
If you have discoid or systemic lupus erythematosus, you’re not just managing rashes, joint pain, and fatigue-you might also be quietly losing bone density. Osteoporosis doesn’t come with warning signs until a bone breaks. And for people with lupus, that risk is 2 to 5 times higher than in the general population. This isn’t a side effect you can ignore. It’s a direct consequence of the disease itself, the medications used to treat it, and the lifestyle changes it forces on you.
What’s the Link Between Lupus and Bone Loss?
Lupus doesn’t just attack skin and joints-it triggers chronic inflammation. That inflammation doesn’t stay local. It floods your bloodstream with cytokines like TNF-alpha and IL-6, which directly interfere with how your bones rebuild themselves. Your body normally balances bone breakdown and bone formation. In lupus, the scales tip hard toward breakdown. Studies show that even early-stage lupus patients have lower bone mineral density than healthy peers of the same age and sex.
Discoid lupus, which mostly affects the skin, still carries this risk-even if internal organs aren’t involved. Why? Because the same immune overactivity that causes scaly, circular rashes on the face or scalp also sends inflammatory signals through the body. Systemic lupus erythematosus (SLE) is worse. When kidneys, heart, or blood vessels are involved, the inflammation is more intense and widespread. That means faster bone loss.
Medications That Weaken Bones
Glucocorticoids like prednisone are the go-to treatment for flare-ups in both discoid and systemic lupus. They work fast. But they’re also one of the leading causes of drug-induced osteoporosis. Taking just 5 mg of prednisone daily for three months can cut bone density by 5-10%. After a year, the risk of spine or hip fracture doubles.
How? Corticosteroids shut down bone-building cells called osteoblasts. They also ramp up bone-eating cells called osteoclasts. On top of that, they reduce calcium absorption in your gut and increase calcium loss through your kidneys. It’s a triple hit on your skeleton.
Some lupus patients take hydroxychloroquine long-term to control symptoms. While this drug helps protect bones by reducing inflammation, it doesn’t cancel out the damage from steroids. And if you’re on both, the bone loss keeps creeping up.
Who’s Most at Risk?
Not everyone with lupus gets osteoporosis-but certain patterns make it much more likely:
- Women over 50 with lupus-especially postmenopausal-are at the highest risk. Estrogen loss plus lupus inflammation is a dangerous combo.
- People who’ve been on steroids for more than 3 months, even at low doses.
- Those with kidney involvement. Lupus nephritis reduces vitamin D activation, which is critical for calcium uptake.
- People who avoid the sun due to photosensitivity. Sunlight is your body’s main source of vitamin D. Less sun = less vitamin D = weaker bones.
- Those with low physical activity. Joint pain and fatigue make movement hard, but inactivity accelerates bone loss.
A 2023 study tracking 1,200 lupus patients over five years found that 38% developed osteoporosis. Of those, 62% had taken daily steroids for over a year. The average bone density drop was 12% in the spine and 9% in the hip.

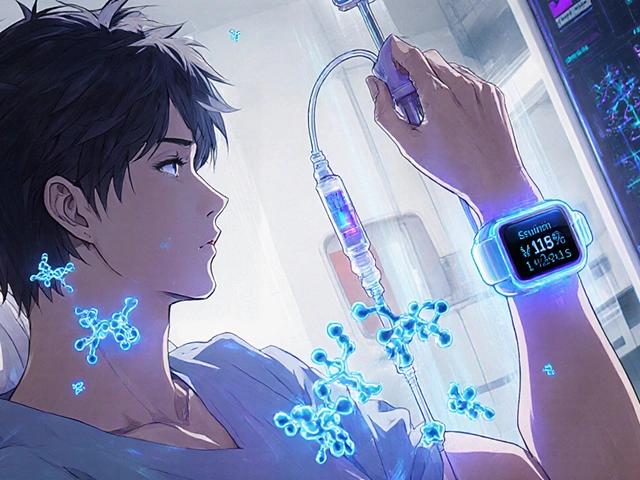
How to Test for Bone Loss
Don’t wait for a fracture. Get a DEXA scan-a simple, painless X-ray that measures bone density. The American College of Rheumatology recommends it for all lupus patients who:
- Are over 50
- Have taken steroids for more than 3 months
- Have had a low-trauma fracture (like breaking a wrist from a minor fall)
- Have kidney disease or low vitamin D levels
Results are given as a T-score:
- -1.0 or higher: normal bone density
- -1.1 to -2.4: osteopenia (low bone mass)
- -2.5 or lower: osteoporosis
If you’re in the osteopenia range, it’s not a death sentence-but it is a red flag. You need to act now.
