Statin Nocebo Effect Checker
How Likely Is Your Symptom Due to the Nocebo Effect?
Based on the SAMSON trial (2021), 90% of reported statin side effects were caused by expectation rather than the drug itself. Answer these questions to see if your symptoms might be nocebo.
What Does This Mean?
In the SAMSON trial, symptoms were equally bad on placebo (15.4) and statins (16.3), but dropped to 8.0 with no pills. This means 90% of side effects were caused by expectation.
Key Takeaway:
If you restart statins, you can likely tolerate them. The SAMSON trial showed 50% of patients who restarted after understanding nocebo effect experienced no symptoms.
When people stop taking statins, it’s often because they feel worse-muscle aches, fatigue, weakness. But what if those symptoms aren’t really from the drug? What if they’re from expectation? That’s the startling insight from one of the most important studies in modern cardiology: the SAMSON trial. And it’s changing how doctors talk to patients about statins-forever.
What the SAMSON Trial Really Found
In 2021, researchers in the UK ran a 12-month experiment with 60 people who had quit statins because of side effects. These weren’t just mild complaints-they were patients who had tried multiple statins and given up. The study’s design was simple but brilliant. Each person got 12 bottles over a year: four with atorvastatin (20 mg), four with placebo pills, and four empty (no pill at all). They didn’t know which was which. Every day, they logged their symptoms on a smartphone app using a scale from 0 to 100. The results? Painful clarity. Symptom scores during placebo months averaged 15.4. During statin months? 16.3. Barely different. And during the no-pill months? Just 8.0. That means when people thought they were taking a statin, their symptoms were just as bad as when they were actually taking one. But when they took nothing at all? Symptoms dropped sharply. The nocebo ratio? 0.90. That means 90% of the side effects people blamed on statins were actually caused by the belief that they were taking a statin-not the drug itself. This isn’t about being "imaginary." These people weren’t faking it. Their pain was real. But the source wasn’t the medication. It was their mind.Why Statins Are Different
Most drugs don’t trigger this kind of reaction. Take blood pressure pills or antidepressants. In blinded trials, side effects in the placebo group rarely match the drug group. But statins? They’re an outlier. Why? Because of the noise. For decades, patients have heard warnings: "Statins can cause muscle pain." TV ads, pamphlets, online forums, even doctor’s office posters-all hammer this message. A 2022 survey found that 78% of statin users recalled hearing about muscle side effects before even starting the drug. That’s not an accident. It’s a marketing legacy from the 1990s and early 2000s, when drug companies overemphasized risks to avoid lawsuits. The result? A self-fulfilling prophecy. People start taking statins. A week later, they feel a twinge in their thigh. They think: "It’s the statin." And suddenly, that twinge becomes aching legs, fatigue, even nausea. The brain amplifies normal sensations because it’s been primed to expect harm. Compare that to a 2021 meta-analysis of 18,192 patients in randomized trials. In those studies, where patients didn’t know if they were on statins or placebo, there was no difference in muscle symptoms. But in observational studies-where patients knew they were on statins-up to 20% reported muscle pain. The difference? Expectation.Real People, Real Stories
