait, so you’re saying if you have stomach pain during your period, it’s not food poisoning? That’s wild. I thought everyone just had bad cramps. Maybe I should stop blaming my burritos. But seriously, how do you even know it’s endo and not just… bad luck? Like, what’s the science behind this? I’m just asking.
Ashley Elliott
I’m a nurse. I’ve seen this over and over. Women come in with textbook symptoms, and the first thing they’re given is a prescription for ibuprofen and a ‘try yoga’ pamphlet. It’s heartbreaking. If you’re reading this and you’ve been dismissed-keep going. Bring the article. Print it. Show it. You deserve care. You’re not exaggerating.
Chad Handy
I’ve had this since I was 14. I’m 34 now. I’ve had three surgeries, two failed IVF cycles, lost jobs because I couldn’t get out of bed, and my husband left me because he said ‘you’re always in pain.’ I’m not bitter-I’m just tired. I don’t want sympathy. I want someone to fix this. I don’t care if it’s surgery, pills, or aliens. Just make it stop. And don’t tell me to ‘eat clean.’ I’ve tried everything. I’ve tried everything.
Augusta Barlow
Okay but what if this is all just a big pharmaceutical scam? Like, what if they’re making money off of unnecessary surgeries? I read online that endometriosis is overdiagnosed because doctors want to sell laparoscopies. And what about the hormone treatments? Are they really safe? I’m not saying it’s not real-I’m just saying… maybe we’re being manipulated. Like, why is there no ‘cure’? Hmm.
Shofner Lehto
My daughter was diagnosed at 19. She’s now in med school. She wants to be a gynecologic surgeon so no one else has to wait a decade like she did. This isn’t just about pain-it’s about changing the system. The fact that we still don’t have non-invasive diagnostics is a scandal. We need more funding, more research, and more doctors who listen. This post is a step forward.