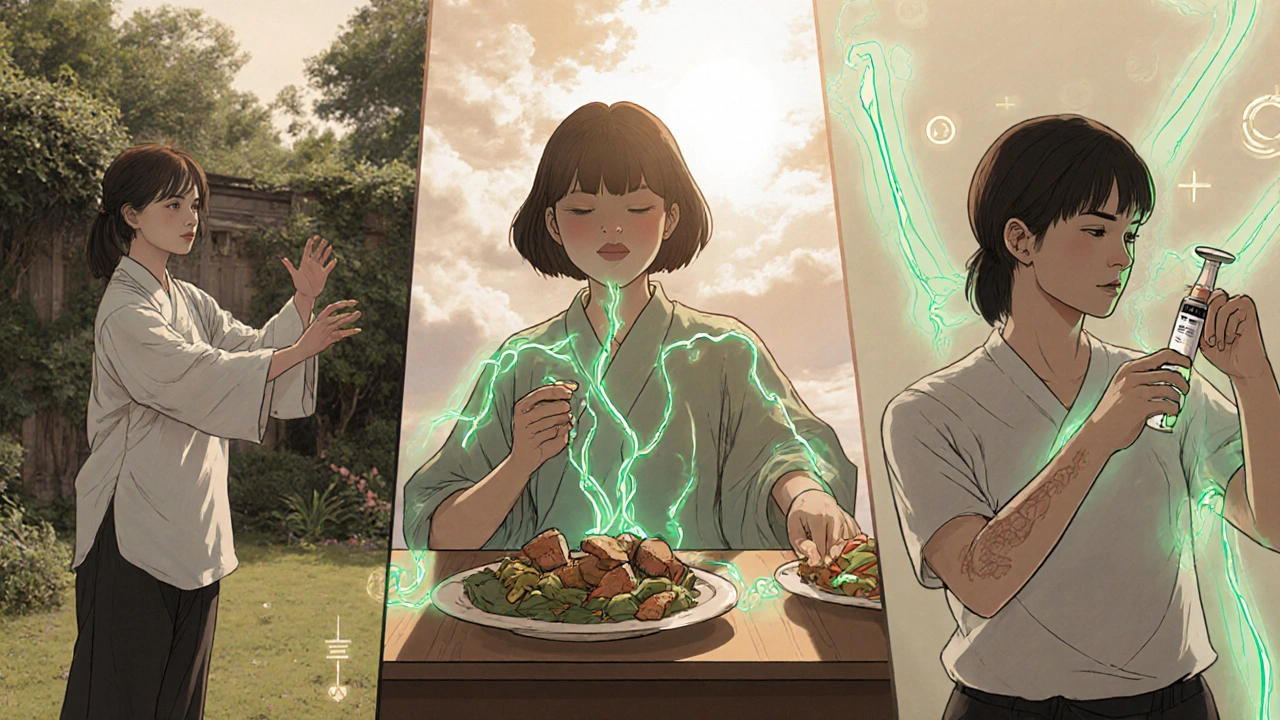
How to Protect Your Bones
There’s no magic bullet, but you can slow or even stop bone loss with a few proven steps:
- Get enough calcium and vitamin D. Aim for 1,200 mg of calcium daily from food or supplements. Sources: dairy, fortified plant milks, canned salmon with bones, kale. For vitamin D, take 800-1,000 IU daily. If your levels are low, your doctor may prescribe 2,000-5,000 IU.
- Move your body. Weight-bearing exercise like walking, stair climbing, or resistance training signals your bones to get stronger. Even 30 minutes three times a week helps. If joint pain is an issue, try swimming or tai chi.
- Reduce steroid use when possible. Work with your rheumatologist to find the lowest effective dose. Sometimes adding drugs like methotrexate or mycophenolate lets you cut steroids faster.