The SAMSON trial didn’t just produce numbers. It changed lives. One participant, a 68-year-old man who had stopped statins after two months of leg pain, saw his symptom log. He realized: his pain was just as bad on placebo as on the real drug. He restarted atorvastatin. Six months later, his LDL dropped from 150 to 72. No pain. No complaints. On Reddit, threads like r/Cardiology and r/Pharmaceuticals are full of similar stories. One user wrote: "I thought I was intolerant. Then I saw my data. Placebo and statin were identical. I restarted. 10 months in-no issues." Another: "I cried when I saw the graph. All that fear… for nothing." But not everyone reacts this way. Some patients had real, measurable muscle damage-elevated CPK levels, confirmed by blood tests. Those cases are rare. About 1 in 10,000 for muscle injury, and less than 1 in a million for rhabdomyolysis, according to the Mayo Clinic. The SAMSON trial specifically excluded these patients. Their pain is pharmacological. But for the vast majority? It’s psychological.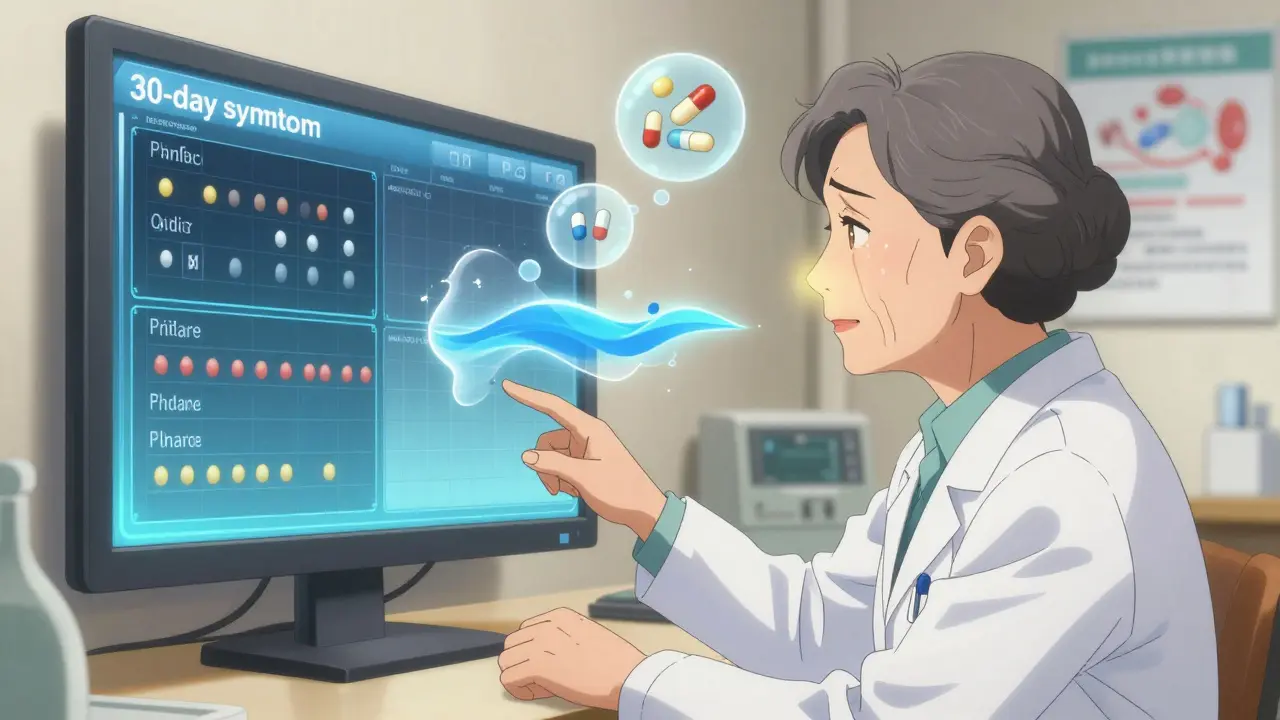
What This Means for Your Health
Statins save lives. They cut heart attacks, strokes, and death risk by 25% to 35% in people with high cholesterol or heart disease. But 40% to 70% of people stop taking them within a year. Why? Because they think the side effects are worse than the risk. That’s a massive public health failure. The U.S. loses an estimated $11.2 billion a year in preventable heart events because people quit statins over perceived side effects. And it’s mostly not the drug’s fault. If you’ve stopped statins because of muscle pain, you’re not alone. And you’re not weak. But here’s the truth: if you’re one of the 90%, you might be able to take them again. Not because you’re "stronger"-but because you now understand how your mind works.How Doctors Are Changing Their Approach
Cardiologists aren’t ignoring symptoms. They’re redefining them. The American College of Cardiology now recommends n-of-1 trials for patients with suspected statin intolerance. That means: a simple, low-cost test. Three phases: placebo, statin, no-pill. Track symptoms daily. Show the patient the data. Let them see for themselves. Clinics in the UK, Canada, and the U.S. are adopting this. A 2022 survey of 127 cardiologists found those who used this method saw 48.7% of patients restart statins. Those who didn’t? Only 22.1%. The key? Communication. Not dismissing. Explaining. Showing. A 2023 American Heart Association CME module trains doctors to say: "Your body isn’t rejecting the drug. Your brain is reacting to the idea of it. Let’s test that." And it works. One 72-year-old woman in Halifax, who had quit statins three times, restarted after seeing her symptom log. She’s now on rosuvastatin 5 mg. Her cholesterol is normal. Her legs feel fine. She says: "I thought I was broken. Turns out, I was just scared."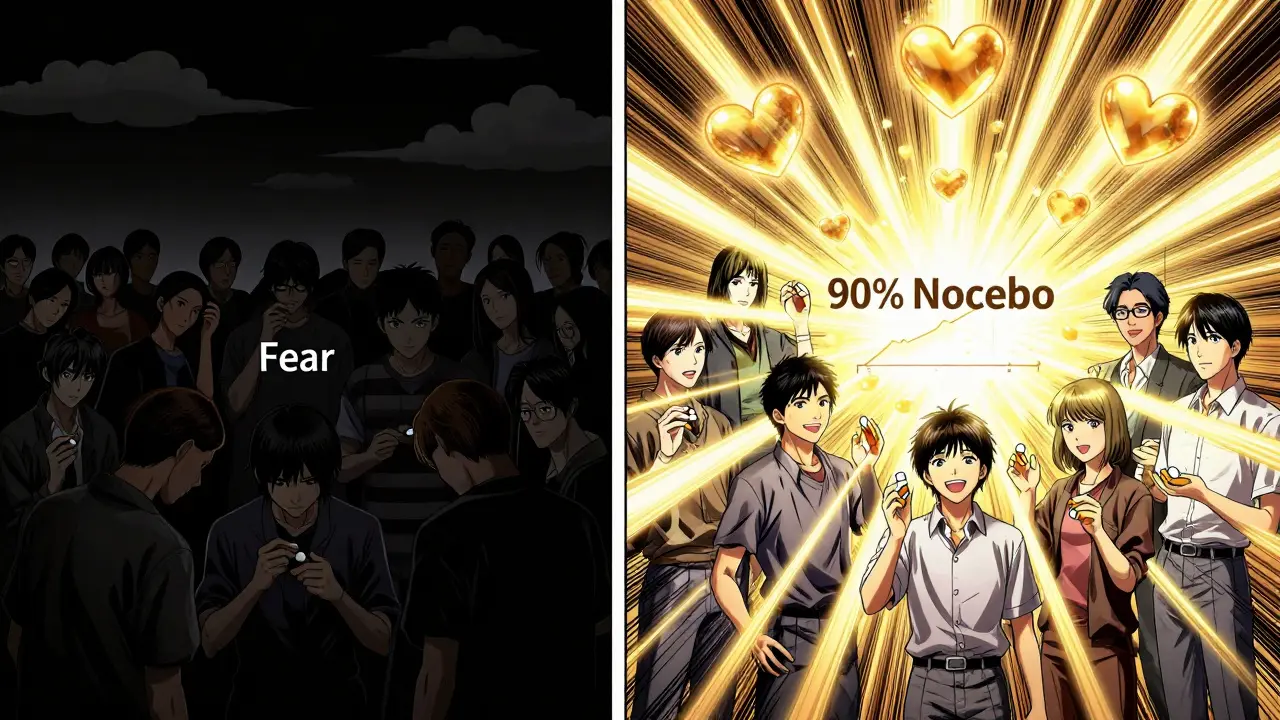
What to Do If You’re Stopped on Statins
If you’ve quit statins because of side effects, here’s what to do next:- Don’t assume it’s the drug. Muscle aches are common. They happen from walking too far, lifting heavy boxes, or even stress. Statins don’t cause them more than anything else.
- Ask your doctor about the nocebo effect. Bring up the SAMSON trial. Ask: "Could this be in my head?"
- Request a simple symptom tracking trial. Use a free app like Apple Health or Google Fit. Log daily symptoms for a month without any pills. Then try a placebo pill (your doctor can prescribe one). Then try a low-dose statin. Compare the patterns.
