
Imagine looking at a street sign, but the letters keep blurring and doubling. You try glasses, but they don’t help. This is the reality for many people with keratoconus, a condition where the cornea-the clear front surface of the eye-gradually thins and bulges outward into a cone shape. It doesn’t happen overnight. It starts in the teens or early 20s, often going unnoticed until vision becomes noticeably blurry or distorted. By the time most people get diagnosed, the cornea has already changed structure, and regular glasses simply can’t fix it. That’s where rigid lenses come in-not as a cure, but as the most reliable way to restore clear vision without surgery.
What Exactly Happens in Keratoconus?
Keratoconus isn’t just blurry vision. It’s a structural breakdown. The cornea, which normally stays smooth and dome-shaped, starts to weaken. Enzymes in the eye break down collagen fibers faster than the body can rebuild them. This causes the cornea to thin, especially in the center or lower part, and bulge forward like a cone. The result? Light entering the eye bends unevenly, creating distorted images, glare, double vision, and increased sensitivity to light. This isn’t random. It’s progressive. Most people notice worsening vision over 5 to 10 years, usually slowing down by their 40s. It affects both eyes, but often unevenly-one eye might be much worse than the other. Corneal topography scans show this clearly: the central cornea becomes steeper, while the edges stay normal. That’s why glasses fail. They’re designed for even curvature. When the surface is irregular, the only way to create a smooth optical surface is with a rigid lens that sits on top of the cornea like a new, perfectly shaped lens.Why Rigid Lenses Work When Glasses Don’t
Regular eyeglasses sit far from the eye. They can’t compensate for the uneven shape of a keratoconus cornea. Rigid lenses, on the other hand, rest directly on the eye. Because they’re stiff, they don’t conform to the cornea’s irregular shape. Instead, they create a new, smooth surface in front of it. The space between the lens and the cornea fills with tears, which act as a liquid buffer. This tear layer smooths out the bumps and dips in the cornea, letting light focus properly on the retina. This isn’t theory-it’s measurable. Studies show patients with moderate keratoconus go from seeing only 20/400 with glasses to 20/200 or better with rigid lenses. For many, that’s the difference between driving legally and not being able to read a license plate. Some even reach 20/25 after full adaptation. That’s near-perfect vision without surgery. There are three main types of rigid lenses used for keratoconus:- Rigid Gas Permeable (RGP) lenses: These are the most common starting point. They’re small, about 9-10mm wide, and made of oxygen-permeable plastic. Their Dk values range from 50 to 150, meaning they let enough oxygen through to keep the cornea healthy during daily wear.
- Hybrid lenses: These combine a rigid center (for clear vision) with a soft outer skirt (for comfort). They’re a good middle ground for people who find RGPs too uncomfortable.
- Scleral lenses: These are larger-15 to 22mm in diameter. They vault over the entire cornea and rest on the white part of the eye (the sclera). They create a fluid reservoir that cushions the cornea, making them ideal for advanced cases with scarring or extreme irregularity.