- Consider bone-protecting drugs. If you have osteoporosis or high fracture risk, bisphosphonates like alendronate or zoledronic acid can reduce fracture risk by 40-70%. Denosumab is another option. These aren’t for everyone-side effects exist-but for many lupus patients, they’re life-changing.
- Stop smoking and limit alcohol. Smoking cuts blood flow to bones. More than two drinks a day interferes with calcium absorption.
What Happens If You Do Nothing?
Osteoporosis doesn’t hurt until it’s too late. A spinal fracture can collapse your vertebrae without trauma-leading to chronic pain, height loss, and a hunched posture. A hip fracture often requires surgery and can end independence. One in four people over 50 who break a hip die within a year.
For lupus patients, recovery is harder. Inflammation slows healing. Steroids weaken muscles and increase infection risk after surgery. Many end up in long-term care. This isn’t inevitable. But ignoring bone health makes it far more likely.
What’s New in 2025?
Research is shifting. In 2024, a trial showed that a new biologic drug, anifrolumab, used for moderate-to-severe SLE, reduced steroid use by 30% over a year. Less steroid use = less bone loss. Another study found that lupus patients on newer DMARDs like belimumab had slower bone density decline than those on older regimens.
Doctors are also testing routine bone scans at diagnosis-not just after steroid use. Early detection means early intervention. Some clinics now pair lupus care with bone health specialists, creating a joint care plan.
Bottom Line
Lupus doesn’t just live in your skin or joints. It lives in your bones too. Whether you have discoid lupus or systemic lupus erythematosus, your bones are under siege-from inflammation, from medication, from inactivity. But you’re not powerless. You can test for bone loss. You can change your diet. You can move more. You can talk to your doctor about alternatives to long-term steroids. You can take medication to rebuild what’s been lost.
It’s not about living perfectly. It’s about living with awareness. One scan. One supplement. One walk. Those small steps add up. And they might keep you standing-strong and steady-for years to come.
Can discoid lupus cause osteoporosis even without systemic involvement?
Yes. Even though discoid lupus mainly affects the skin, the chronic immune inflammation it causes releases cytokines that circulate through the body and disrupt bone remodeling. Studies show patients with discoid lupus still have lower bone density than healthy individuals, especially if they take corticosteroids for flare-ups.
How often should lupus patients get a bone density scan?
The American College of Rheumatology recommends a DEXA scan at diagnosis if you’re over 50, have taken steroids for more than 3 months, or have other risk factors like kidney disease. After that, repeat every 1-2 years if you’re on long-term steroids or have low bone density. If your bones are normal and you’re not on steroids, you may only need a scan every 3-5 years.
Is vitamin D supplementation enough to prevent bone loss in lupus?
No. While vitamin D is essential for calcium absorption and bone health, it doesn’t counteract the bone-damaging effects of steroids or chronic inflammation alone. You need calcium too, plus weight-bearing exercise, and sometimes prescription bone medications. Vitamin D is a foundation-not a full solution.
Can I stop taking steroids to protect my bones?
Never stop steroids suddenly-they can cause life-threatening adrenal crisis. But you can work with your rheumatologist to reduce your dose gradually by adding other immunosuppressants like methotrexate or azathioprine. The goal is the lowest effective dose for the shortest time possible.
Do biologics like belimumab help protect bones?
Yes, indirectly. Biologics like belimumab and anifrolumab help control lupus activity without relying on high-dose steroids. By reducing steroid use, they lower one of the biggest drivers of bone loss. Some studies show slower bone density decline in patients using these drugs long-term.



Comments (11)
Ankita Sinha
I was diagnosed with discoid lupus last year and never even thought about my bones until my doctor mentioned it. I started taking vitamin D and walking every morning-just 20 minutes-and my joint pain actually improved. Who knew moving more could help so much?
Also, I switched to fortified almond milk and started eating canned salmon. Small changes, but I feel stronger already.
Kenneth Meyer
It’s wild how the body’s immune system, meant to protect us, ends up turning against itself in such quiet, systemic ways. Lupus doesn’t just attack skin or joints-it erodes the very scaffolding of our physical existence. Bone isn’t inert; it’s a living tissue constantly reshaped by inflammation, hormones, and chemical signals we barely understand.