- Start low. If you restart, begin with 5 mg of rosuvastatin or 10 mg of atorvastatin. Most people tolerate this fine.
- Give it time. Symptoms from nocebo usually peak in the first week and fade by day 14. If they don’t, talk to your doctor. But if they do? You’ve just proven it wasn’t the drug.
The Bigger Picture
This isn’t about blaming patients. It’s about fixing a system that told everyone statins were dangerous. It’s about recognizing that fear can be more harmful than medicine. The nocebo effect isn’t unique to statins. It happens with vaccines, antibiotics, even caffeine. But statins are the clearest example we have. Because the data is undeniable. The science is solid. And the stakes? Life or death. If you’re at risk for heart disease, skipping statins because of fear might be the most dangerous choice you make. But if you understand this? You might just live longer.Is the nocebo effect real, or is it just "in my head"?
The nocebo effect is absolutely real. It’s not imaginary. It’s a measurable, biological response triggered by expectation. When you believe a pill will cause side effects, your brain releases stress chemicals like cortisol and adrenaline. These can cause real physical symptoms-muscle tension, fatigue, nausea. The SAMSON trial proved this by showing identical symptom patterns between statin and placebo. The pain is real. The cause is psychological, not pharmacological.
Can I still have real statin side effects?
Yes-but they’re extremely rare. True statin-induced muscle injury (elevated CPK, myopathy) occurs in about 5 out of 10,000 people per year. Rhabdomyolysis, the most severe form, affects fewer than 1 in a million. These are confirmed by blood tests and clinical signs. The SAMSON trial excluded these patients. If you’ve had a blood test showing CPK levels 5x higher than normal after starting statins, your symptoms may be real. But if you’ve never had testing, and you only feel muscle aches, it’s far more likely to be the nocebo effect.
Why do statins cause more nocebo effects than other drugs?
Because of how they’ve been marketed. For decades, statin ads, pamphlets, and even doctor’s warnings focused heavily on muscle pain. Patients were told, "You might feel achy," over and over. This created a powerful mental association. Other drugs don’t have this level of public messaging. A 2022 study found 78% of statin users recalled side effect warnings before starting-compared to under 20% for most other medications. The fear was planted before the pill was even taken.
If I restart statins, will the pain come back?
Not necessarily. In the SAMSON trial, 50% of patients who restarted statins after seeing their symptom data reported no return of symptoms. The key is knowing the truth: your symptoms aren’t caused by the drug. When you stop expecting pain, your brain stops creating it. Start with a low dose. Track your symptoms daily. Most people find symptoms fade within 10-14 days. If they don’t, talk to your doctor-but don’t assume it’s the statin.
Should I avoid statins if I’m worried about side effects?
No-not if you’re at risk for heart disease. Statins reduce your risk of heart attack or stroke by up to 35%. The risk of serious side effects is less than 0.1%. The risk of not taking them? Much higher. If you’re worried, ask your doctor about a nocebo test. Track your symptoms. Compare placebo and statin. You might be surprised. You might find you can take them safely. And you might save your life.