How Scleral Lenses Changed the Game
Ten years ago, people with advanced keratoconus had few options: endure blurry vision or get a corneal transplant. Today, scleral lenses are often the first choice for stage III or IV keratoconus. Why? Because they don’t touch the damaged cornea at all. The lens floats above it, held in place by the sclera, with a layer of saline solution underneath. This fluid reservoir not only improves vision-it also protects the cornea from rubbing, reduces dryness, and can even help heal minor surface damage. In clinical settings, scleral lenses have an 85% success rate in advanced cases, compared to just 65% for traditional RGPs. That’s a big difference when you’re struggling to see your child’s face across the room. And they’re not just for extreme cases. Many patients who couldn’t tolerate RGPs due to discomfort switch to scleral lenses and suddenly find they can wear contacts all day without pain. Recent advances in materials have made them even better. New scleral lenses introduced in 2022 have oxygen permeability ratings above Dk 200-higher than most RGPs. This means less risk of corneal swelling, even with long wear. In January 2023, the FDA approved the first digital manufacturing process for fully customized scleral lenses. Now, instead of guessing lens curves based on standard templates, optometrists use 3D corneal scans to design lenses that match the exact shape of each patient’s eye. This level of precision wasn’t possible five years ago.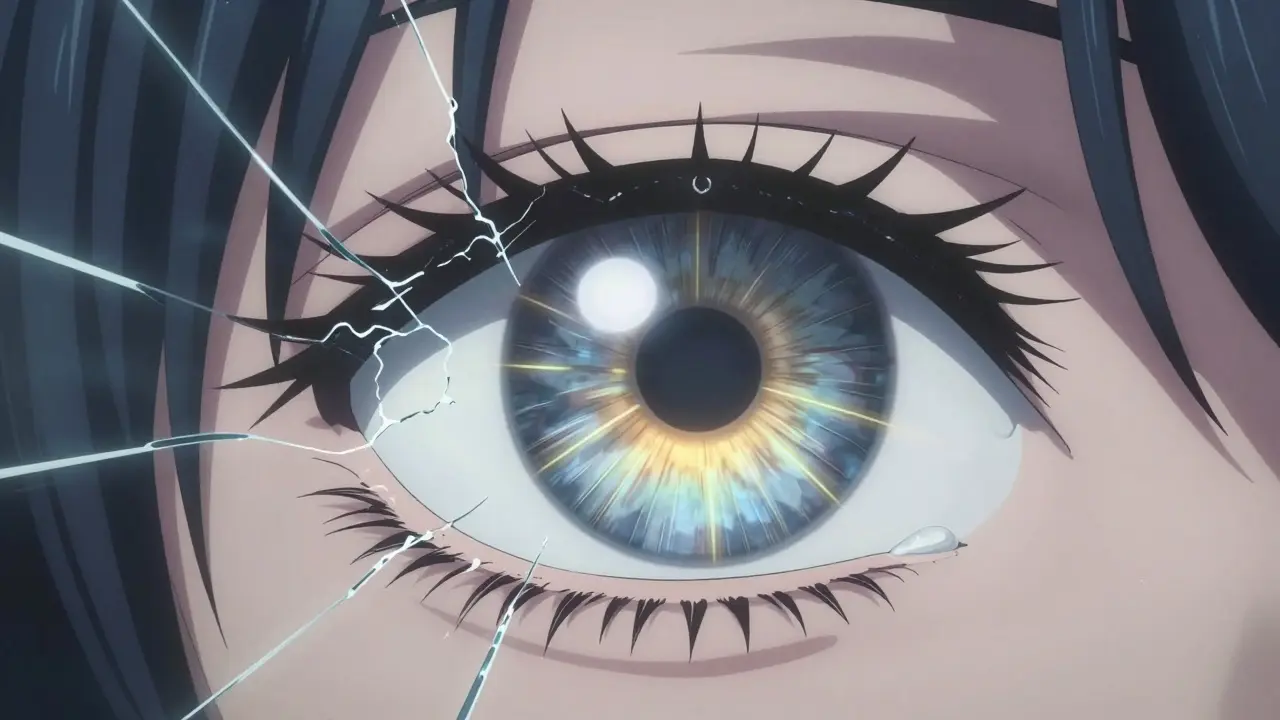
What About Other Treatments?
Rigid lenses aren’t the only option, but they’re the most widely used. Other treatments serve different purposes:- Corneal cross-linking (CXL): This is the only treatment proven to stop keratoconus from getting worse. It uses UV light and riboflavin to strengthen collagen bonds in the cornea. Success rates are 90-95% at five years. But here’s the catch: CXL doesn’t improve vision. It just stops decline. You still need rigid lenses afterward to see clearly.
- INTACS: These are tiny plastic rings inserted into the cornea to flatten its shape. They’re FDA-approved since 1999 and help in some cases. But even after implantation, 35-40% of patients still need rigid lenses to get good vision.
- Corneal transplant: This is the last resort. About 10-20% of keratoconus patients eventually need it, usually because lenses no longer fit or the cornea is scarred. But transplants come with risks-5-10% chance of rejection, and it can take over a year to stabilize vision. Recovery is long, expensive, and unpredictable.