Maybe osteoporosis in lupus isn’t just a side effect-it’s a mirror. A reflection of how deeply our internal wars leave scars we can’t see until we break.
Donald Sanchez
LMAO so prednisone is the real villain?? 😂 I’ve been on 10mg for 2 years and my bones feel like chalk. My doc just says ‘take calcium’ like that fixes everything. Nah fam. This is a scam. Big Pharma wants you dependent on steroids AND bisphosphonates. Double profit!
Also, DEXA scans? Bro, I got mine and the machine said ‘osteopenia’ like it was a bad Yelp review. 😭
Danielle Mazur
Have you considered that the rise in lupus diagnoses correlates with increased fluoride in drinking water and EMF exposure from 5G networks? The medical establishment refuses to acknowledge environmental triggers because they’re tied to pharmaceutical revenue streams.
My cousin’s bone density dropped 18% after her first steroid cycle. She’s now on a raw food, alkaline diet and refuses all pharmaceuticals. Her T-score improved by 1.3 in 14 months. Coincidence? I think not.
Freddy Lopez
There’s a quiet dignity in how the body endures. We treat lupus as if it’s a problem to be solved, but maybe it’s a teacher. It forces us to slow down, to listen, to care for the parts of ourselves we ignore-the bones, the lungs, the kidneys.
Perhaps the real question isn’t how to stop bone loss, but how to live gently enough that our bodies don’t have to fight so hard just to stay whole.
Brad Samuels
I’ve been living with SLE for 12 years. I lost my mom to a hip fracture at 62-she had lupus too. I got my first DEXA scan at 45. Osteopenia. I cried. But then I started swimming three times a week, took my vitamin D like it was oxygen, and switched to a rheumatologist who actually listens.
You’re not alone in this. And you’re not broken. You’re adapting. That’s strength.
Herbert Scheffknecht
Okay, but think about it-lupus is the ultimate paradox. Your immune system is screaming for help, but the only thing that quiets it makes your bones crumble. It’s like your body is trying to survive by setting itself on fire.
And then we wonder why people with chronic illness die younger? Because we’re not treating the system-we’re treating symptoms. We’re patching holes while the whole ship is sinking.
And don’t even get me started on how doctors treat women’s pain like it’s anxiety. ‘Oh, it’s just lupus.’ Like that’s an excuse to stop caring.
But hey, at least we got biologics now. Progress? Maybe. But I still feel like my bones are just collateral damage in a war no one’s winning.
Jessica Engelhardt
Why are we even talking about vitamin D when the real issue is that the CDC and WHO are pushing estrogen blockers in women over 40? It’s a population control tactic disguised as healthcare. Lupus is just the symptom. The disease is the system.
Also, calcium supplements are made from limestone-why do you think they’re so cheap? Because they’re not real nutrients. They’re fillers. Your bones need real food. Like bone broth. From grass-fed cows. Not factory farms.
Lauren Hale
For anyone new to this-don’t panic. Bone loss is scary, but it’s manageable. I’m 53, had discoid lupus for 15 years, and my DEXA scan last year showed improvement. I didn’t change everything overnight. I just added one thing: daily walking with my dog. Then I added calcium-rich greens. Then I talked to my doctor about my steroid dose.
You don’t need to be perfect. You just need to start. One step. One pill. One conversation. That’s enough.
Greg Knight
I’ve coached dozens of lupus patients through bone health, and here’s the truth: the biggest barrier isn’t the disease-it’s shame. Shame that you can’t run like you used to. Shame that you need meds. Shame that you feel like a burden.
But your body isn’t failing you. It’s adapting. And you? You’re still showing up. That’s not weakness. That’s courage.
Start small. A 10-minute stretch. A glass of fortified milk. A question to your rheumatologist. You’ve already won by reading this. Now take the next step. I believe in you.
rachna jafri
Western medicine is a joke. They give you steroids that turn your bones to dust, then sell you expensive pills to fix it. Meanwhile, in India, we’ve been using ashwagandha and turmeric for centuries to calm inflammation-no side effects, no corporate patents.
My aunt had discoid lupus and never took a single steroid. She drank warm milk with turmeric, walked barefoot on grass, and lived to 87. No fractures. No hospital stays. Just wisdom.
Stop trusting Big Pharma. Go back to the roots. Your bones will thank you.