Every year, half of all people taking medication for chronic conditions like high blood pressure, diabetes, or cholesterol don’t take it as prescribed. That’s not because they’re careless or lazy. It’s because the system is stacked against them. Skipping pills isn’t a choice-it’s often the only option left after cost, confusion, and complexity pile up. The real question isn’t why people forget their meds. It’s why we keep expecting them to remember in a system that makes it so hard.
Cost Is the Biggest Reason People Skip Medications
One out of every five new prescriptions is never picked up from the pharmacy. Why? Price. A 2023 survey by the American Medical Association found that 50% of patients say cost is their top barrier to taking medication. For many, choosing between insulin and groceries isn’t a hypothetical-it’s real. A month’s supply of some brand-name drugs can cost $300 or more. Even with insurance, copays can be $50 or higher for a single pill. People ration pills. They cut doses in half. They skip days. Some stop entirely. The CDC reports that 20% to 30% of new prescriptions go unfilled because of cost. This isn’t just about greed or profit-it’s about a system where medication is treated like a luxury, not a necessity.Too Many Pills, Too Many Times a Day
Imagine you’re on five different medications. One in the morning, one after lunch, one at dinner, one before bed, and another at 2 a.m. because your doctor said it’s “best for absorption.” Now add in a few supplements, vitamins, and over-the-counter painkillers. That’s not a treatment plan-it’s a full-time job. Research shows that for every extra pill a person takes, their chance of missing a dose goes up by 16%. When someone has to take a medication four times a day, only about 51% stick with it. But when it’s once daily? That jumps to 79%. It’s not magic. It’s math. Simpler regimens work. Combination pills-like a single tablet that combines blood pressure and cholesterol meds-cut adherence problems in half. Yet most doctors still prescribe separate pills because it’s easier for them, not better for the patient.Forgetting Isn’t Just About Memory
People say they forget. And yes, they do. But forgetting isn’t random. It’s predictable. A 2024 study found that 44% of diabetic patients over 59 reported forgetting doses as their main issue. But here’s what they didn’t say: they also didn’t know when to take it, what it was for, or how long it would take to work. Forgetting is often a symptom of deeper confusion. A patient might take their pill at breakfast one day, then at lunch the next because they never got clear instructions. Or they’re on a rotating shift job and their schedule changes every week. Their phone alarm goes off at 7 a.m., but they’re already at work. They skip it. Then they feel fine. So they keep skipping. The body doesn’t scream when you miss a dose-it just slowly falls apart over months. That’s why “I forgot” is rarely the whole story.Instructions That Are Impossible to Follow
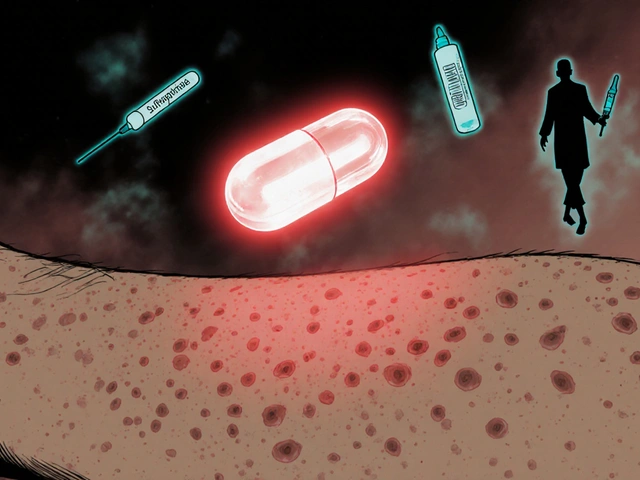
Ever tried reading the tiny print on an insulin pen? Or figured out how to use a complex inhaler without a demonstration? Many medication instructions are written for pharmacists, not patients. The font is too small. The diagrams are unclear. The language is full of medical jargon. One patient on Reddit shared how she overdosed twice because she couldn’t read the dosage markings on her insulin pen. Another said she stopped her blood thinner because the bottle said “take with food,” but she didn’t know what “with food” meant-did it mean right after eating? During? Thirty minutes later? No one told her. Health literacy isn’t just about reading. It’s about understanding. A 2024 study found that patients with low health literacy are 2.5 times more likely to miss doses. If you don’t understand why you’re taking a pill, you won’t stick with it.