What to Expect When You Start Wearing Rigid Lenses
Getting fitted isn’t a one-time visit. It’s a process. You’ll need 3-5 appointments over 4-6 weeks. The optometrist will use a corneal topographer to map your eye, then try different lens designs. Each lens is tested for fit, movement, and vision clarity. It’s not like picking off-the-shelf contacts. Adaptation takes time. Most people start with just 2-4 hours of wear per day, adding an hour or two each day. Full-time wear usually takes 2-4 weeks. During this period, you might feel:- A foreign body sensation (45% of new wearers)
- Lens awareness (38%)
- Difficulty inserting or removing the lens (32%)
Who Doesn’t Do Well With Rigid Lenses?
Not everyone succeeds. About 15-25% of patients can’t tolerate rigid lenses, especially in advanced stages. Common reasons:- Extreme corneal scarring that prevents proper lens centration
- Chronic dry eye that makes lens wear painful
- Severe sensitivity to lens solutions
Is This the Future of Keratoconus Care?
Yes. The global market for specialty contact lenses-mostly for keratoconus-is projected to grow from $1.85 billion in 2022 to $2.78 billion by 2027. Why? Because rigid lenses keep getting better. New materials, digital design, and better fitting protocols mean more people can wear them comfortably. And as awareness grows, more teenagers are being diagnosed early-before vision gets too bad. The future isn’t about replacing rigid lenses. It’s about combining them smarter. CXL to stop the disease. Custom scleral lenses to restore vision. And regular check-ups to catch changes before they become problems. For most people with keratoconus, this is the best path forward: no surgery, no overnight fix, but a reliable, life-changing way to see clearly every day.What Happens If You Ignore It?
Keratoconus doesn’t just fade away. Left untreated, it keeps progressing. Vision gets worse. Glasses become useless. You might start avoiding driving at night because of glare. Reading becomes a chore. You might stop doing things you love because you can’t see well enough. Worse, if you wait too long, the cornea can develop permanent scarring. Once that happens, rigid lenses often won’t fit properly anymore. Your options shrink. Surgery becomes more likely. And recovery from a transplant is long, risky, and expensive. The earlier you get diagnosed and start treatment, the better your outcome. If you’re in your teens or 20s and notice blurry vision that doesn’t improve with glasses, get a corneal topography scan. It takes 10 minutes. It could change your life.Can glasses fix keratoconus?
No. Glasses cannot correct the irregular shape of a keratoconus cornea. They work for simple nearsightedness or astigmatism with even curvature, but keratoconus creates a cone-shaped distortion that glasses can’t compensate for. Rigid contact lenses are needed to create a smooth optical surface over the irregular cornea.
Are scleral lenses better than RGP lenses for keratoconus?
For advanced cases (stage III or IV), yes. Scleral lenses have an 85% success rate in these cases, compared to 65% for RGP lenses. They’re more comfortable, don’t touch the damaged cornea, and provide better vision stability. For early or mild cases, RGP lenses are often the first choice because they’re smaller, easier to handle, and less expensive.
Does wearing rigid lenses stop keratoconus from getting worse?
No. Rigid lenses improve vision but don’t treat the underlying cause. To stop progression, you need corneal cross-linking (CXL), which strengthens the cornea’s collagen fibers. Most eye doctors now recommend combining CXL with rigid lenses for both vision correction and disease control.
How long does it take to get used to rigid lenses?
Most people adapt within 2 to 4 weeks. Start with 2-4 hours of wear per day and increase by 1-2 hours daily. Initial discomfort, like a foreign body sensation or lens awareness, is normal. About 85% of patients achieve full-time comfortable wear after this adaptation period.
Can keratoconus be cured?
There is no cure for keratoconus. But it can be effectively managed. Corneal cross-linking stops progression in 90-95% of cases, and rigid lenses restore clear vision in most patients. Only 10-20% of people eventually need a corneal transplant. With proper care, many live full lives without significant vision loss.
Is keratoconus common?
Yes. About 1 in 2,000 people worldwide have keratoconus. It’s more common than many realize, especially in teens and young adults. Diagnosis rates are rising as screening tools like corneal topography become more widely available in eye clinics.
Comments (10)
Diana Stoyanova
Okay, but have you ever tried putting in rigid lenses after a 12-hour shift? I’m not kidding-it’s like trying to thread a needle while someone’s poking your eyeball. I went from 20/400 to 20/20 in 6 weeks, but man, the first month felt like I was living inside a lava lamp. The tears? The weird blinking reflex? The way your eyelid just *slaps* the lens when you yawn? Yeah. Worth it. Now I can see my cat’s whiskers. And that’s a miracle.
Gregory Clayton
Ugh, I hate how this whole thing gets marketed like some miracle cure. Meanwhile, my cousin in Ohio got a corneal transplant because these fancy lenses kept scratching his cornea. And now he’s on immunosuppressants for life. Who’s paying for all this? Insurance? You think the eye doctors are doing this because they care? Nah. They’re making bank off the ‘lens treadmill.’ Just sayin’.
Catherine Scutt
People who say ‘just wear scleral lenses’ clearly haven’t tried to clean them. I used to do it every night like clockwork-10 minutes of saline, 5 minutes of scrubbing, 15 minutes of rinsing. Then I realized I was spending more time on my contacts than on my relationships. And I still got fungal keratitis. So no. Not worth it. Glasses are embarrassing. But at least I can blink without crying.
Darren McGuff
As a contact lens fitter for 22 years, I’ve seen this evolution firsthand. In 2010, we’d fit 3 patients a month with RGPs. Now? 12 a week. The real game-changer wasn’t the lens-it was the digital mapping. We used to guess corneal curvature with trial lenses. Now? We scan, design, print, fit-all in one day. I’ve had teens cry because they saw their own reflection clearly for the first time. That’s not tech. That’s magic.
Alicia Hasö
To anyone reading this who’s terrified of starting rigid lenses: you’re not broken. You’re just in the wrong stage of the journey. I’ve worked with over 400 keratoconus patients. The ones who succeed? They don’t push through pain. They listen. They track their symptoms. They ask for adjustments. And they never, ever skip their follow-ups. This isn’t about toughness-it’s about partnership with your eye care team. You’re not alone. And your vision matters.
Ashley Kronenwetter
It’s important to clarify that corneal cross-linking is not a vision-enhancing procedure. It is a structural stabilization technique. Rigid lenses remain the primary modality for visual rehabilitation. The combination of CXL and customized contact lenses represents the current standard of care, supported by peer-reviewed literature and clinical guidelines from the American Academy of Ophthalmology. Please consult a corneal specialist before making treatment decisions.
Aron Veldhuizen
Let’s be brutally honest: if rigid lenses were so effective, why do 25% of patients still end up with transplants? And why is the industry pushing ‘custom digital lenses’ like they’re the Holy Grail? Because they’re expensive. And because the real problem isn’t the cornea-it’s the profit model. The system is designed to keep you dependent on $500 lenses every 6 months, not to cure you. Cross-linking? Great. But why isn’t there funding for regenerative therapies? Because it doesn’t pay as well.
Micheal Murdoch
I’ve been wearing scleral lenses for 8 years now. I was diagnosed at 19. I thought my life was over. Now I’m a teacher. I read to my students. I drive. I even hiked the Grand Canyon last summer. The first year was hell-foggy lenses, dry eyes, one time I dropped one in a toilet (yes, really). But here’s the thing: every single person who told me ‘you’ll never wear contacts again’ was wrong. It’s not easy. But it’s possible. And if you’re reading this and you’re scared? I’m here. Message me. I’ll walk you through it. You’ve got this.
Drew Pearlman
Just want to say-this post gave me chills. I’m 23, got diagnosed last year, and I was ready to give up. I thought I’d be blind by 30. But after my first scleral fitting? I saw my mom’s face. Not blurry. Not fuzzy. CLEAR. Like, I could count the freckles on her nose. I cried in the chair. And now I wear them 14 hours a day. It’s not perfect. But it’s enough. To everyone else out there: don’t give up. There’s light. Even if you have to wear it on your eye.
Lindsey Wellmann
😭 I just got my first pair of sclerals today. I saw my dog’s nose. His nose. I’ve never seen his nose before. 🤯 I’m crying. Again. This is the most emotional thing I’ve ever experienced. Thank you, science. Thank you, optometrist. Thank you, tears. 🙏💧👁️🗨️