Doctors Don’t Have Time to Explain
The average doctor’s visit lasts 15 to 20 minutes. In that time, they’re supposed to diagnose, prescribe, answer questions, update records, and refill prescriptions. Medication adherence? It’s the last thing on the list. A 2022 study found that only 1 in 5 patients receive any kind of structured counseling about how to take their meds. Most get a printed sheet with a list of names and times-and that’s it. No one checks if they understood. No one asks if they can afford it. No one says, “What’s your biggest problem with taking these?” And yet, studies show that when doctors spend just five extra minutes explaining why a medication matters and how to take it, adherence goes up by 25%. It’s not rocket science. It’s basic communication.Complex Schedules and Life Get in the Way
Life doesn’t stop for a pill schedule. Kids get sick. Work shifts change. Travel happens. Seniors forget where they put their pill organizer. People with depression or anxiety don’t have the energy to manage a dozen pills. A 2023 survey found that 78% of patients who missed doses said their daily routine made it hard to remember. One man in Halifax told me he works nights, sleeps days, and his meds are scheduled for 8 a.m., 1 p.m., and 8 p.m. He can’t take them at 8 a.m. because he’s asleep. He can’t take them at 8 p.m. because he’s just waking up. He skips. He feels guilty. He stops going to the doctor because he doesn’t want to be judged. This isn’t about discipline. It’s about design. The system doesn’t adapt to real life-it demands that real life adapt to it.Depression, Anxiety, and the Mental Load
It’s easy to blame patients for not taking their meds. But what if they’re depressed? Or overwhelmed? Or scared of side effects? A patient might skip their heart medication because they’re afraid it’ll make them dizzy. Or stop their antidepressant because they think it’s “not working yet.” These aren’t irrational fears-they’re real concerns, often unaddressed. The NICE guidelines show that 47% of nonadherence comes from doubts about whether the medicine is even necessary. And 38% comes from fear of side effects. These aren’t minor worries. They’re deeply personal. When a patient feels like their doctor dismissed their fears, they stop talking. And they stop taking the pills.
Pharmacies Can Help-But Most Don’t
Pharmacists are the most accessible healthcare professionals. They see patients every time they refill a prescription. Yet only 32% of small pharmacies have formal adherence programs. Meanwhile, big pharmacy chains and insurance companies are rolling out automated refill systems, 90-day mail-order deliveries, and synchronized refills-all of which improve adherence by 15% to 20%. One simple trick: if all your meds are due on the same day each month, you’re far more likely to remember. But most patients still get staggered refill dates-meaning they have to go to the pharmacy three or four times a month. That’s not just inconvenient. It’s expensive. It’s time-consuming. And for people without a car or reliable transit, it’s impossible.What Actually Works
The best solutions don’t rely on patients being perfect. They change the system. Here’s what helps:- Combination pills-one tablet instead of three.
- Once-daily dosing-even if it costs a little more.
- 90-day mail-order refills-cuts trips to the pharmacy in half.
- Medication synchronization-all prescriptions due on the same day.
- Pharmacist check-ins-a 10-minute call every month to ask, “What’s hard about taking these?”
- Clear, simple instructions-written in plain language, with pictures.
It’s Not About Willpower
We keep telling patients to “be responsible.” But responsibility isn’t the problem. The system is. People aren’t failing because they don’t care. They’re failing because the rules are written for a world that doesn’t exist anymore. We have pills that last a week, but still ask people to take them daily. We have apps that can remind them, but don’t teach them how to use them. We have doctors who mean well, but no time to listen. Until we fix the design-not the patient-we’ll keep seeing the same results: missed doses, hospital visits, and preventable deaths. The solution isn’t more reminders. It’s fewer pills. Simpler schedules. Better conversations. And a system that meets people where they are.Why do people skip their medications even when they know it’s important?
People don’t skip meds because they’re irresponsible. They skip because they can’t afford them, don’t understand how to take them, are overwhelmed by too many pills, or fear side effects. When the system makes it hard to take medication, skipping becomes the only practical choice-even if they know it’s risky.
Is forgetting pills just a memory problem?
No. Forgetting is often a sign of deeper confusion. Many patients don’t know why they’re taking a pill, when to take it, or what it’s supposed to do. Without that understanding, even the best reminder app won’t help. It’s not about memory-it’s about clarity.
How does dosing frequency affect adherence?
The more times a day you have to take a pill, the less likely you are to remember. For once-daily medications, adherence is about 79%. For medications taken four or more times a day, it drops to 51%. Simplifying the schedule-like switching to a long-acting version-can double adherence rates.
Can pharmacists really help with medication adherence?
Yes. Pharmacists are often the only healthcare provider patients see regularly. Simple actions like synchronizing all prescriptions to one refill date, offering 90-day supplies, or calling to check in can improve adherence by 15% to 20%. Yet most small pharmacies don’t offer these services.
What’s the biggest mistake doctors make about medication adherence?
Assuming patients understand their treatment. Most doctors hand out a prescription and assume the patient knows why they need it, how to take it, and what side effects to watch for. But without a clear, patient-centered conversation, that assumption leads to confusion-and missed doses.
Are there new technologies that help with medication adherence?
Yes. Smart pill bottles, AI tools that predict who’s at risk of skipping doses, and long-acting injectables (like monthly shots for schizophrenia) are improving adherence. But tech alone doesn’t fix the problem. It only works when paired with support, education, and simpler regimens.
Why do older adults struggle more with medication adherence?
Older adults often take more medications, have lower health literacy, and may have memory or vision issues. But the bigger problem is complexity. A 75-year-old might be on 8 different pills with different times, instructions, and refill schedules. That’s not just hard-it’s impossible without support.
Can medication adherence be improved without spending more money?
Yes. The cheapest fix is simplifying prescriptions: fewer pills, once-daily dosing, combination drugs. Better communication from doctors and pharmacists costs little but improves outcomes dramatically. The real cost is in ignoring the problem-hospitalizations, ER visits, and deaths from preventable causes cost the system hundreds of billions.